Bone Grafting: Essential Indications and Techniques in Implant Dentistry
Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Limited bone availability makes implant placement challenging and sometimes unpredictable. Candidates for implant therapy must have enough bone to enable implant placement in a position that allows for proper form, function and emergence profile of the dental prosthesis. Also, as teeth are lost, the subsequent bone resorption can result in a lack of attached gingiva on the facial aspect as the mucosal tissue relocates to the crest of the edentulous ridge, potentially compromising the esthetics of the case.
Fortunately, socket and defect grafting procedures allow us to regenerate bone at sites where deficiencies are present, facilitating implant placement for patients who might otherwise be contraindicated for treatment. This has made proper bone grafting techniques an essential part of the implant practitioner’s skill set. Indeed, the days of being restricted by limited bone availability are long gone, even in esthetically demanding situations. With the use of the appropriate materials and techniques, clinicians can prepare a site for eventual implant placement or repair a bone defect during immediate implantation with a high degree of restorative predictability.
The days of being restricted by limited bone availability are long gone, even in esthetically demanding situations.
BONE GRAFTING MATERIALS
Although autogenous grafts, which are harvested from another site on the patient’s body, were long considered the “gold standard,” they have fallen out of favor among many clinicians due to the invasiveness of this procedure. Allograft materials, harvested from the bone of human donors, have become very popular because a second surgical site is not required. With cortico/cancellous allograft materials, bone is ground into cortical and cancellous particles and processed to prevent disease transmission and antigenic response. The cortical particulate provides space maintenance during the regeneration process, while the cancellous bone remodels at a faster rate.
Mineral-collagen composite is a grafting material that becomes a moldable putty upon wetting. The calcium phosphate-based mineral is combined with a type 1 collagen derived from bovine Achilles tendon and features a carbonate apatite structure similar to natural bone. Although standard alloplastic (synthetic) and xenograft (from another species) materials are additional options, the use of cortico/cancellous allograft blend and mineral-collagen composite will be described here, as their suitability for a wide range of bone regeneration procedures is ideal for the implant armamentarium.
SOCKET REGENERATION
Simple socket regeneration techniques are an important adjunct following the atraumatic extraction of teeth. Tooth extraction is accompanied by changes in bone morphology, as the socket site will resorb, leaving a shorter, thinner residual ridge. Delayed implant placement requires adequate bone quality and quantity to achieve sufficient primary stability and eventual osseointegration, necessitating ridge preservation to help maintain available bone.
After tooth removal and thorough debridement, an allograft material or mineral-collagen composite is prepared for insertion into the extraction socket. The grafting material is hydrated and then packed firmly — but not aggressively — into the socket. Care should be taken to avoid crushing any of the grafting material, which can accelerate the rate of resorption. The grafting material is eventually replaced by the patient’s own bone and is a safe, predictable means of preserving the ridge.1
Because epithelial tissue grows significantly faster than bone regenerates, it is imperative that the extraction socket be covered with a protective membrane, which provides a barrier against epithelial downgrowth into the grafted site. Resorbable membranes are intended to last anywhere from eight weeks to several months before dissolving and are ideal for most grafting procedures because a second surgical procedure is not required to remove the membrane. Following socket grafting and in the absence of facial defects, the membrane is positioned directly over the crestal aspect prior to suturing.
IMMEDIATE IMPLANTATION AND DEFECT GRAFTING
Bone grafting is typically indicated when immediately placing an implant following an atraumatic extraction. Because tooth sockets are elliptical in cross section and implants are cylindrical, grafting material must be added to fill in any gaps greater than 2 mm.2 This allows osteoclastic activity to resorb the bone particulate and replace it with natural bone.
When a facial defect is present at the site of an immediate implant, allograft material is usually indicated and is placed within the void and packed firmly but not condensed. A resorbable membrane is then positioned at least 2 mm beyond the facial defect and draped over the ridge to engage a minimum of 2 mm of palatal or lingual bone. Passively placing the membrane in this way will make for a predictable bone repair process and avoid the membrane becoming dislodged during suture placement or removal.3
CASE EXAMPLES
The following case examples illustrate the two most common bone grafting indications in implant dentistry. With the use of grafting material and straightforward surgical techniques, practitioners can maximize bone volume at the sites of tooth extractions and facial defects, establishing the foundation needed to achieve acceptable implant stability and excellent long-term functional and esthetic results.
CASE REPORT NO. 1: SOCKET REGENERATION
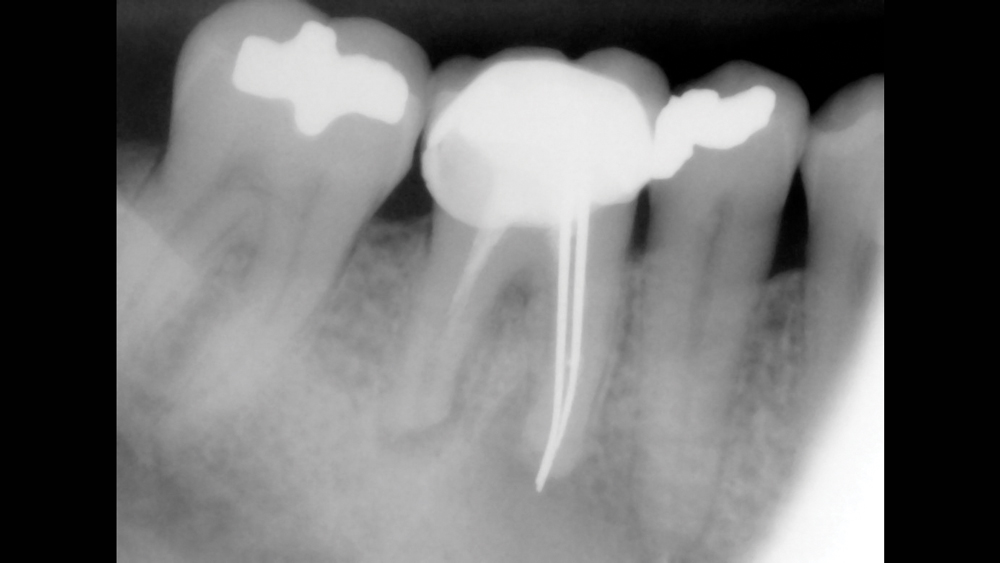
Figure 1: The patient presented with a non-restorable mandibular first molar. The tooth had received prior endodontic treatment and displayed infection and severe recurrent decay.
