Principles of Implant Occlusion: Part 3 – Recommendations for Fixed Full-Arch Implant Prostheses
With the high success rates of modern implantology, edentulous patients have the opportunity to improve their quality of life and benefit from the advantages of a removable implant overdenture or a fixed implant-supported prosthesis. In the literature, fixed full-arch implant restorations have been shown to have many advantages over removable implant-supported prostheses, including greater masticatory force and efficiency, higher satisfaction rates, less maintenance, greater bone maintenance and superior prosthesis success rates.1, 2, 3, 4
A fixed full-arch implant prosthesis is usually defined as an FP-3 prosthesis.5 This type of prosthesis replaces the clinical crown of the missing teeth and utilizes a pink-colored material such as acrylic, porcelain or zirconia to replicate the soft tissue. The fixed full-arch implant prosthesis was originally fabricated as a “hybrid” prosthesis, consisting of a metal substructure with denture teeth and acrylic. However, this type of prosthesis resulted in a high incidence of maintenance issues and complications, such as excessive wear or debonding of the denture teeth.6
To eliminate these complications, advancements in technology allowed for the fabrication of a porcelain-metal prosthesis. This type of restoration also exhibited many complications, including a high incidence of porcelain fracture, as well as difficulty in achieving a passive fit of the prosthesis. Recently, monolithic zirconia has been introduced to the profession with great success (BruxZir® Solid Zirconia Full-Arch Implant Prosthesis). This prosthesis has superior strength, very low fracture probability and excellent antagonistic wear characteristics7,8 The BruxZir Full-Arch Implant Prosthesis has outstanding esthetics and provides a solution to the disadvantages of the prior types of prostheses.
REHABILITATING THE FULLY EDENTULOUS ARCH
To optimize the longevity of a completely implant-supported full-arch prosthesis, the correct occlusal scheme is of paramount importance. Unfortunately, there is significant conflict within the dental literature regarding implant occlusion recommendations. Most occlusal concepts utilized in implant dentistry have evolved via complete dentures and fixed tooth-supported prostheses. Currently, there are no controlled studies on the ideal occlusion for fixed implant-supported prostheses. Thus, there exists no accepted consensus on the ideal occlusal scheme for patients.
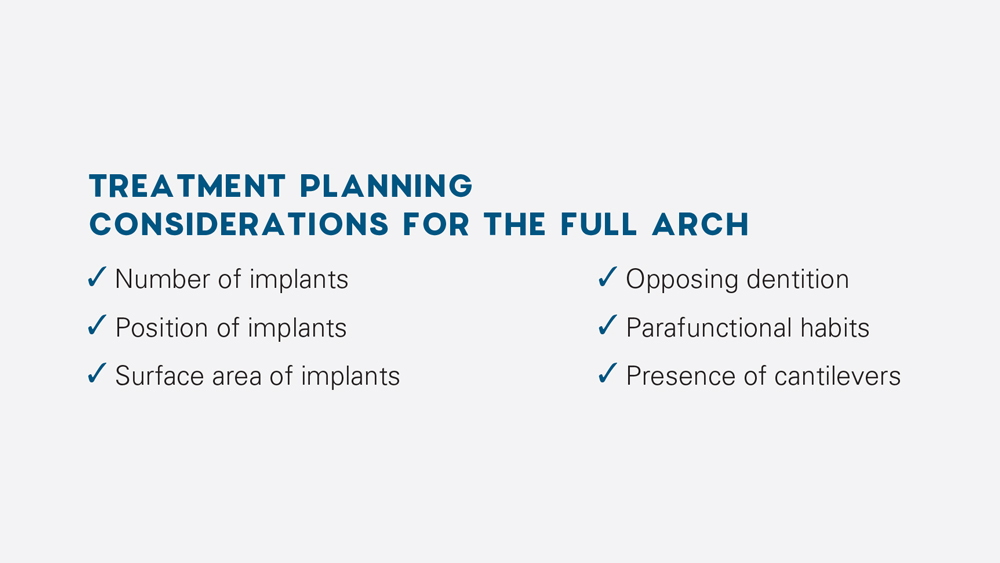
There are many variables when rehabilitating a fully edentulous arch with dental implants. Treatment planning is of the utmost importance and the following must be taken into consideration: the number, position and surface area of implants; opposing dentition; parafunctional habits; and presence of cantilevers.
