The Evolution of Human Occlusion — Ancient Clinical Tips for Modern Dentists
Man evolved in an environment in which the occlusion was worn down quickly, resulting in flattened occlusal and interproximal surfaces. This rapid wear reduced occlusal decay, traumatic occlusion, malaligned teeth, impactions and temporomandibular disease (TMD). In the last 250 years, however, new food production techniques created an environment that was less dentally abrasive than earlier diets. Teeth were not worn down as programmed in our “evolutionary blueprint.” This lack of wear resulted in increased caries, cusp fractures, bruxing, malocclusion, periodontal disease and TMD. A practical re-creation of ancient dental wear patterns can help to reduce these modern dental diseases.
Great controversies have erupted recently over the question, “What is normal occlusion?” A variety of scholars, clinicians and other experts have suggested numerous hallmarks of “proper” occlusion, including appropriate cusp heights, degrees of canine rise, and adjustments favoring centric relation and/or centric occlusion.1,2,3
Many of these experts and their supporting camps have battled over which theories are correct and how occlusally related diseases should be treated. In some cases, these theories have taken the forms of mystic religions, with gurus and their disciples sniping at each other over arbitrary walls of definitional purity.
Today, as in the past, there is no one theory of occlusion which, when applied to the many dental diseases found in our society, explains and leads to cures for all cases and situations.1,2 The wide use of money-driven new technology, gadgets, for-profit educational institutes, therapy modalities and medications has not provided consistent, predictable relief to those who have temporomandibular disease (TMD) or serial cracked cusp syndrome. Some clinical techniques will cure one individual but not another who appears to have the same symptoms.2,3
Dental research into TMD and other occlusion syndromes often is a hit or miss affair with inadequate samples, lack of meaningful controls, and a general inability to master all of the relevant parameters, such as psychology, physiology and individual variation. Many studies omit obvious conditions, which nullify their results. Few TMD researchers and clinicians conduct an internal examination of the patient’s ears (to check for ear pathology that may trigger TMD) or consider the high incidence of TMD-related headaches and myalgias reported by patients taking common drugs such as Isordil® (25% incidence), Prozac® (20%) and Procardia® (23%).4
As more clinicians become enamored and then disillusioned with one theory/technique or another, the need for an accurate and universal understanding of occlusion becomes imperative for the educated dentist. We must know what “normal” occlusion is and how to treat the deviations that result in pathology for our patients and frustration for us. This article presents a historic definition of normal occlusion and evidence-based recommendations established by our evolutionary history.
Recent history
Modern theories defining normal occlusion began in the mid-1800s with Carabelli (1844) and Angle (1899) refining a classification of occlusion based on the position and interdigitation of the teeth.5 Early theories seemed to stress religion (Bonwill’s triangle of the lower jaw [1899]: “This is God’s architecture”), temperament (Angle [1900, 1907]: “though the length of overbite varies, being greater in the teeth indicating the bilious and nervous temperaments. . .”), ideals (Christensen [1905]: “the ideal bite path must always follow spherical surfaces”), or combinations of these nonscientific notions (e.g., Monson, Moses) mixed with quasi-scientific observations.5
Many dental authors today quote and derive their theories and treatments from the inspired, anecdotal scientific work of these early dentists. Jankelson’s theory of neuromuscular occlusion (1970) and Dawson’s stress reduction/harmony theory of jaw function (1989) currently are in favor.3,6
Evolution
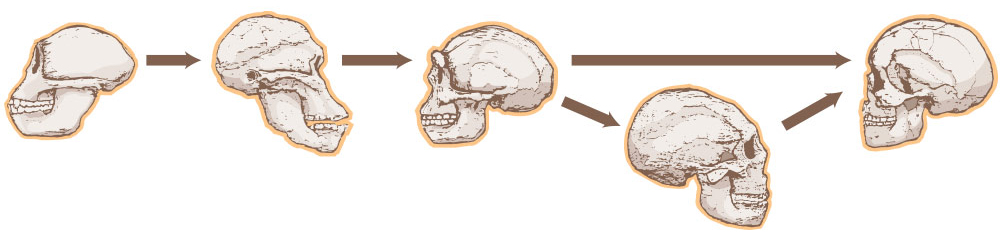
Man is the product of his evolutionary history. “Normal” occlusion, like all other aspects of human anatomy-physiology, is the result of man’s evolution. The major evolutionary pressures of heredity and environment have shaped us over our 4+ million year history.5,7,8 These forces have had a great impact on our body design and function (Fig. 1).