 Case 1 - Figure 2a
Case 1 - Figure 2a
 Case 1 - Figure 2b
Case 1 - Figure 2b
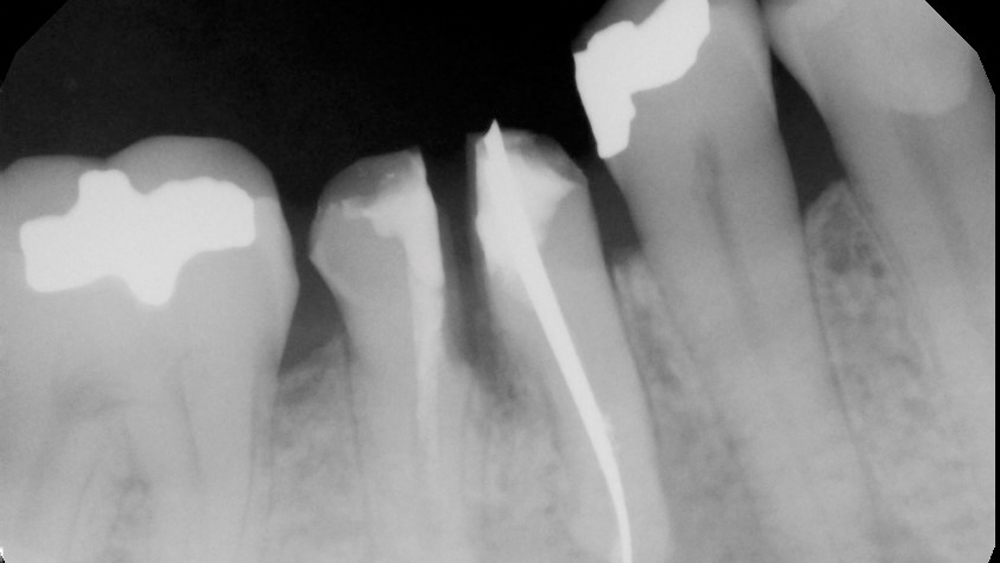
Figures 2a, 2b: The tooth was sectioned mesial-distally using a #557 surgical bur, and the existing crown was removed.
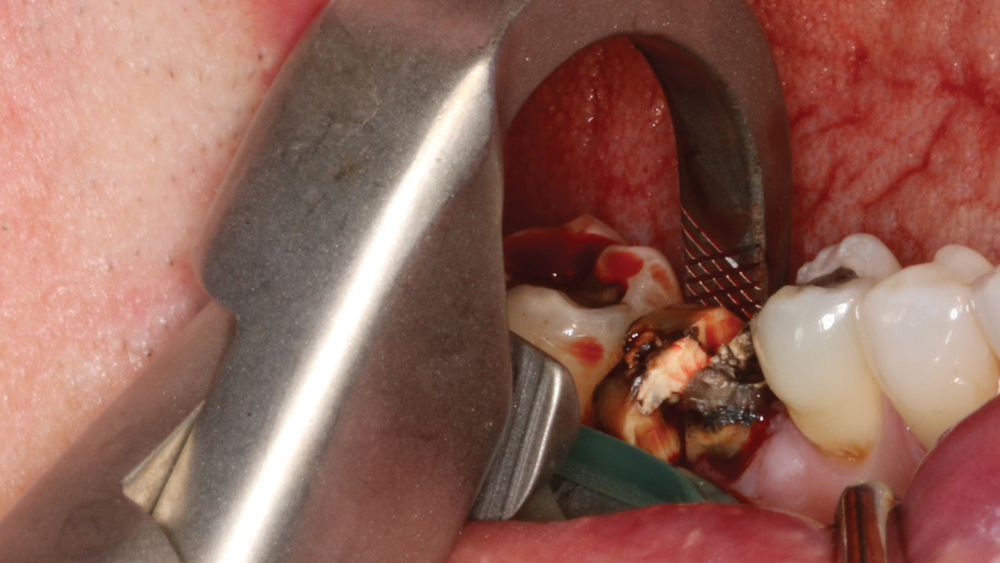
Figure 3: The individual roots were extracted using Physics Forceps® (GoldenDent; Roseville, Mich.). Although the tooth was removed in a manner that minimized trauma to the extraction socket, a large facial defect was present, necessitating a socket grafting procedure to prepare the site for future implant placement.
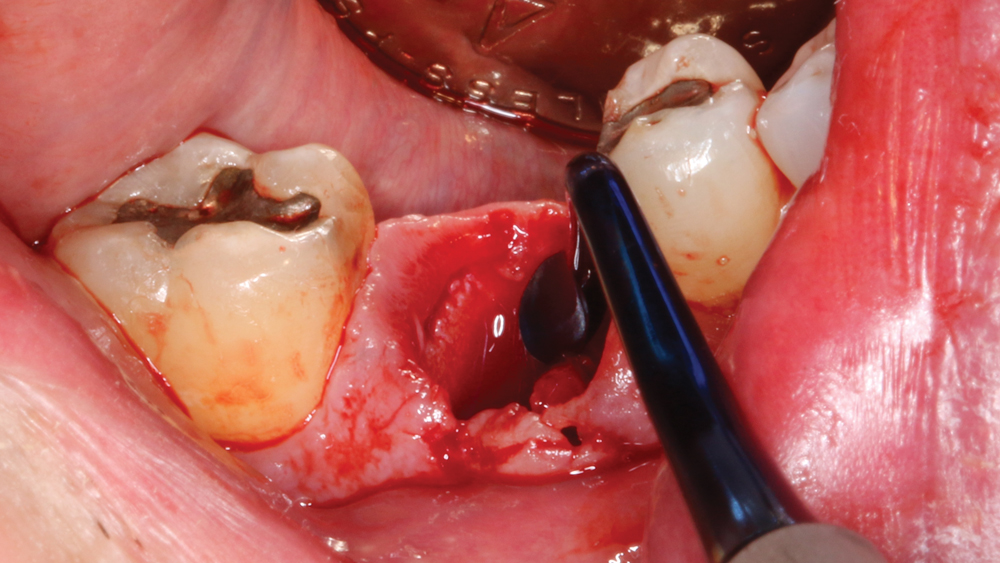
Figure 4: The socket was aggressively curetted to remove any granulation tissue and evaluate the facial defect.
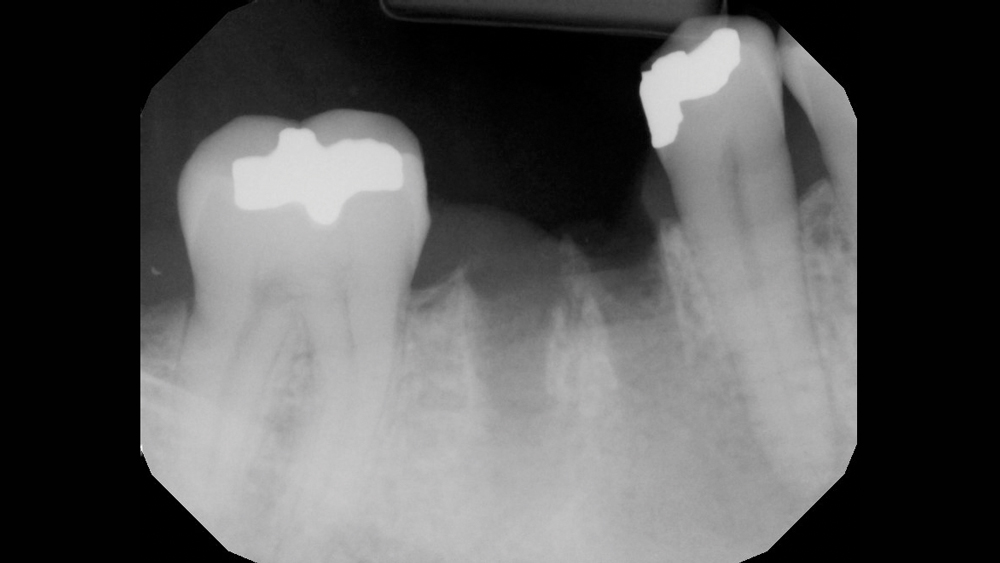
Figure 5: A digital radiograph was taken to confirm complete removal of the tooth roots.