The profession is in need of a decision tree for determining the type of occlusion to be used for fully implant-supported prostheses. In the literature, there exist three accepted and recognized ideal occlusal schemes for full-arch restorations with respect to functional and excursive positions of the mandible: bilateral balanced, group function, and mutually protected occlusion.
1a
2a

1c

1d
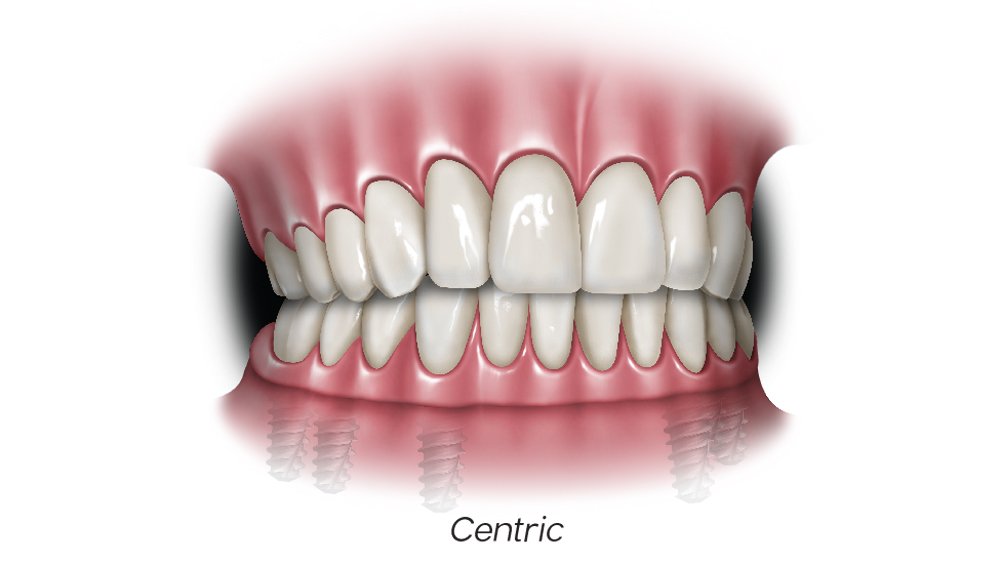
Figures 1a–1d: In bilateral balanced occlusion, in centric relation, anterior and posterior simultaneous contact should be present (a). Upon protrusive movement, bilateral simultaneous contacts are present (b). Posterior contacts are present on working and balancing sides during right lateral excursion (c, d).
I. BILATERAL BALANCED OCCLUSION
Bilateral balanced occlusion is defined as simultaneous, anterior and posterior occlusal contact in centric and eccentric positions. This occlusal scheme is mainly utilized with complete dentures, in which contact on the nonworking side prevents tipping of the prosthesis. Balanced occlusion is rarely seen in natural dentition with normal periodontium unless advanced and extensive attrition is present.
For full-arch implant restorations, this occlusal scheme is used only when one arch is restored with a conventional denture or an RP-5, which is a soft-tissue supported overdenture.
Lingualized Occlusion (Medial-Positioned)
Lingualized occlusion is a type of bilateral balanced occlusion where the maxillary lingual cusps articulate with the mandibular occlusal surfaces in centric and all excursive movements of the mandible. This occlusal scheme was first described by Dr. S. Howard Payne in 1941, then by Dr. Earl Pound, and further modified by Dr. Carl E. Misch in 1988.9 Lingualized occlusion maintains the esthetics and advantages of the anatomic form of the teeth (maxilla), while maintaining the mechanical freedom of nonanatomic teeth (mandible).
II. GROUP FUNCTION OCCLUSION
Group function, also termed unilateral balanced occlusion, is defined as simultaneous contact between multiple teeth on the working side during excursive movement of the mandible. This type of occlusion was first described by Dr. Clyde Schuyler, who determined that nonworking side contacts were traumatic to the dentition, resulted in neuromuscular disturbances, accelerated periodontal breakdown and resulted in excessive attrition.10
Group function is accomplished by having working side contacts and no nonworking side contacts, thus preventing excessive wear of the centric holding cusps and maintaining occlusion. In order to transmit lateral pressures to posterior teeth instead of the canine, this occlusion is used primarily with compromised canines.