Heredity, the first evolutionary force, links the new generations with their ancestors. Modern humans (Cro-Magnons), as compared to earlier species (e.g., Homo erectus, the australopithecines, the Neanderthals), have existed no longer than 4,000 generations (100,000 years). Yet our anatomy, including our occlusion (flat plane), is stable and has not changed significantly (with one exception) (Figs. 1–5).7,8 Our teeth and supporting structures were genetically programmed to function in an environment of heavy attrition, which generally flattened them interproximally and in occlusion (Fig. 6).5,7,8
The second force in our evolution is environmental. It is the environment, through natural selection processes, that allows individuals (and their progeny) to survive with a variety of naturally occurring genetic mutations.7 If a mutation in one’s anatomy (e.g., size, color, intelligence) gives an advantage to a family in a particular environmental setting, they will reproduce successfully and thrive as compared to a poorly endowed group who may become extinct during the ever-present competition for limited nutrition and living space (natural selection).
Successful genetic traits, which have remained stable over thousands of generations of changing environments, are strong evidence of positive, well-established, “normal” phenotypes. Any dental trait (tooth design, jaw shape, and so on) which has lasted unchanged over the millennia of our species’ existence must be considered essentially successful and thus be the norm (“normal”).10 We know that these traits (e.g., flat plane occlusion) have evolved and were perfected, so to speak, by natural selection because they have functioned and continue to function sufficiently well to ensure continued survival and success to the humans who have possessed them. Those individuals whose anatomy deviated from these traits (mutations) are extinct, attesting to the lack of benefit derived from the deviated traits.
To identify what is normal occlusion, we must study the occlusions of our ancestors (evidence-based research) and, especially, the occlusions of modern (Cro-Magnon) man in today’s Third World and First World societies. By doing this, important lessons can be learned regarding what our occlusion is, what it should be, and how we can treat associated pathology successfully.
Flat plane occlusion
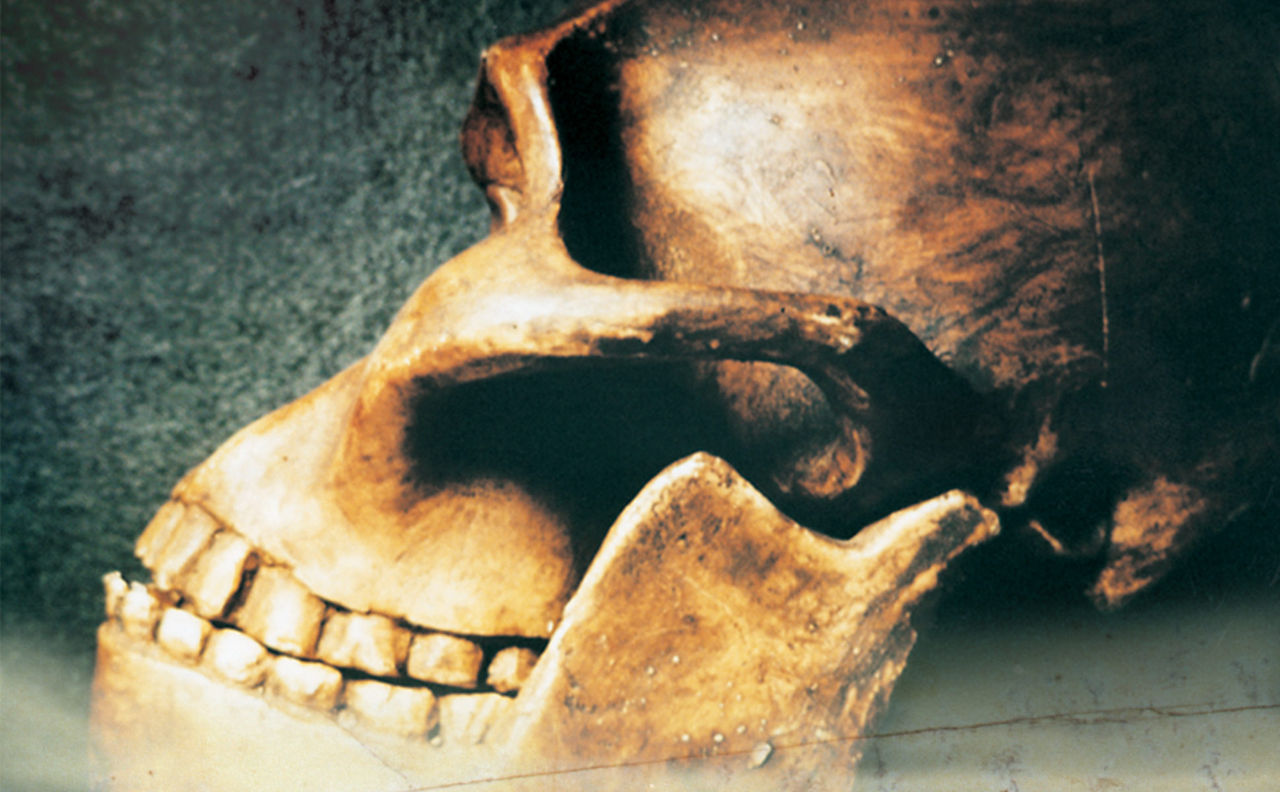
