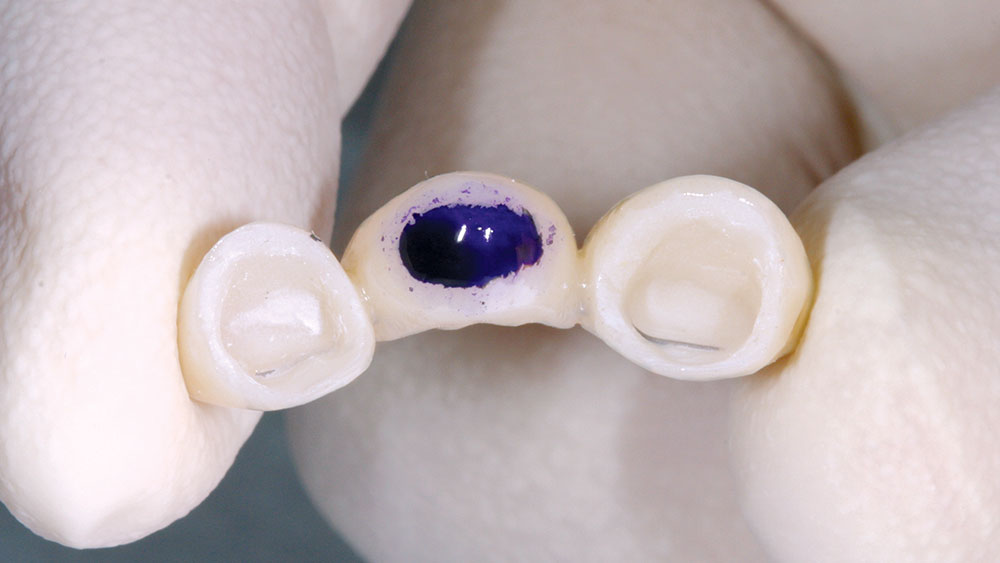
Correcting Esthetic and Functional Problems with the Use of BioTemps® Provisional Restorations

In my opinion, BioTemps® may be the most versatile restoration available in dentistry today. This is surprising considering that it is a provisional restoration, but provisionals play such a big role in managing clinical situations to ensure success with our final restorations. From tissue recontouring to ovate pontic development, BioTemps are the ideal soft tissue template for shaping gingival tissues to match your esthetic requirements. From restoring vertical dimension to withstanding months of periodontal therapy, you won’t find a better long-term provisional on the market. This article looks at some of the clinical applications I have found for BioTemps, and I welcome your input on any other uses you may have found for these versatile provisional restorations.
Case A
Case B
Case C
Case D
Case E
Case F
Case G
Case H
Clinical dentistry by Michael DiTolla, DDS, FAGD. BioTemps by Glidewell Laboratories.