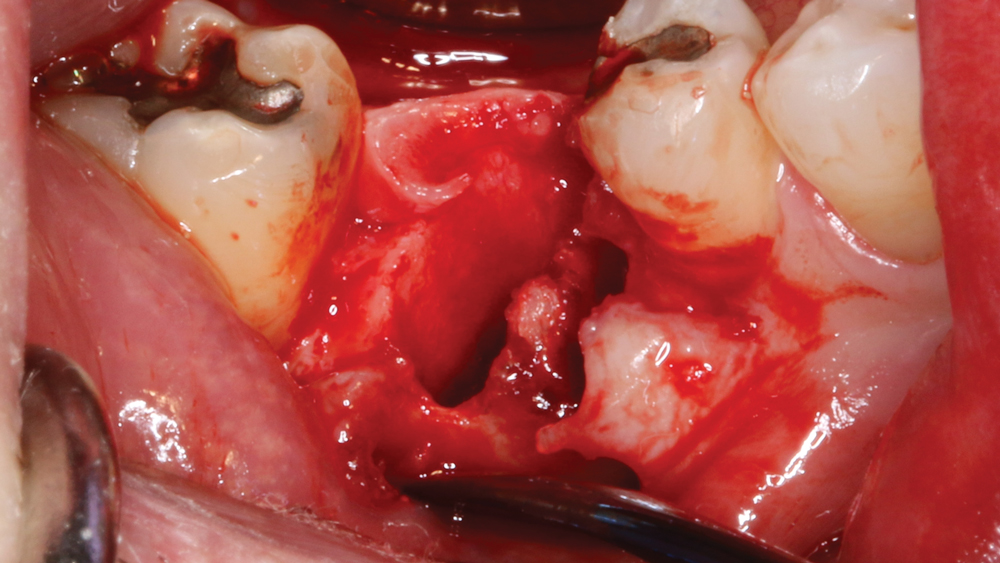
Figure 6: Because there was some crestal bone loss due to the infection of the tooth, a simple envelope flap was made facially and lingually to expose the defect. Note that vertical incisions were not necessary.
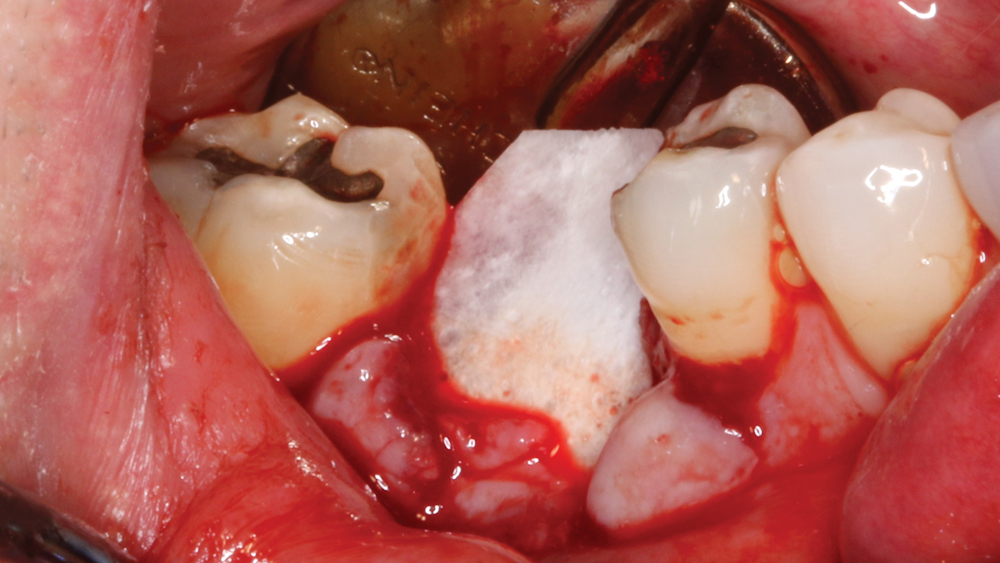
Figure 7: A Newport Biologics™ Resorbable Collagen Membrane 3-4 (Glidewell Direct; Irvine, Calif.) was cut to proper size and positioned a minimum of 2 mm beyond the facial defect. This ensures a passive placement where the membrane is not easily dislodged.
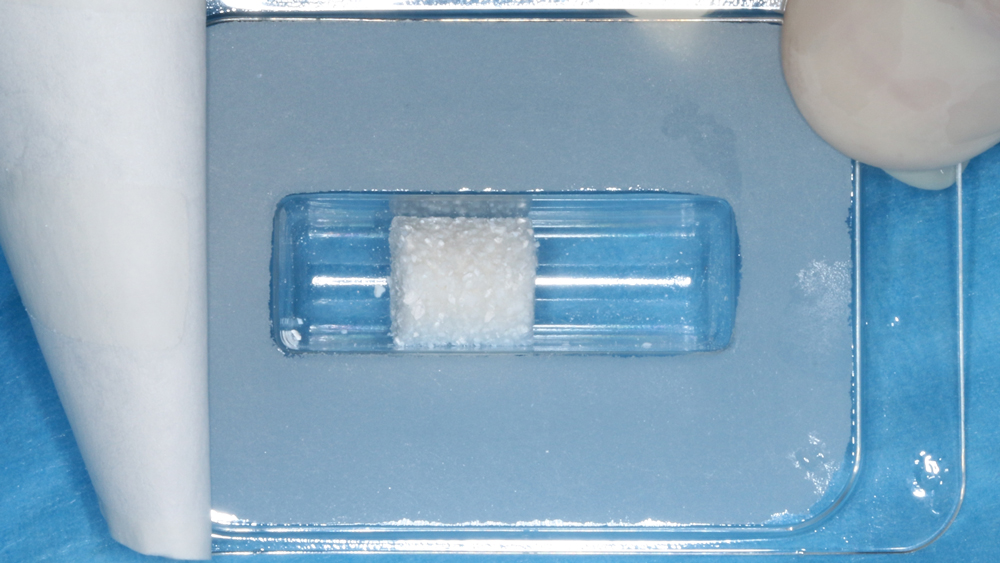
Figure 8: To maximize control and moldability of the grafting material within the large defect and socket site, Newport Biologics Bone Graft Putty Mineral-Collagen Composite was selected for the procedure.