The earliest pre-human and human-like animals (the australopithecines, Homo erectus, Homo hablis, the Neanderthals) lived in an environment in which the occlusion was worn quickly (Figs. 1–5).8 Pointed cusps and deep fossa of new teeth, which served the purpose of efficient eruption and positioning, were flattened quickly by coarse, gritty diets and constant, day-long chewing, as were the grooved occlusal anatomy and pointed interproximal contacts of new teeth.5,8,11 Soft, nonabrasive food was rare, and the life span essentially was determined by the ability to chew enough food adequately to extract sufficient nutrition to survive.7 The lack (until recently) of fossils and historic skeletons with cuspal oclusion or less than half of their natural teeth attest to the fact that early man needed his teeth to survive. In a study of more than 10,000 ancient skeletons worldwide, fewer than 0.02% had cuspal occlusion.7,8,11-16 In ancient times, life was brutish, mean and short. Maintaining cuspal occlusion or losing too many teeth would reduce chances of survival.15
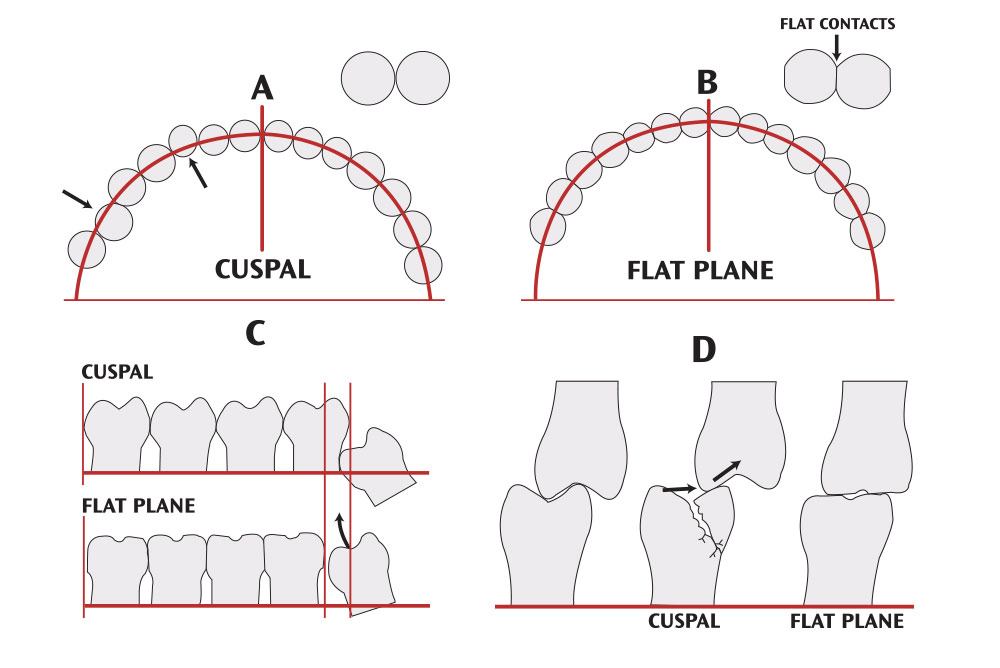
Early man and many present-day residents of Third World nations chewed and lived with flattened, well-worn teeth (Figs. 5–9).11-15 This condition is termed flat plane occlusion (Fig. 6).12,15 In flat plane occlusion, the occlusal table is predominately flat. The teeth have low (if any) cusps and shallow fossa. The interproximal areas are worn nearly flat so that teeth contact each other on a broad surface area (Fig. 5). The interproximal distance between teeth is shortened. There is essentially no canine rise and little incisor guidance. The bite often can be slipped into an edge-to-edge relationship in which centric occlusion (the maximum interdigitation of the teeth) becomes centric relation (the occlusion manifested by the most superior position of the mandibular condyle in the glenoid fossa).3 The jaw can slide easily into all excursions, including protrusion and lateral directions, with most teeth contacting each other.11,12,15,18 This condition represents a range of wear in which cusp inclines may vary slightly (between 0 and 20 degrees) and some teeth may not occlude in concert with their neighbors. Generally, every tooth is naturally flattened and equilibrated with the others (Figs. 5, 6).8,11,12
Heavy dental wear is the primary source of flat plane occlusion (Figs. 5, 6, 8). The most common cause (seen today and assumed historically) is fine abrasives in food and a relatively long period of mastication each day. Eating gritty food contaminated with sand or earth from the natural environment or from worn millstones (used in pre-industrial societies) gradually will lead to flat plane occlusion. Based on skull studies from all societies in human history (except recently in the industrial world), this condition has been the norm for most of mankind since the time of the australopithecines (4 million years ago) (Figs. 1–5).8,12,16 Essentially, everyone had flat plane occlusion. Cuspal occlusion in adults was rare (Fig. 6).
Flat plane occlusion compared to cuspal occlusion