III. MUTUALLY PROTECTED OCCLUSION
Mutually protected occlusion — also termed canine-protected, cuspid-rise or organic occlusion — is an occlusal scheme in which the anterior teeth protect the posterior teeth in protrusive movements by keeping them out of contact with the opposing dentition. The posterior teeth protect the anterior teeth in centric relation, and the canines protect the incisors and posterior teeth during lateral excursive movements. This occlusal scheme is based on the concept that the canine is a crucial element of occlusion, avoiding heavy lateral pressures on posterior teeth. Studies have shown that two-thirds of the temporalis and masseter muscles do not contract when posterior teeth do not occlude.11
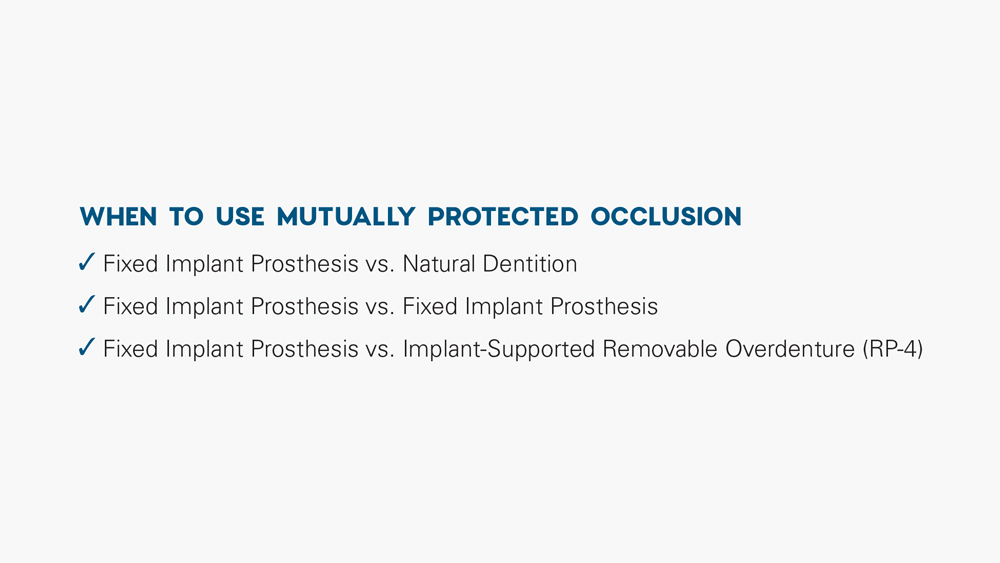
This occlusal scheme is used when the full-arch implant restoration opposes an arch with natural dentition or that is restored with a fixed implant prosthesis or an RP-4, which is an implant-supported overdenture.
Additionally, with a full-arch fixed implant prosthesis, the following should be integrated into the occlusal scheme: bilateral stability in centric (habitual) occlusion; wide freedom in centric (habitual) occlusion; narrow occlusal table; minimal cusp height; evenly distributed occlusal contacts and forces; no interferences between the retruded position and centric (habitual) position; and smooth and even lateral excursive movements without working or nonworking interferences.12