Figure 9: The mineral-collagen composite was hydrated and then packed firmly — but not condensed — into the extraction socket and facial defect.

Figure 10: The resorbable membrane was folded over the grafted socket site to engage 2 mm of lingual bone. The technique of passively placing the membrane is critical to ensure predictable integration of the grafting material. Note that when no facial defect is present at an extraction site, the membrane is positioned directly over the crestal aspect.
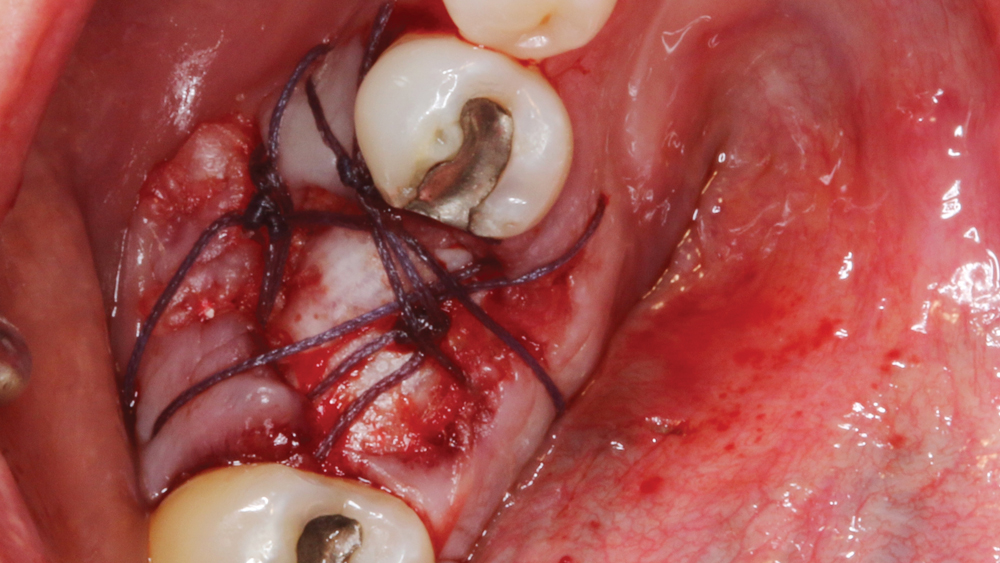
Figure 11: Several Vilet Plus™ sutures (Riverpoint Medical; Portland, Ore.) were placed to close the site and maintain the membrane, which serves to prevent invagination of epithelium during the healing phase. When the membrane remains intact for a minimum of six weeks, the graft will heal predictably. The Newport Biologics membrane used in this case was selected for its drapability, strength and ability to last 3–4 months intraorally, which make it an ideal product whether or not primary closure is obtained.
 Case 1 - Figure 12a
Case 1 - Figure 12a
 Case 1 - Figure 12b
Case 1 - Figure 12b
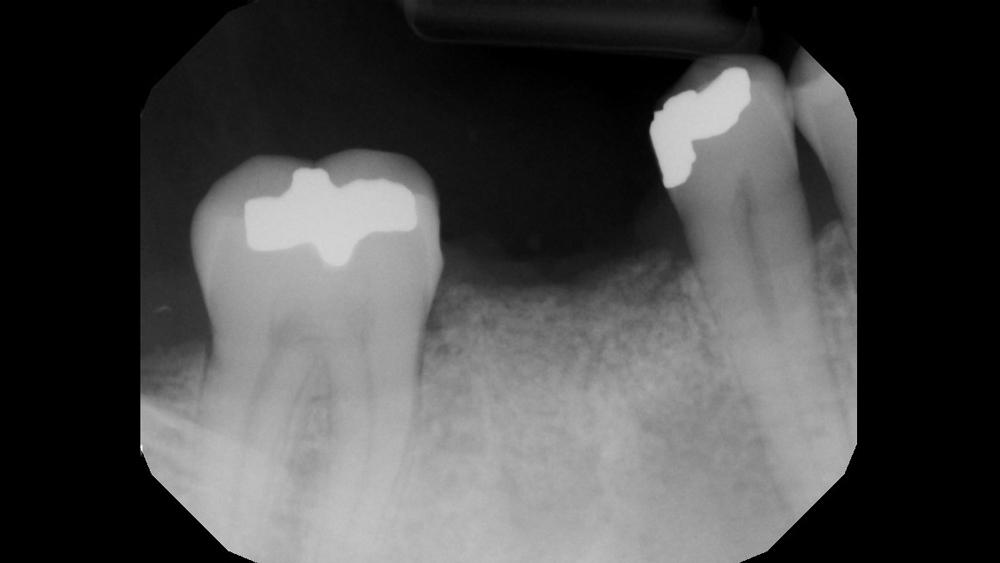
Figures 12a, 12b: Postoperative radiograph (12a) indicates an adequate fill of the extraction socket following placement of the grafting material. Four-month follow-up radiograph (12b) confirms successful regeneration and maintenance of bone within the extraction socket, illustrating proper bone turnover from the apex to the crest over time.

Figure 13: With adequate ridge width and height established, a Hahn™ Tapered Implant (Glidewell Direct) was placed.

Figure 14: Post-placement radiograph shows properly positioned implant, with ample space available in the apical-coronal and mesial-distal dimensions.
CASE REPORT NO. 2: IMMEDIATE IMPLANT WITH FACIAL DEFECT

Figure 1: The patient visited my office seeking treatment for a fractured maxillary right central incisor. Note the severe soft-tissue irritation around the badly damaged tooth.