People currently living in industrialized societies possess predominately cuspal occlusion.8,11,12,15, This form of occlusion is seen in the majority of patients. This is caused by the lack of tooth attrition and, with few exceptions, was first noted 250 years ago when metal rollers replaced the grit-producing grinding stones used in food production.7 With cuspal occlusion, the teeth maintain their cusps and fossa.
Flat plane occlusion is the main chewing system of prehistoric and nonindustrialized man.8,12 In flat plane occlusion, the occlusal tables are flat, reducing prematurities and traumatic occlusions that occur frequently in people who have cuspal occlusion. With low or nonexistent cusps, cracked cusp syndrome and fracturing is rare. Patients with cuspal occlusion suffer greatly from these problems, especially as they age and undergo dental restorations, which allow chewing pressures to fracture weakened cusps (Fig. 6).
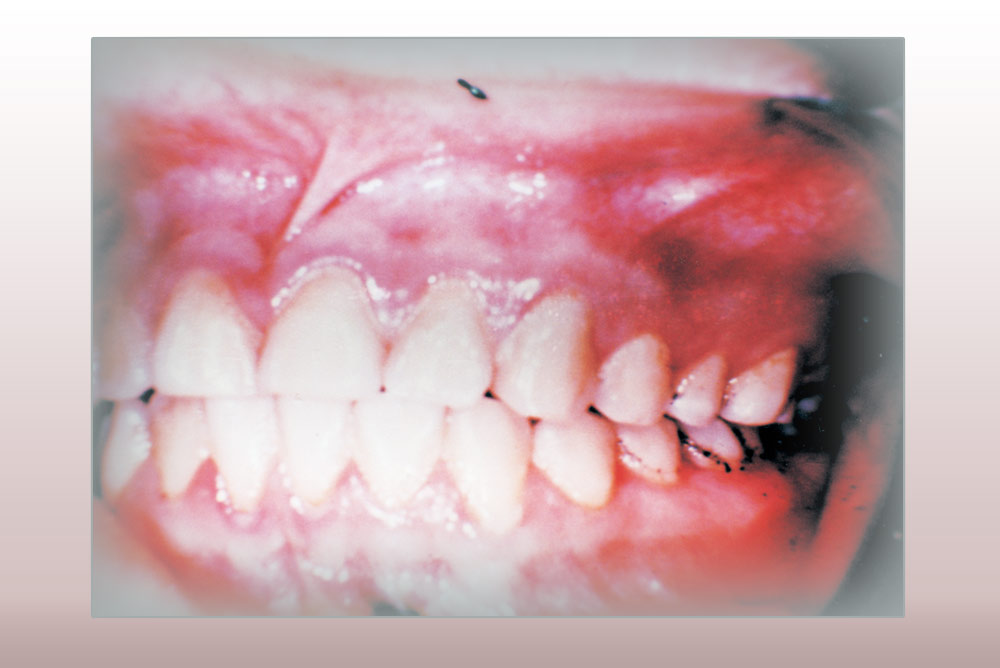
In flat plane occlusion, the mandible is free to move, unrestricted, to any position of the mouth (e.g., occlusolaterly), reducing excessive stresses (e.g., traumatic occlusion) on individual teeth and the temporomandibular joint (TMJ).8,15 This condition is seen often in today’s children.9 The anterior teeth, unlike those seen in modern adult populations, are worn down quickly to a shape that renders them occlusally inert.11,12,18,19 There is little or no incisal guidance and no canine rise, and the anterior occlusion often is noted as being edge-to-edge (Figs. 2, 3).5,7,8,11,18 In modern populations, with less tooth wear, anterior teeth will restrict and “guide” excursive jaw movements, sometimes resulting in stressed periodontium and TMJ tissues.3,12,15,20
Tooth malalignments are rare in flat plane occlusion because the inherently unstable “point” interproximal tooth contacts seen in cuspal occlusion are worn down quickly to flat, broad, stable surfaces reminiscent of stone blocks in a Roman arch (Figs. 2–9). In cuspal occlusion, because of the rounded interproximal contacts, tooth slippage (buccally or lingually) occurs easily, contributing to dental malalignments in the arch and future periodontal pathology (Fig. 6).8,11,13
In flat plane occlusion, mesial drift and interproximal wear, which often amount to 1.0–1.5 cm per arch, provide added arch space for the eruption of most third molars, reducing the incidence of impactions (Fig. 6).5,8,11 In cuspal occlusion, this beneficial wear is minimal, leaving a longer tooth-filled arch and causing a higher incidence of impacted third molars and associated pathology.13 Until recent times, this was a major cause of mortality and morbidity (natural selection). If one of our predental treatment ancestors developed pericornitis around an impacted third molar, there was a high probability of the genetic lineage being terminated.