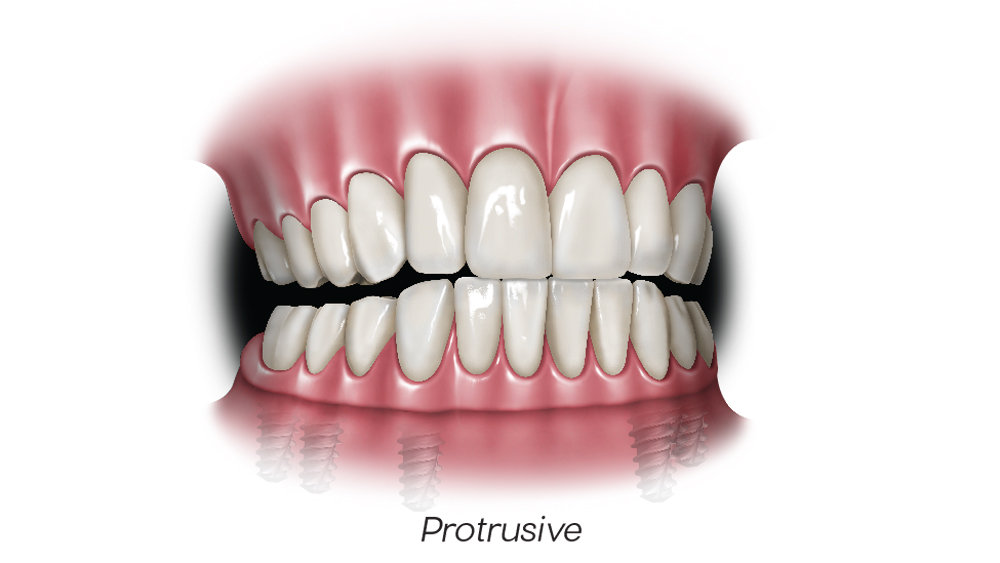

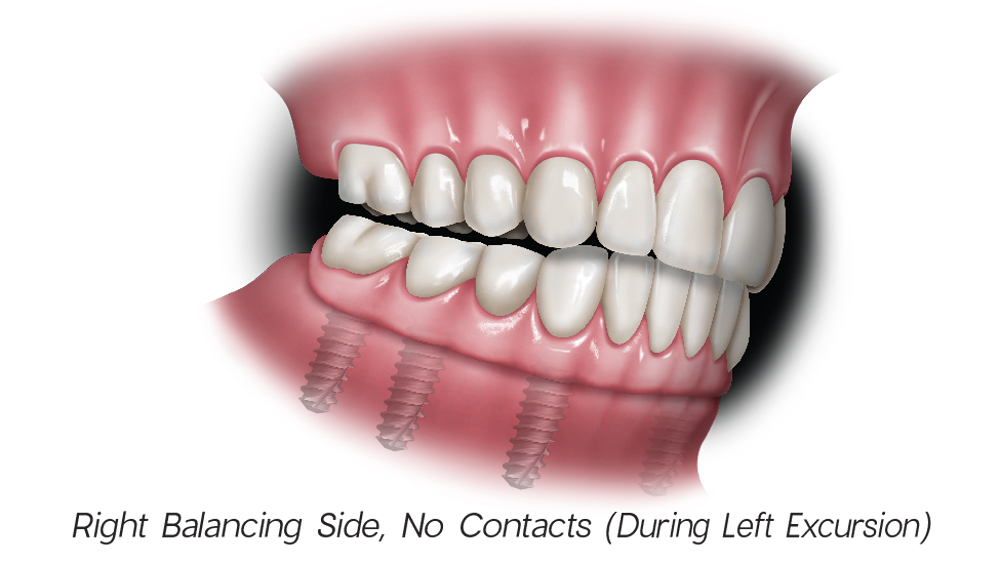
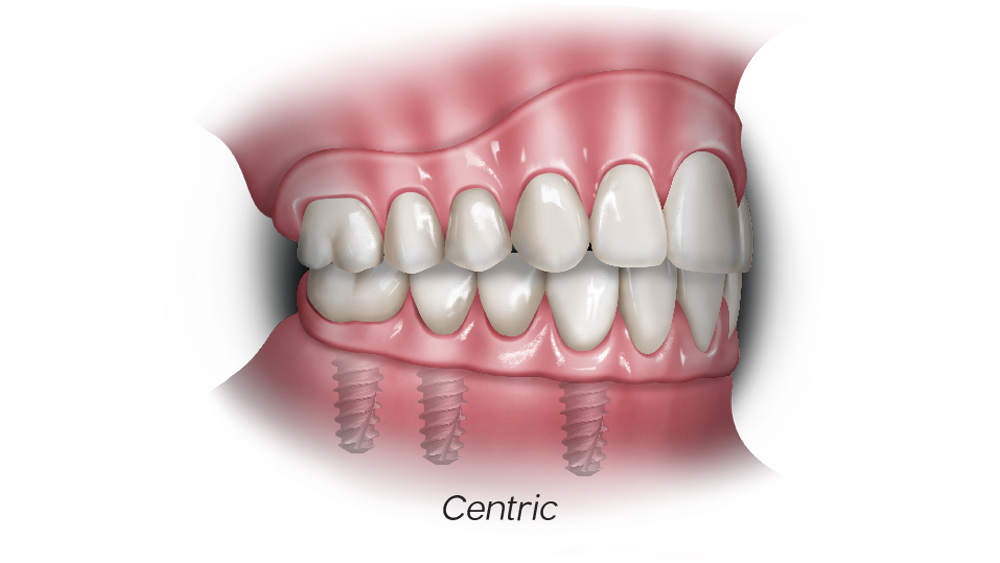
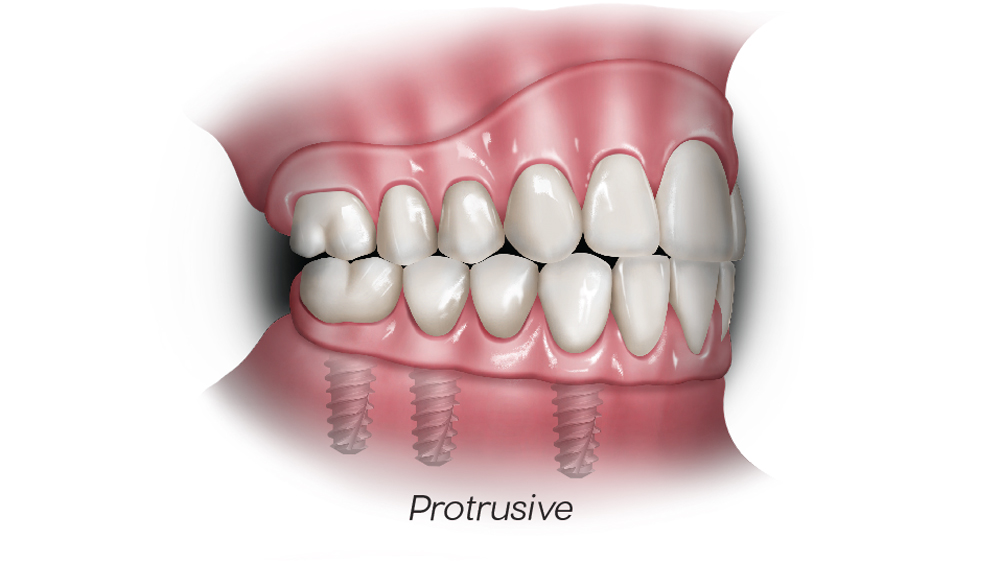
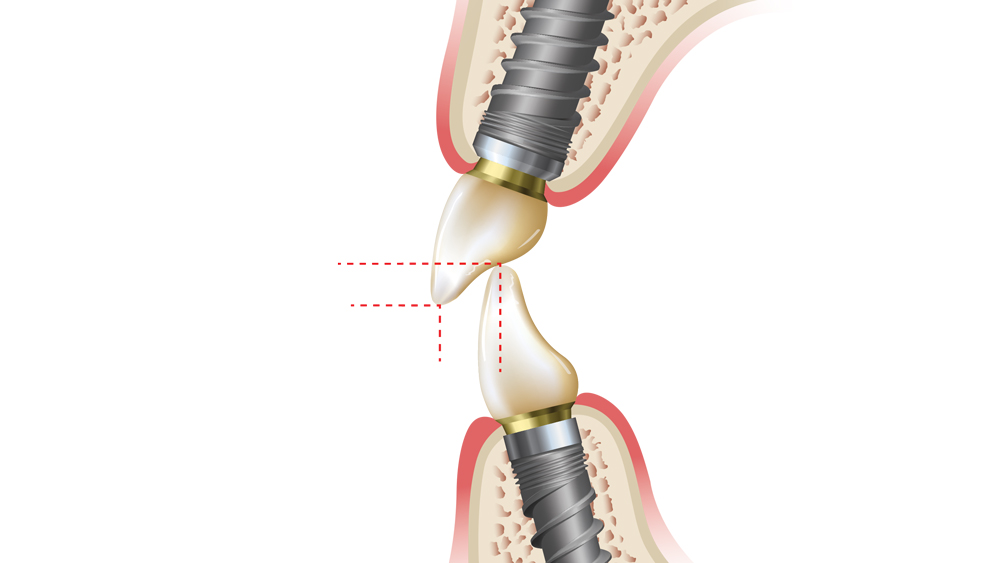
Figures 2a–2d: In mutually protected occlusion, the posterior teeth protect the anterior teeth in centric relation (a); the anterior teeth protect the posterior teeth in protrusive movements by disoccluding them, which will result in minimizing damaging lateral forces on the posterior teeth (b); and the canines protect the incisors and posterior teeth during lateral excursive movements (c, d).