 Case 2 - Figure 2a
Case 2 - Figure 2a
 Case 2 - Figure 2b
Case 2 - Figure 2b
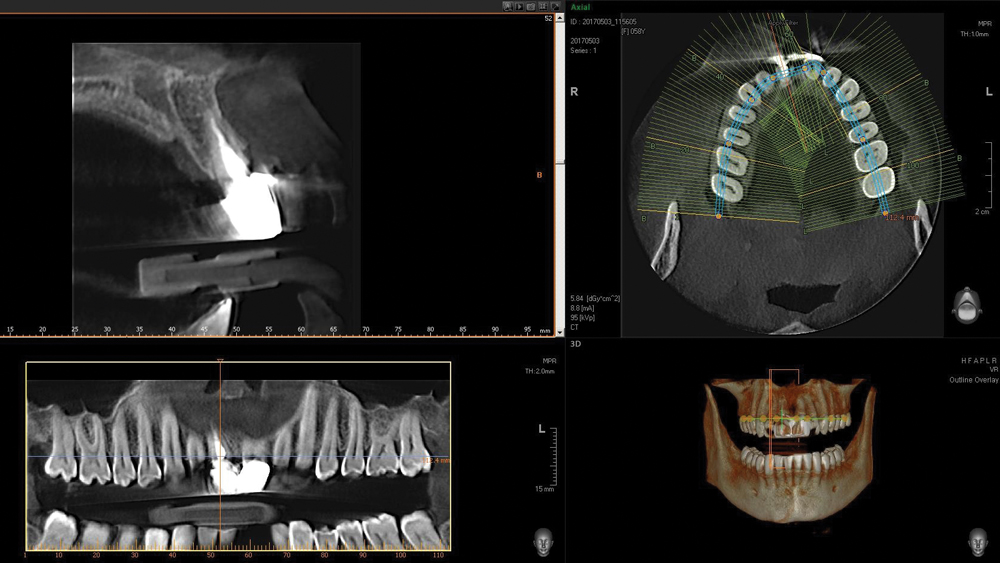
Figures 2a, 2b: Digital radiograph and CBCT analysis confirmed a hopeless prognosis for tooth #8. Note the facial defect caused by the root splitting. Implant treatment was proposed and accepted by the patient, with immediate implantation preferred if indicated following extraction of the tooth.
 Case 2 - Figure 3a
Case 2 - Figure 3a
 Case 2 - Figure 3b
Case 2 - Figure 3b
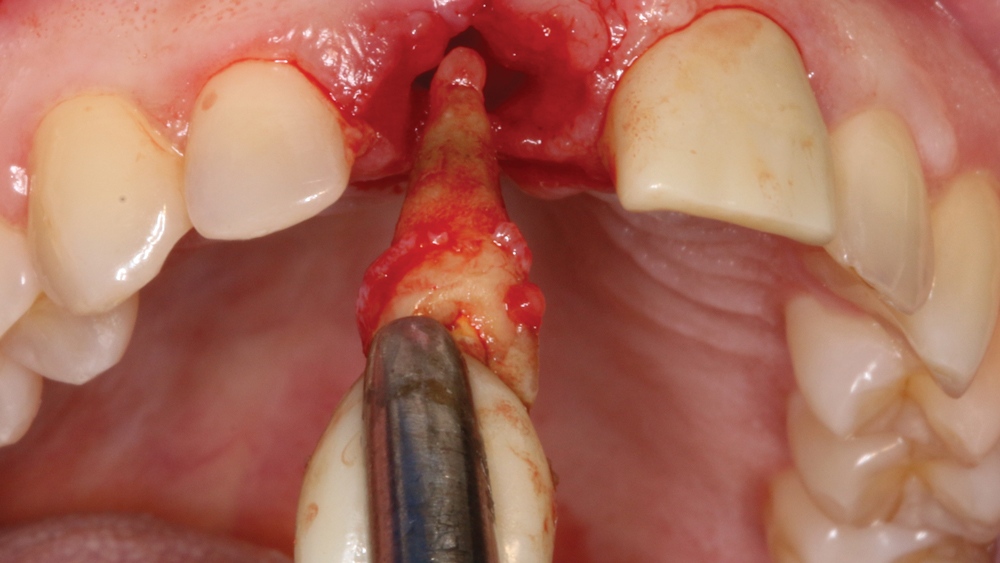
Figures 3a, 3b: The untreatable tooth was carefully and atraumatically removed.
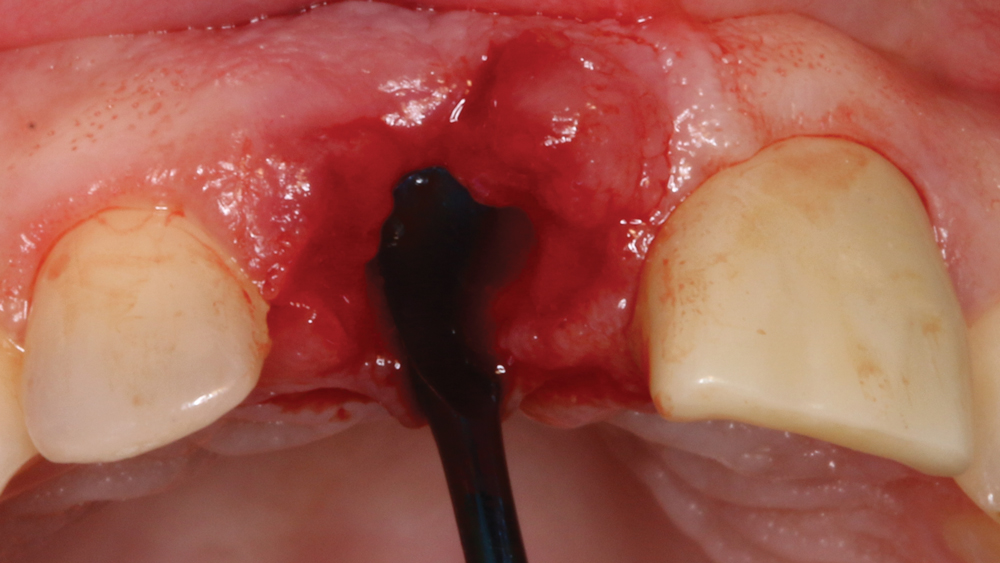
Figure 4: It is critical to curette the socket site to remove any granulation tissue and evaluate any bony defects.