In flat plane occlusion, crowding of mandibular anterior teeth seldom is observed because heavy interproximal wear compensates for the loss of arch space due to the natural lingual tipping of the anterior teeth (Figs. 8, 9).8,17 In populations with cuspal occlusion, lower incisor tipping is a serious cause of crowding and orthodontic relapse.
In today’s populations who exhibit flat plane occlusion (e.g., the nonindustrialized Third World), chewing is an important activity and is done throughout the day (Figs. 7–9).5 Because of the toughness of the diet, long periods of mastication are needed to process food. Essentially, these people graze all day long on tough, fibrous, low calorie material. They generally are thin and comfortable, and appear to gain some psychological satisfaction from the habit.12,15 Often their jaw muscles are hypertrophied, presenting the appearance of a wide middle face (Fig. 7).15 TMD is rare.8,11,15,16
By contrast, in Western societies, chewing times are reduced and usually restricted to soft foods at short prescribed mealtimes.6 Apart from meals, mastication generally is limited to soft, high calorie snacks (often eaten all day long) and softer chewing gum, with many episodes of destructive bruxing apparently fulfilling a need to further exercise the mastication muscles.5,12
Flat plane occlusion reduces the size of the tooth’s occlusal fossa and developmental grooves. Often the tooth becomes a smooth, flat table of enamel and hardened, sclerosed secondary dentin, which is less likely to retain food or promote decay (Fig. 5). There is no apparent loss in nutrition due to the reduced efficiency in this form of occlusion. Frequently, the enamel edges of the occlusal surface acquire a sharpness, which aids in mastication (thegosis). Cuspal occlusion, though somewhat more efficient in mastication because of the teeth’s pointed cusps and inclined planes, provides opportunistic food collection sites and leads to tooth decay and cusp fracture (Fig. 6).7,11-16
Flat plane occlusion causes flattening of interproximal contacts and, with the help of mesial drift, reduction of the interproximal space between teeth. This in turn reduces the amount of food that can collect in these areas and helps limit related decay and periodontal disease until old age (Fig. 6).5,11,14-16 As the teeth gradually wear, they slowly erupt, re-establishing any lost vertical dimension.10,12
Disadvantages of flat plane occlusion
Because flat plane occlusion relies on tooth wear, it is possible that people may wear their teeth down to a point where vertical dimension is lost and chewing is uncomfortable. Resultant pulp exposures and TMJ strain could have an adverse effect on health. Severe wear and pulp exposures would tend to cause starvation unless the society is supportive (e.g., providing special diets or prechewed food), which rarely occurs historically.