With full-arch implant prostheses, the correct occlusal scheme is critical to decreasing morbidity and increasing prosthesis longevity. A poorly designed occlusal scheme will lead to biomechanical stress and strain on the underlying bone, which can cause biological and mechanical complications. These biomechanical overloads may lead to early or late implant failure, early crestal bone loss, screw loosening or fracture, an uncemented prosthesis, or prosthesis fracture.13
THE PRINCIPLES OF IMPLANT-PROTECTED OCCLUSION
To minimize the possibility of occlusal-related issues, Dr. Misch developed the concept of implant-protected occlusion (IPO), which helps to minimize the possibility of overload on the implant prosthesis and crestal bone. In addition to the occlusal scheme recommendations provided above, adhering to the following IPO principles can help reduce the biomechanical stress on the implant interface and maximize the success of the full-arch prosthesis:
IPO principles can help reduce the biomechanical stress on the implant interface and maximize the success of the full-arch prosthesis.
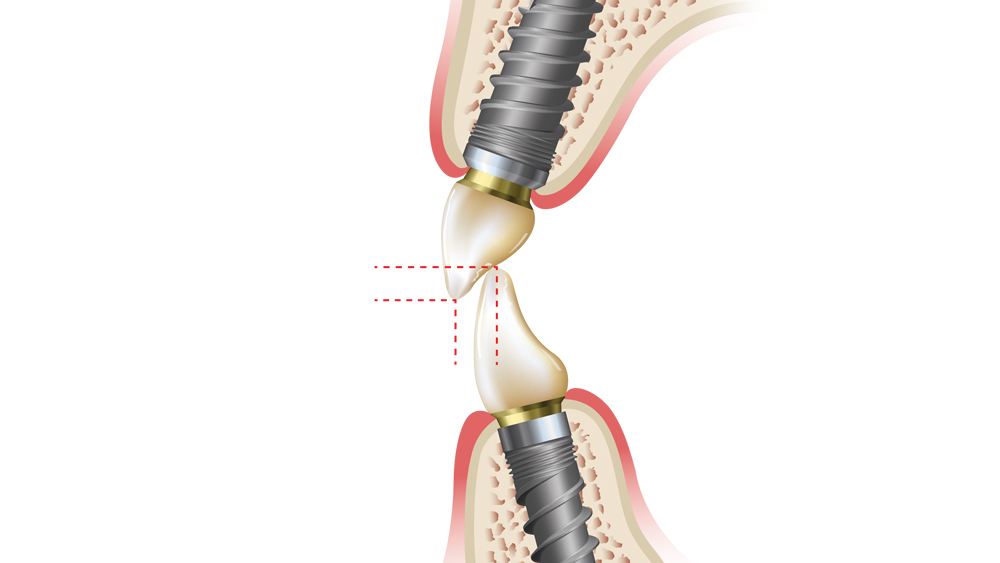
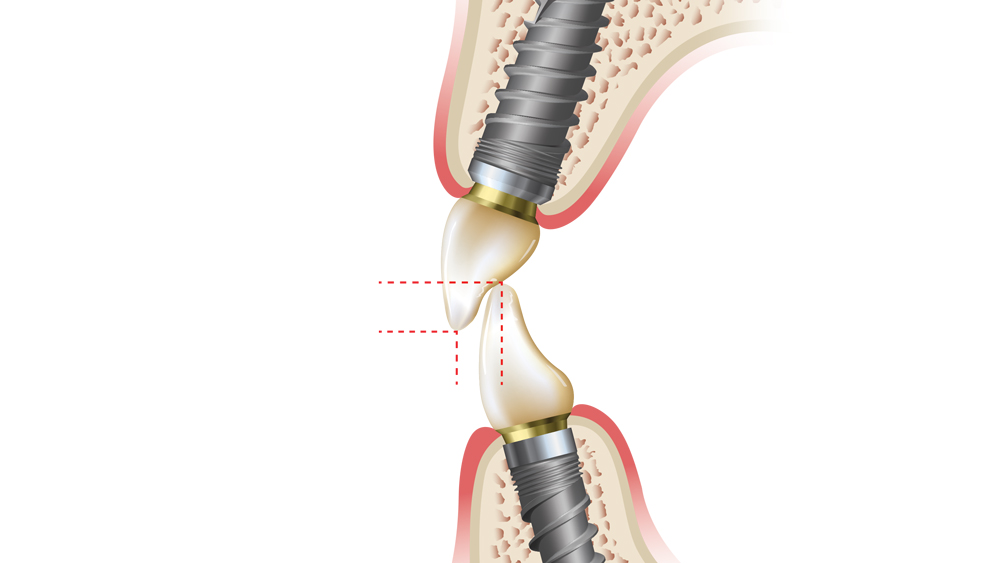
1. Ideal Implant Position — With a full-arch prosthesis, there exist key implant positions that are crucial to reduce force. The two most important positions are the canine and first molar, as both the magnitude and direction of the force is increased at these arch positions. Additionally, an implant positioned in the incisor area should be utilized to minimize an anterior cantilever effect.