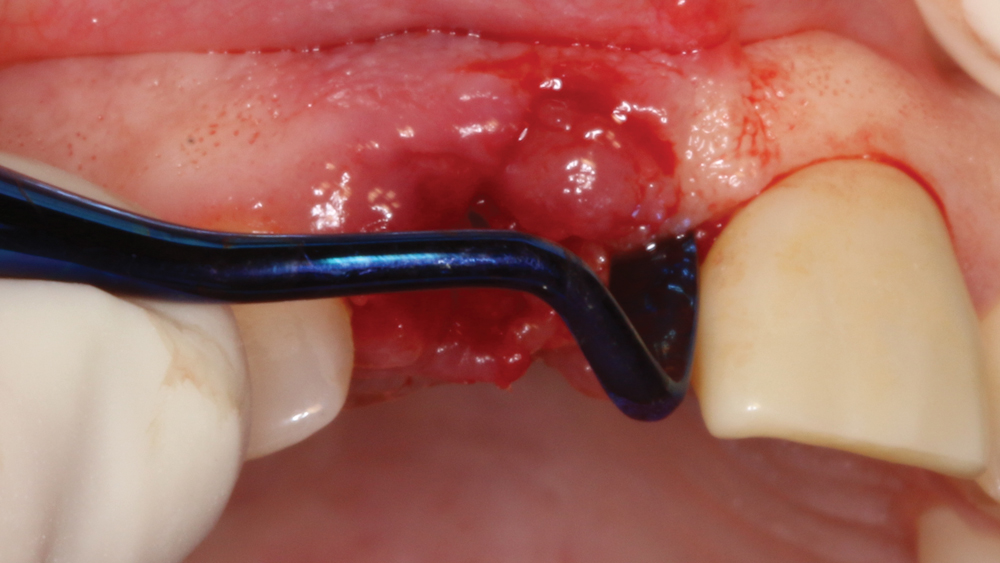 Case 2 - Figure 5a
Case 2 - Figure 5a
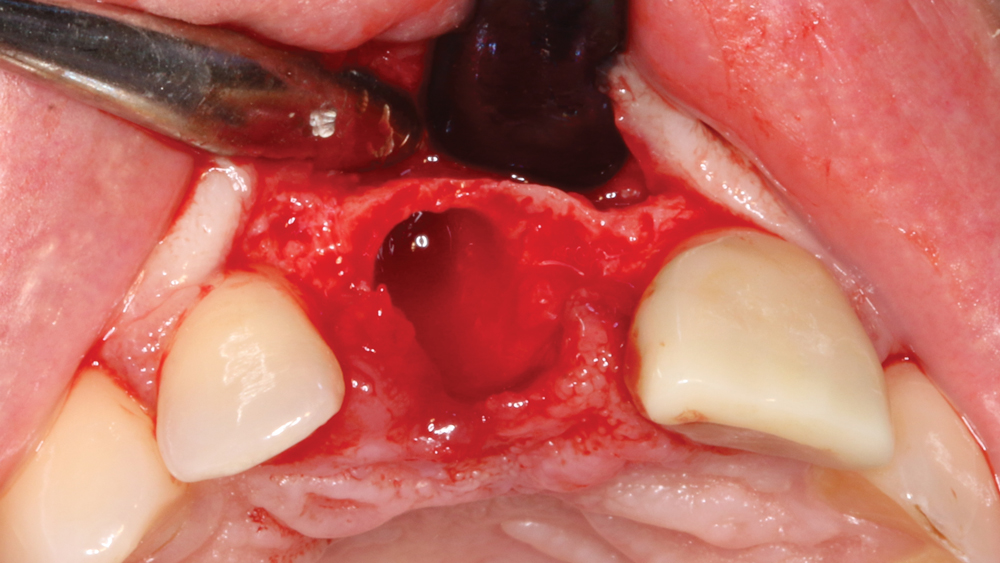 Case 2 - Figure 5b
Case 2 - Figure 5b
Figures 5a, 5b: An Orban knife was used to create an envelope flap, eliminating the necessity of vertical incisions. This allowed for visualization and examination of the facial defect prior to moving forward. Despite the presence of the facial defect, sufficient bone was available to proceed with immediate implantation with the aid of cortico/cancellous allograft material.
 Case 2 - Figure 6a
Case 2 - Figure 6a
 Case 2 - Figure 6b
Case 2 - Figure 6b
Figures 6a, 6b: Newport Biologics Mineralized Cortico/Cancellous Allograft Blend was wetted with sterile saline, and the resorbable membrane was cut to proper size to cover the defect and lay passively over the edentulous crest.
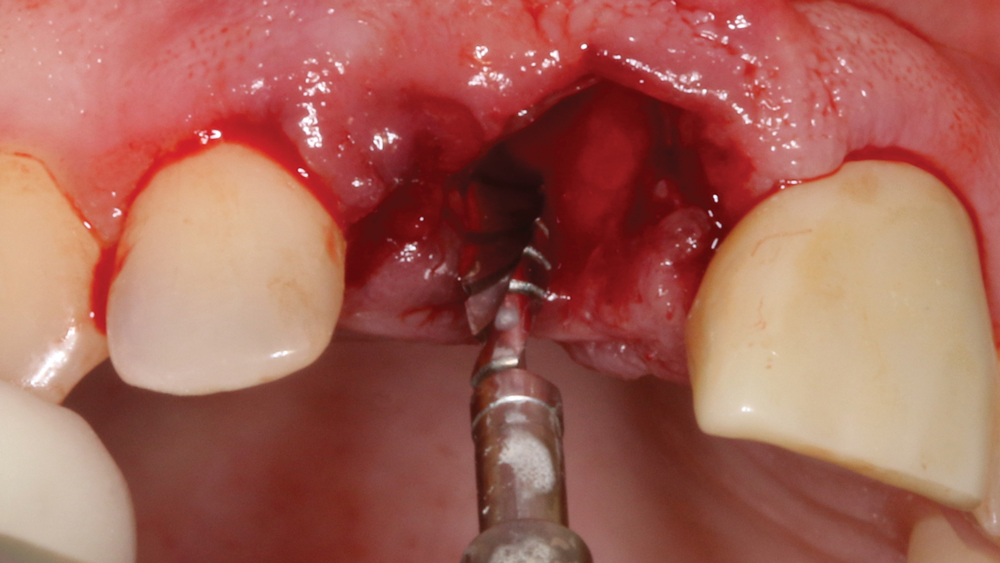
Figure 7: A pilot drill was used to make the initial penetration into the bone. The preparation was not made directly into the socket, but rather 3 mm palatal to the facial aspect of the adjacent teeth. Engaging the palatal wall helps increase initial implant stability.
 Case 2 - Figure 8a
Case 2 - Figure 8a
 Case 2 - Figure 8b
Case 2 - Figure 8b
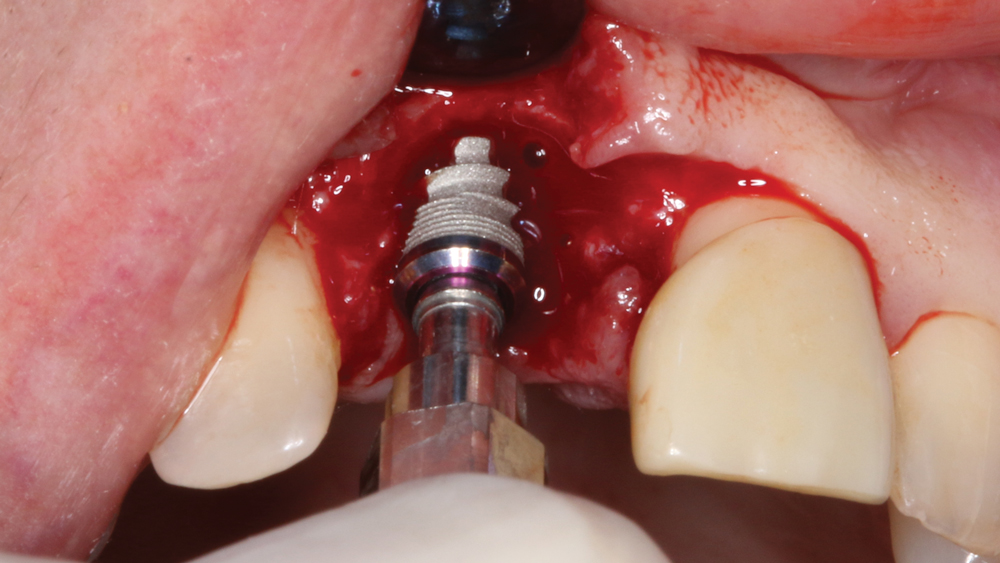
Figures 8a, 8b: The Hahn Tapered Implant was threaded into position and was tightened to a final torque value of 45 Ncm.