Excessive interproximal attrition eventually can change the tooth anatomy to such a degree that increased food impaction promotes decay and periodontal disease. Tooth loss from periodontal disease is common in older “primitive” people.15-18 It appears that a moderate amount of tooth attrition is beneficial, while an excessive amount of wear eventually is harmful.5,7,8,10-12
Discussion
What does this mean to modern dental practices? How does this evolutionary history influence how we treat patients or define normal occlusion?
Man’s development through the australopithecines, Homo erectus and Cro-Magnon evolutionary stages occurred in an environment in which the teeth erupted into cuspal occlusion and quickly were worn into flat plane occlusion, which constituted the norm. Our anatomy developed, over time, on the basis of flat, worn dentition. Cuspal occlusion was relatively rare until recent times (the last 250 years) in industrialized societies. Though ancient man had horrific dental problems due to poor hygiene, primitive dentistry and a rugged lifestyle, flat plane occlusion prevented many conditions now seen routinely in individuals with unworn teeth. Today, in industrialized societies, there is a high incidence of TMD, occlusal decay, bruxism, traumatic occlusion, fractured cusps, third molar impactions and orthodontic crowding associated with cuspal occlusion.19 These afflictions are comparatively rare in fossils, ancient medical writings and present-day Third World patients who exhibit normal levels of flat plane occlusion (Figs. 2–9).
It is the author’s recommendation that we assist our patients in emulating this lost form of occlusion as a means of treating the pathologies listed above. This does not mean wholesale flattening of all teeth using heatless wheels at the next appointment, but a gradual re-creation of natural worn dentition as the conditions present themselves.7,8,11
Patient treatment guidelines
The following guidelines are recommended for treating patients.20,21 Obviously, discretion is required on a case-by-case basis (Figs. 8, 9).
When restoring a tooth, create shallow anatomy and low cusps, and fill in any deep grooves or fossa without seriously altering flat plane occlusal function. It is not necessary to recreate textbook-like secondary developmental anatomy on the occlusals of every restored tooth. Creating flat plane anatomy will reduce occlusal decay, traumatic occlusion and fractured cusps.
When restoring a tooth with an interproximal restoration, shape it so that the contact is wide and flattened instead of the point contact advocated in many dental school texts. This will reduce food impingement and instability leading to tooth crowding and other malalignments. It will contribute to interdental space closure (mesial drift), which will reduce plaque collection.
If possible, treat impactions and slight crowding (as happens frequently in mandibular anterior teeth) by lightly stripping the contacts of teeth in the arch. Stripping 0.25 mm per contact per tooth can easily gain 4.0+ mm of arch space without seriously damaging the enamel. This may be sufficient to reduce anterior crowding and allow many impacted third molars to erupt.
Strip interproximal contacts so they are flat rather than rounded. This will stabilize the teeth and prevent further crowding. After active orthodontic treatment, flatten the contacts to maintain tooth position.
Gently equilibrate patients at each visit, removing excessive prematurities as if an abrasive food were being eaten, causing natural attrition. Do this gradually, using articulating paper in all excursions. Ideal occlusion occurs when the jaw can slide easily into any excursion (i.e., centric occlusion equals centric relation).3
People have an evolutionary acquired need to chew stiff materials. Encourage patients with common TMD or bruxism syndromes to gently chew stiff fibrous materials (e.g., toothpicks, stimudents, or popsicle sticks). Chewing gum is too soft.
Do not build up or restore high cusps, especially on the canines (canine rise). This creates uneven forces, resulting in TMJ stress and traumatic occlusion. Let the patient’s natural wear patterns guide you. Reconstruct crowns to a morphology similar to the neighboring teeth. Avoid placing a 20-year-old’s crown anatomy in a 50-year-old’s mouth.
Like natural attrition, these changes must be done gradually, as if the patient were eating pumice on French fries. Follow the patient’s physiology and jaw movements rather than depending on artificial programs or measuring devices, which exhibit an inferior and limited design compared with the patient’s jaws and TMJ. Be practical and responsive to the patient’s symptoms and needs. Reshape teeth as they need repair. Do nothing extreme. If there is an improvement, your patient will inform you so that you may continue. If not, you may have to rely on the older, traditional dental treatments.