2. Increased Implant Surface Area — Ideally, the implant surface area, which includes the number of implants and diameter of the implant bodies, should be increased, especially when the opposing occlusion is natural teeth or there exist parafunctional habits. A prosthesis with compromised implant surface area will lead to increased stress and strain, and possible biomechanical overload.
3. Minimized Cantilevers — Because of the pneumatization of the maxillary sinus and mandibular posterior bone loss, cantilevers are often utilized in full-arch implant prostheses to replace the first molar in the maxilla or mandible. Cantilevers act as force magnifiers, and the presence of cantilevers will lead to tensile forces, which increase the stress on the implant and the prosthesis. The destructive nature of cantilevers has been shown to result in peri-implant bone loss and prosthesis failure.14,15
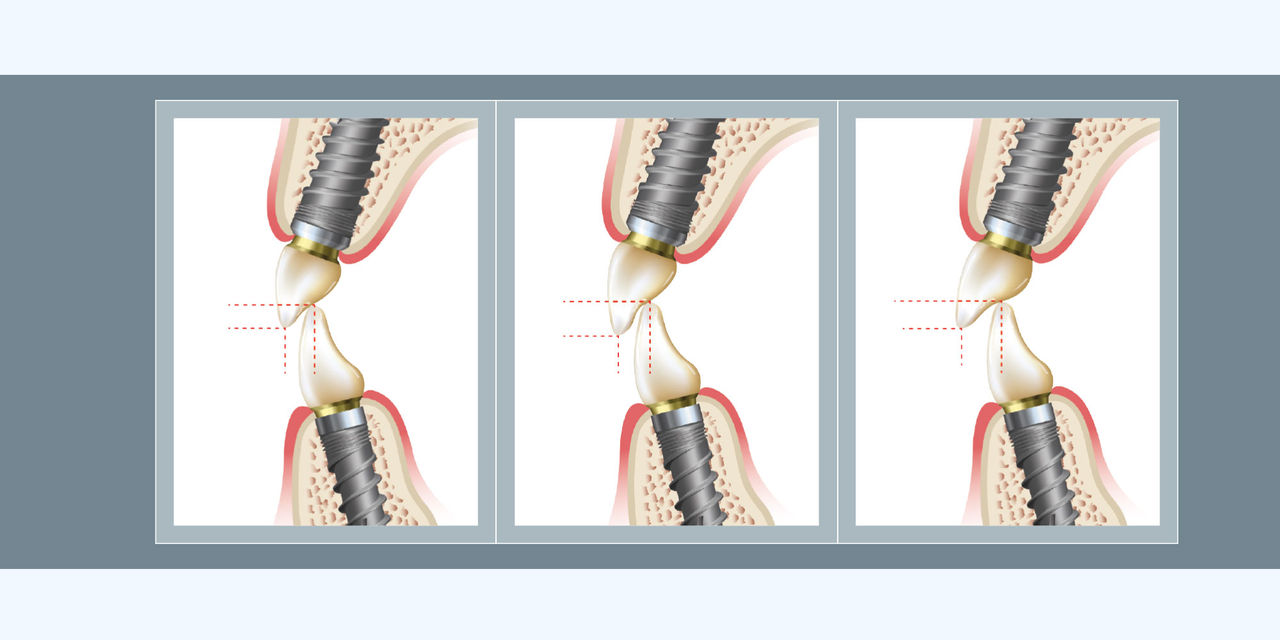
Figures 3a–3c: Shown is the interrelationship between vertical and horizontal overlap of the anterior teeth. To make the anterior guidance shallow, either decrease the overbite (from b to a) or increase the overjet (from b to c).
