Photo Essay: The Importance of Connective Tissue
It is important to determine whether the connective tissue present is attached or unattached at the start of a case. If tissue is unattached, it provides no protection for the underlying periodontal foundation.
Fibers of the connective tissue must either be attached to the root surface or bone in order to act as a barrier to bacterial infiltration, or to prevent trauma from retraction cords or impressions. In this author’s opinion, a biologic width in which only 1 mm of attached connective tissue is present is a weak attachment. When undertaking restorative procedures, 3 mm or more of attached connective tissue is ideal and acts as a strong protection barrier for the periodontal foundation.
Case Presentation
The benefits of connective tissue in protecting the underlying periodontal foundation cannot be overstated. Connective tissue, by its tenacious consistency and vascular makeup, can be extremely beneficial in its resistance to bacterial infiltration and protection against retraction cord and impression taking. The limited ability of bacteria to infiltrate connective tissue allows for better long-term stability of the periodontium. The first case was followed for 10 years and shows the importance of connective tissue in maintaining the underlying supporting tissues of the tooth.
Case 1
Q: Can we stop recession once it has started?
Yes, if we add tissue that can protect the underlying periodontal foundation.
Case 2
Q: Can AlloDerm® (LifeCell Corp.; Branchburg, N.J.) be used for cases in which restorative treatment is to be undertaken?
Yes. Though AlloDerm may not always convert to keratinized tissue, it does create a thick band of connective tissue.
Case 3
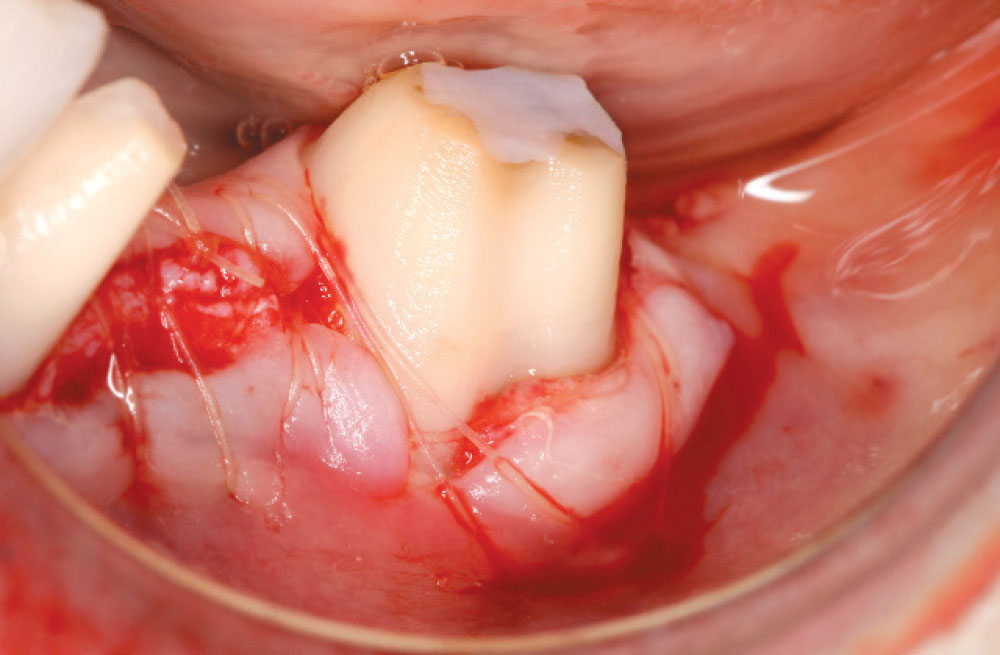
Q: What happens when a surgery is being carried out and a large dehiscence is found?
Placing a large piece of connective tissue over the root will serve as a barrier to bacterial infiltration. It also provides a stable environment for impressions to be taken without damage to the underlying support.
Case 4
Q: What is the best way to protect an exposed root from future bone loss?
Placing dense, thick vascular connective tissue over the defect will help prevent further breakdown and stabilize the area for the future.
Case 5
Q: Can we remove old Class V restorations and replace them with new ones?
Class V restorations can be removed and connective tissue placed in these areas to preserve the integrity of the foundation. In some cases, submarginal grafts can be placed to add the same stability.
Case 6
Q: Can problems occur when using weak tissue in areas where restorative is to be placed?
There is a chance of recession and bone loss when weak tissue is present; strong, dense connective tissue is preferred. Trauma from impressions or the seating of restorations can cause soft tissue breakdown.
Dr. Daniel Melker is in private practice and can be reached at 727-725-0100.