When Is a Full-Crown Restoration Indicated?

Full-crown restorations are commonly placed today, and the revenue produced from this procedure makes up a significant portion of a typical general dentist’s income, as I have observed in the past.1,2,3 Practitioners may wonder if full crowns still are indicated, as there are so many resin-based composite materials that rival tooth structure in physical properties. Properly placed resin-based composite restorations are indeed beautiful and can serve for many years. However, placing large, resin-based composite restorations is difficult and time-consuming, which explains their lower rate of acceptance among practitioners. My feeling is that placement of full-crown restorations still is one of the most accepted procedures in restorative dentistry.
This article provides my observations on indications for full-crown restorations based on my years as a practicing prosthodontist. I have seen restorations, including full crowns, that have served successfully for several decades. More importantly from an educational standpoint, I have seen many failed tooth restorations — including full crowns, partial crowns, onlays, and direct and indirect intracoronal restorations — on which I will base the following suggestions for making full-crown placement the treatment of choice.
Indications for Placement of Full Crowns
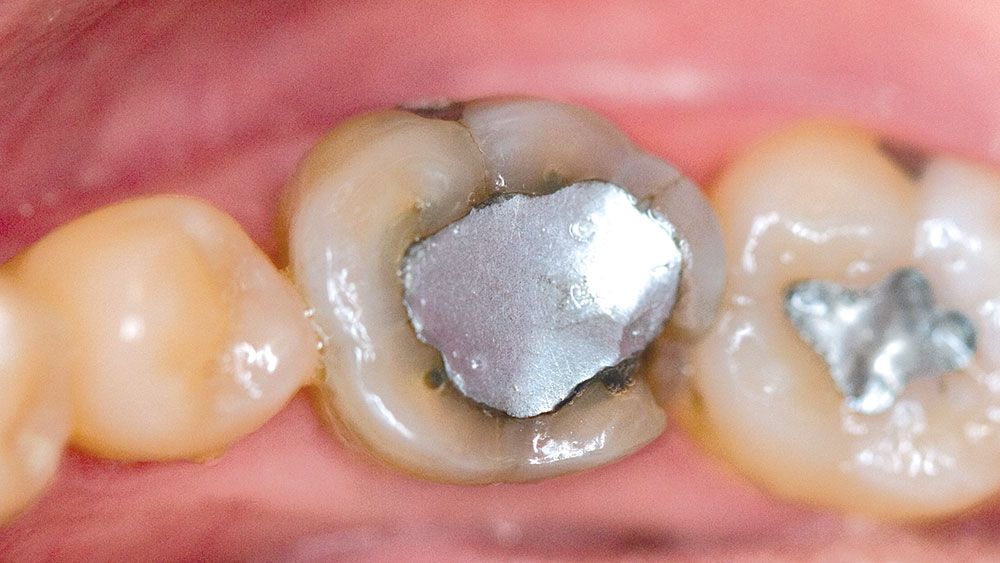
Large, previously placed restorations. From my experience, when a tooth appears to require an intracoronal preparation that exceeds one-half of the facial-lingual cusp tip-to-cusp tip distance, placement of an intracoronal direct or indirect restoration is a questionable procedure (as I have written in earlier columns4,5). Cusps often break off during service, in spite of the placement of “bonded” restorations. After informing and educating the patient about the apparent weak characteristics of the remaining tooth structure, the clinician should place a full crown or onlay covering the tooth cusps.
Cracked-tooth syndrome (symptomatic cracks in teeth). Cracked-tooth syndrome is well-known to dentists (as I wrote in 19936). It is my observation that this problem has increased during my career as the population’s average life span has lengthened. Patients with cracked-tooth syndrome complain of sharp pain when they chew in a specific way. Additionally, sensitivity to sugar-containing foods and drinks, as well as occasional unprovoked pain, are indications of a potentially cracked tooth. I have found the following diagnostic and therapeutic technique for cracked-tooth syndrome to be successful:
- Inform the affected patient that it appears that he or she has the signs and symptoms associated with cracked-tooth syndrome and discuss the alternatives for treatment of this condition. The best and most commonly successful alternative is placement of a simple crown or onlay. The dentist can assess the potential success of this simple treatment by observing the condition of the tooth after placement of the provisional restoration. If pain continues after the provisional restoration is placed, endodontic therapy may be indicated. If pain still persists, tooth hemisection or extraction and tooth replacement may be necessary.