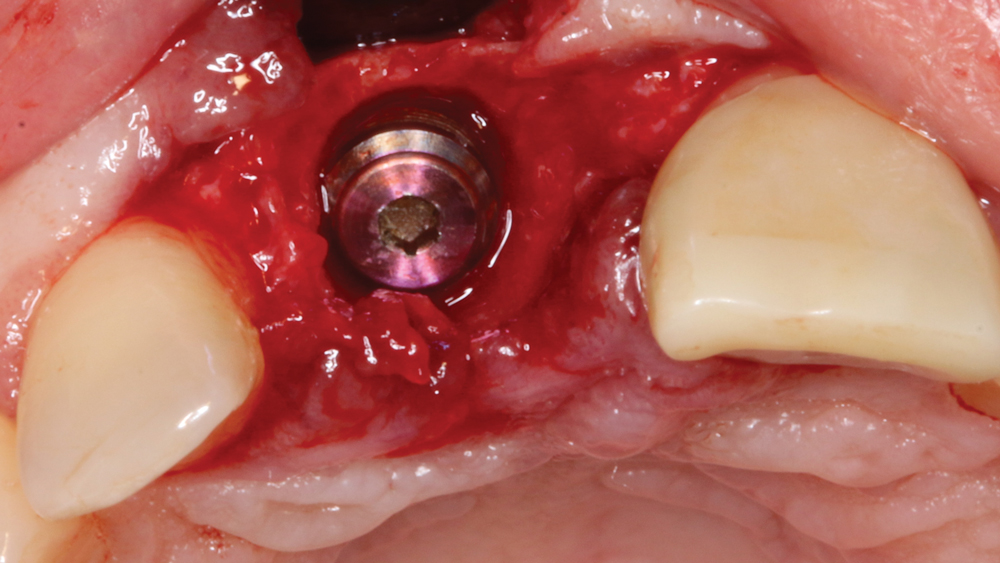
Figure 9: A cover screw was placed into the implant prior to bone grafting and membrane placement.
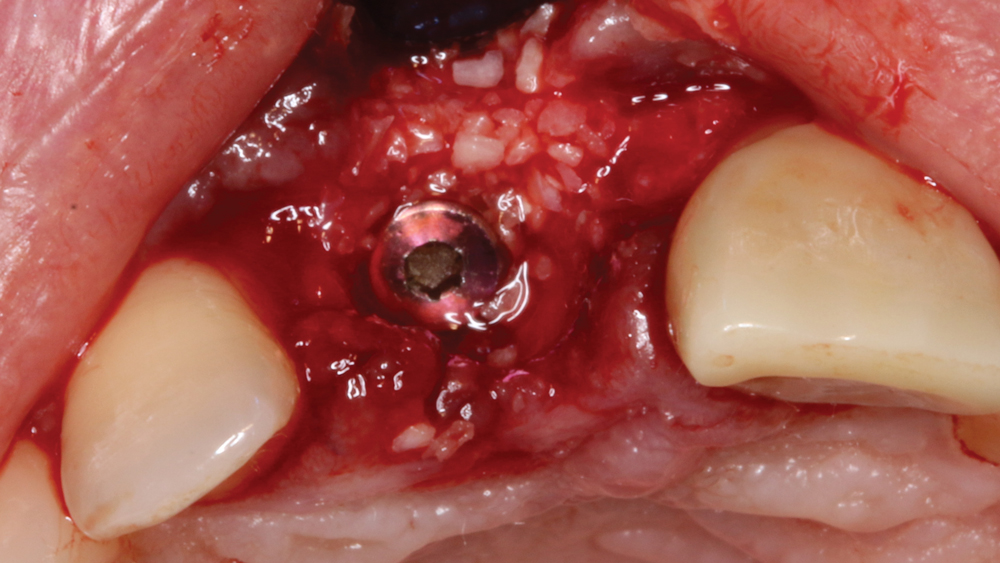
Figure 10: Newport Biologics allograft material, which provides an osteoconductive matrix for revascularization and structural integrity for the regenerated bone, was positioned in and around the facial defect.
 Case 2 - Figure 11a
Case 2 - Figure 11a
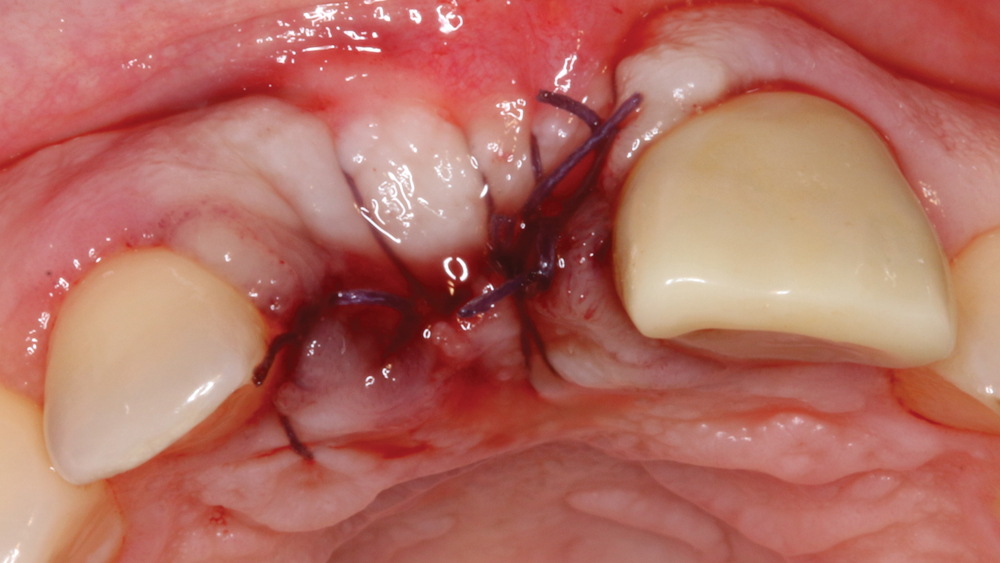 Case 2 - Figure 11b
Case 2 - Figure 11b
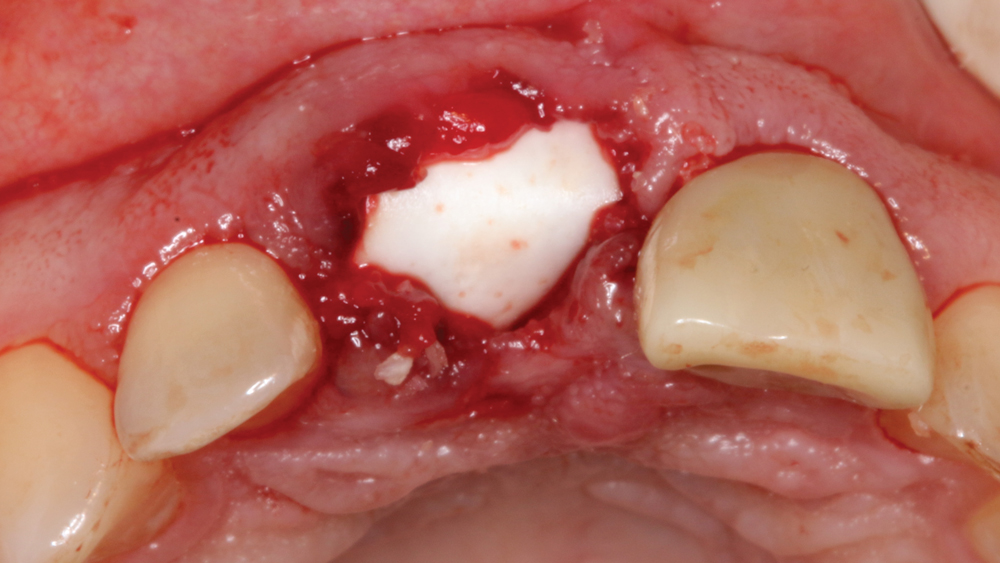
Figures 11a, 11b: The resorbable membrane was passively positioned and sutured into place.