Remember, our evolutionary history prescribes flat plane occlusion. All living humans were designed to chew with flattened teeth. It is a part of our natural history and in our genes. Our prehistoric record substantiates this fact. Deviations from this model may cause serious problems for our patients; when this happens, re-establishing normal occlusion can help.
Summary
Our evolutionary blueprint, formed by millions of years of natural selection, has programmed us for acquired flat plane occlusion — that is, the gradual flattening of occlusal and interproximal tooth surfaces. In modern industrialized societies, the lack of wear on teeth has maintained immature, harmful cuspal occlusion with the resultant problems of increased occlusal caries, malaligned teeth, bruxism, fractured cusps, traumatic occlusion and third molar impactions. Gradually returning patients to a modified flat plane occlusion by use of opportunistic occlusal and interproximal equilibrations, restorations, and chewing can be of significant benefit.
Acknowledgements
The author would like to thank Andent, Inc., for permission to republish their photos and Drs. H. Sutcher, H. Peck and J. Granados for their invaluable assistance.
If you would like to contact Dr. Ellis Neiburger, call 847-244-0292 or visit drneiburger.com.
References
- ^Dickerson WG, Chan CA, Mazzocco MW. The scientific approach to neuromuscular occlusion. Signature. 2000;7(2):14-7.
- ^Spear F. Occlusion in the new millennium: the controversy continues. Signature. 2002;7:18-21.
- ^Dawson PE. Evaluation, diagnosis, and treatment of occlusal problems. 2nd ed. St. Louis: Mosby; 1989. p. 1-29, 434-56.
- ^Tollison CD, Kunzel RS, editors. Headache: diagnosis and treatment. Baltimore: Lippincott, Williams & Wilkins; 1993. p. 182-3.
- ^Brace CL. Occlusion to the anthropological eye. In: McNamara J, editor. The biology of occlusal development. Ann Arbor (MI): University of Michigan Press; 1977. p. 179-209.
- ^Dickerson WG, Chan CA, Carlson J. The human stomatognathic system: a scientific approach to occlusion. Dent Today. 2001 Feb;20(2):100-7.
- ^Neiburger E. Flat-plane occlusion in the development of man. J Prosthet Dent. 1977 Oct;38(4):459-69.
- ^Begg P. Stone age man’s dentition. Am J Orthod. 1954;40:298-312.
- ^Gibbs CH, Wickwire NA, Jacobson AP, Lundeen HC, Mahan PE, Lupkiewicz SM. Comparison of typical chewing patterns in normal children and adults. J Am Dent Assoc. 1982 Jul;105(1):33-42.
- ^Berry DC, Poole DF. Masticatory function and oral rehabilitation. J Oral Rehabil. 1974 Apr;1(2):191-205.
- ^Begg P. Progress report on observations on attrition of the teeth in its relation to pyorrhea and tooth decay. Aust J Dent. 1938;42:315-20.
- ^Davies DM. The influence of teeth, diet, and habits on the human race. London: W. Heinemann Medical Books; 1972. p. 62-70.
- ^Price W. Eskimo and Indian field studies in Alaska and Canada. J Am Dent Assoc. 1936;23:417-37.
- ^Heuser H, Panke H. Dental caries and periodontal disease in stone age man. Dental Abstr. 1960;5:478-80.
- ^Pedersen PO. The dental investigation of the Greenland Eskimo. Proc R Soc Med. 1947;14:478.
- ^Alt KW, Rösing FW, Teschler-Nicola M, editors. Dental anthropology. New York: Springer-Verlag; 1998. p. 203-373.
- ^van der Linden FP. Theoretical and practical aspects of crowding in the human dentition. J Am Dent Assoc. 1974;89:139-53.
- ^Dahlberg A. The dentition of the American Indian. In: Laughlin WS, editor. Papers on the physical anthropology of the American Indian. New York: Viking Fund; 1949. p. 138-77.
- ^Pereira CB, Evans H. Occlusion and attrition of the primitive Yanomami Indians of Brazil. Dent Clin N Am. 1975 Jul;19(3):485-98.
- ^Kirveskari P. The role of occlusal adjustment in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997 Jan;83(1):87-90.
- ^McNeill C. Occlusion: what it is and what it is not. J Calif Dent Assoc. 2000;28:748-58.
Reprinted with permission from the Academy of General Dentistry. Copyright ©2002 by the Academy of General Dentistry. All rights reserved.