4. Shallow Anterior Guidance — With a fixed full-arch implant prosthesis, the anterior guidance should remain shallow. The steeper the incisal guidance, the greater the resultant force on the anterior segment. Drs. Lawrence Weinberg and Bernard Kruger stated that for every 10-degree increase in incisal guidance, a 30 percent increase in force to the anterior segment will result. Additionally, increased anterior guidance will result in a higher possibility of posterior contacts, which lead to greater muscle activity.16
5. Occlusal Guard — With an implant-supported prosthesis, there exists no protective feedback system (i.e., proprioception), leading to biting forces that are greater in comparison to those exerted by natural dentition. Additionally, patients are less aware of premature contacts, which may result in biomechanical overload. A full-arch implant patient will benefit from an occlusal guard, especially if parafunctional habits are present.
CONCLUSION
Occlusion plays a major role in the functional and biological aspects of the full-arch implant-supported prosthesis. The specific occlusal schemes discussed here are generalized recommendations for ideal conditions and should be modified appropriately in the presence of negative individual clinical determinants with regard to implant position, implant number, anterior-posterior spread, skeletal relationship, occlusal vertical dimension, amount of cantilever, esthetic occlusal plane orientations, and lip support.
The most common complications with full-arch implant prostheses are related to biomechanical overload, which may result in crestal bone loss, screw loosening or fracture, an uncemented prosthesis or implant failure. It is paramount that the concept of implant-protected occlusion be integrated into reducing force factors. Therefore, controlling and maintaining occlusion is imperative in reducing mechanical and biological complications, thus increasing the longevity of the prosthesis.
References
- ^ Kern JS, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016 Feb;27(2):174-95.
- ^ Wright PS, Glantz PO, Randow K, Watson RM. The effects of fixed and removable implant-stabilized prostheses on posterior mandibular residual ridge resorption. Clin Oral Implants Res. 2002 Apr;13(2):169-74.
- ^ Castillo-Oyagüe R, Suárez-García MJ, Perea C, Río JD, Lynch CD, Gonzalo E, Torres-Lagares D, Preciado A. Validation of a new, specific, complete, and short OHRQoL scale (QoLFAST-10) for wearers of implant overdentures and fixed-detachable hybrid prostheses. J Dent. 2016 Jun;49:22-32.
- ^ Müller F, Hernandez M, Grütter L, Aracil-Kessler L, Weingart D, Schimmel M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: a cross-sectional multicenter study. Clin Oral Implants Res. 2012 Feb;23(2):144-50.
- ^ Misch CE. Contemporary implant dentistry. 3rd ed. St. Louis: Mosby; 2007.
- ^ Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29 Suppl 3:197-212.
- ^ Stober T, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehabil. 2014 Apr;41(4):314-22.
- ^ Carames J, Tovar Suinaga L, Yu YC, Pérez A, Kang M. Clinical advantages and limitations of monolithic zirconia restorations full arch implant supported reconstruction: case series. Int J Dent. 2015:392496.
- ^ Misch CE. Dental implant prosthetics. 2nd ed. St. Louis: Mosby; 2014.
- ^ Schuyler CH. Factors of occlusion applicable to restorative dentistry. J Prosthet Dent. 1953;3(6):772-82.
- ^ Williamson EH, Lundquist D. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983 Jun;49(6):816-23.
- ^ Misch CE. Occlusal considerations for implant-supported prostheses: implant-protective occlusion. In: Misch CE, editor. Dental implant prosthetics. 2nd ed. St. Louis: Mosby; 2014. p. 472-510.
- ^ Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005 Feb;16(1):26-35.
- ^ Lindquist LW, Rockler B, Carlsson GE. Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. J Prosthet Dent. 1988 Jan;59(1):59-63.
- ^ Shackleton JL, Carr L, Slabbert JC, Becker PJ. Survival of fixed implant-supported prostheses related to cantilever lengths. J Prosthet Dent. 1994 Jan;71(1):23-6.
- ^ Weinberg LA, Kruger B. A comparison of implant/prostheses loading with four clinical variables. Int J Prosthodont. 1995 Sep-Oct;8(5):421-33.