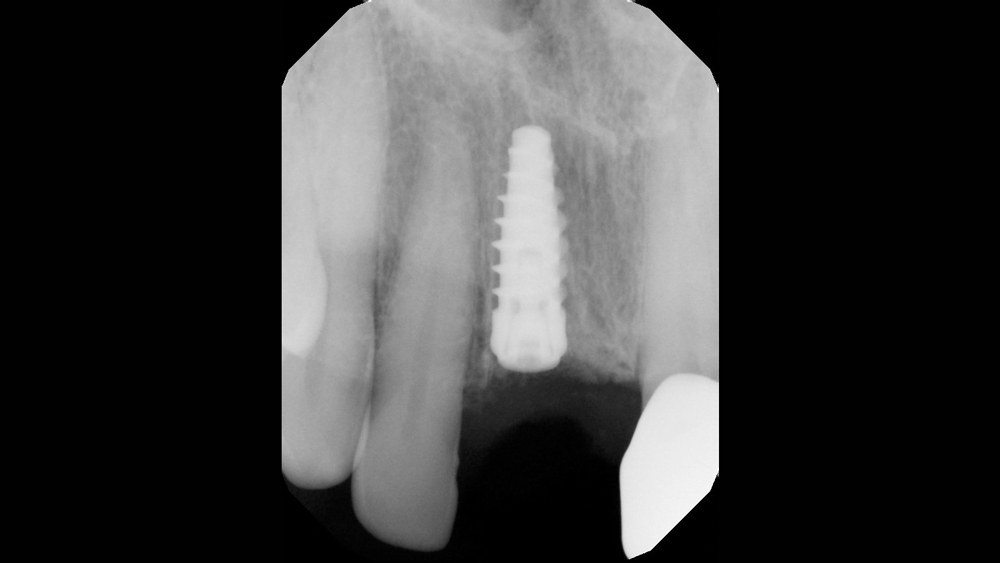 Case 2 - Figure 12a
Case 2 - Figure 12a
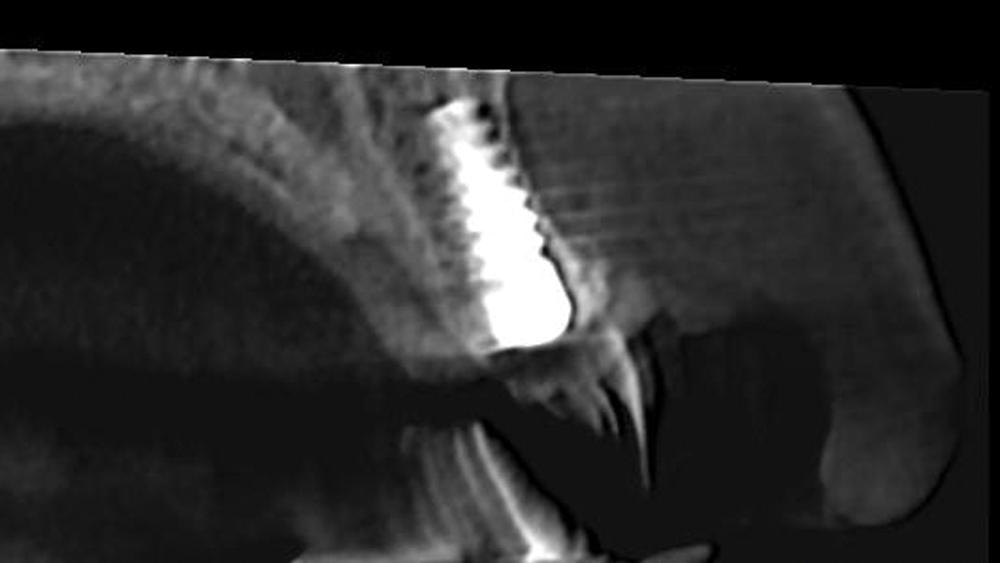 Case 2 - Figure 12b
Case 2 - Figure 12b
Figures 12a, 12b: Postoperative periapical radiograph and CBCT sagittal view illustrate properly positioned implant and grafted defect.
CONCLUSION
The loss of bone following an extraction can be unpredictable and may result in conditions that impede our ability to provide routine implant therapy. Socket regeneration and other osseous grafting procedures are a proven treatment for patients, as they allow us to confidently place implants in situations where the volume or contours of bone at the edentulous site are unfavorable. Indeed, these techniques and materials have helped elevate the quality of care by expanding the patient population able to receive implant treatment.
References
- ^Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C, Bohra AA, Scheetz JP. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003 Jul;74(7):990-9.
- ^AlGhamdi AS, Shibly O, Ciancio SG. Osseous grafting part I: autografts and allografts for periodontal regeneration–a literature review. J Int Acad Periodontol. 2010 Apr;12(2):34-8.
- ^Cafiero C, Marenzi G, Blasi A, Siciliano VI, Nicolò M, Sammartino G. Soft and hard tissues healing at immediate transmucosal implants placed into molar extraction sites with collagen membrane uncovered: a 12-month prospective study. Implant Dent. 2013 Oct;22(5):474-80.