- After the patient accepts the treatment plan, place a crown or onlay preparation on the involved tooth.
- Place a well-made resin provisional restoration on the tooth (as I described in a 1996 column7) cemented with a sedative brand of provisional cement that contains eugenol.
- Instruct the patient to allow the tooth to calm for a few days. After the healing period, chewing normally on the provisional restoration and tooth underneath either will or will not elicit pain. If pain is not present during chewing, fabrication and placement of a full crown or an onlay is indicated.
Asymptomatic cracks in teeth. When shining a light on the occlusal surface of natural teeth or transilluminating teeth by shining a light through the tooth structure from the lingual surface of the tooth, the dentist almost always notes the presence of cracks. The location of the cracks and their severity relate directly to the level of need for crown placement. If the tooth has deep horizontal cracks and an intracoronal restoration, there is a significant possibility that a piece of the tooth will break off during service. If the tooth has vertical cracks, the possibility of tooth breakage appears to be less.
Often, when removing a previously placed intracoronal restoration, the clinician will find cracks extending entirely through the enamel and dentin into the internal aspect of the tooth preparation. The presence of visible horizontal cracks anywhere in the tooth, or of internal cracks inside the tooth preparation when previously placed restorations are removed, are strong indications for placement of either a crown or an onlay restoration. When the dentist observes these conditions, he or she should show the patient their presence and discuss the desirability of placing a restoration that increases the tooth’s strength by covering its occlusal surface.
Endodontically treated, heavily restored teeth. In the past, it was taught in dental schools that all endodontically treated teeth should receive full-crown restorations. Undoubtedly, this belief became prominent when dentists observed that many endodontically treated teeth fractured during service. In recent years, the pendulum of clinical opinion swung in the opposite direction, and “bonding” cusps of endodontically treated teeth together by using acid etching and resin-based composite became common. However, dentists have observed that the conservative restorations often failed and that the cusps fractured in spite of previous bonding.
This topic elicits mixed opinions. It has been my observation that many endodontically treated teeth with minimal endodontic access openings, minimal or no previously placed restorations, and absence of horizontal cracks can serve well with only bonded resin-based composite restorations. If the endodontically treated tooth has been restored previously with large restorations and/or if horizontal cracks are present, a crown or onlay is indicated.
Broken cusps. Frequently, cusps break from either previously restored or unrestored teeth. These broken cusps often extend apically to the bone, leaving only a small amount of tooth structure on which to place a restoration. The dental pulp may or may not be exposed when the cusps break off. Sometimes crown lengthening is necessary to allow future optimum gingival health. Crowns are almost always indicated for teeth with broken cusps.
Hemisected teeth. Although hemisection is discussed frequently in continuing education courses, the number of hemisections actually accomplished in practice is low. It is apparent that when a part of a tooth has been amputated, the only logical restoration is a full crown that connects the affected tooth to an adjacent tooth for additional support.
Mobile teeth requiring splinting. Splinting teeth to counteract weakening of periodontal supporting structures and concomitant mobility has been both accepted and condemned as a viable therapy during my career. If remaining tooth structure is adequate in quantity, the periodontium is stable, the occlusion has been equilibrated, and the teeth are mobile to the degree that the patient cannot eat normally without painful movement of the mobile teeth, splinted crowns are a logical treatment. However, in my experience, splinting the mobile teeth together with resin-based composite holding an orthodontic wire or fibers on the lingual tooth surfaces is a successful and less aggressive technique. Splinting teeth with crowns occasionally is necessary, and this technique can provide years of service from teeth that otherwise would be extracted.
Need for esthetic upgrading. Esthetic upgrading is perhaps the most common reason that crowns are placed today. Most patients want to have their teeth look “normal” in color and shape. Frequently, crown or veneer placement is the only way to achieve that goal. The improvement in both esthetic appearance and function provided by properly placed all-ceramic or porcelain fused to metal crowns is well-known among practitioners. Dentists report to me that well-placed esthetic crowns result in fewer patient complaints than almost all other treatment areas in dentistry.
However, before deciding to treat the unesthetic condition with crowns, dentists and patients should consider one or more of the following techniques: tooth bleaching, orthodontic tooth movement, incisal/occlusal tooth recontouring, conservative tooth veneering, direct resin bonding or other conservative techniques (as I wrote in an earlier column4).
Crowns are a legitimate and logical way to improve the appearance of teeth, provided that the patient provides proper informed consent before beginning the procedure, and that they know that dental third-party payers usually will not pay for restorations that are placed only for esthetic reasons.
From my experience, when a tooth appears to require an intracoronal preparation that exceeds one-half of the facial-lingual cusp tip-to-cusp tip distance, placement of an intracoronal direct or indirect restoration is a questionable procedure. After informing and educating the patient about the apparent weak characteristics of the remaining tooth structure, the clinician should place a full crown or onlay covering the tooth cusps.
Frequently, cusps break from either previously restored or unrestored teeth. Crowns are almost always indicated for teeth with broken cusps.
Esthetic upgrading is perhaps the most common reason that crowns are placed today. Most patients want to have their teeth look “normal” in color and shape. Frequently, crown or veneer placement is the only way to achieve that goal.
Summary
Crowns are one of the most common dental therapies. There are several biological reasons to place crowns — reasons that are easily acknowledged and have been discussed in this article. Dentists should inform patients about the biological need for crowns, educate patients as to why crowns are the preferable treatment for their specific situation, and be prepared to provide the various types of crowns at an acceptable quality level. If crown placement is the most logical procedure to improve esthetic impairments, patients should be so advised. However, if treatments less aggressive than crowns are logical options, clinicians also should discuss those with patients.
Christensen GJ. When is a full-crown restoration indicated? J Am Dent Assoc. 2007 Jan;138(1):101-3. Copyright ©2007 American Dental Association. All rights reserved. Reprinted with permission. Please note: All figures, pictures and captions were added by Glidewell, and did not appear in the original JADA article. The American Dental Association makes no representation and accepts no responsibility for the accuracy, timeliness or comprehensiveness of the figures, photos and captions.
Dr. Christensen is the director, Practical Clinical Courses, and cofounder and senior consultant, CRA Foundation, 3707 N. Canyon Road, Suite 3D, Provo, Utah 84604. The views expressed are those of the author and do not necessarily reflect the opinions or official policies of the American Dental Association.
References
- ^ Christensen GJ. Ceramic vs. porcelain-fused-to-metal crowns: give your patients a choice. J Am Dent Assoc. 1994 Mar;125(3):311-2, 314.
- ^ Christensen GJ. The confusing array of tooth-colored crowns. J Am Dent Assoc. 2003 Sep;134(9):1253-5.
- ^ Christensen GJ. Why all-ceramic crowns? J Am Dent Assoc. 1997 Oct;128(10):1453-5.
- ^ Christensen GJ. Restoration or crown? J Am Dent Assoc. 1997 Jun;128(6):771-2.
- ^ Christensen GJ. Sorting out the confusing array of resin-based composites in dentistry. J Am Dent Assoc. 1999 Feb;130(2):275-7.
- ^ Christensen GJ. The cracked tooth syndrome: a pragmatic treatment approach. J Am Dent Assoc. 1993 Feb;124(2):107-8.
- ^ Christensen GJ. Provisional restorations for fixed prosthodontics. J Am Dent Assoc. 1996 Feb;127(2):249-52.