Four Common Mandibular Nerve Anomalies That Lead to Local Anesthesia Failures

ABSTRACT
Local anesthesia is essential in treating many dental and oral disorders. However, many types of anatomical anomalies are seen in the nervous system of the mandible that interfere with achieving local anesthesia. The authors describe four such anomalies, and offer ways to overcome them when trying to properly anesthetize affected patients.
Effective local anesthesia is an essential part of treatment in patients with many oral disorders. In the general practice setting, this anesthesia is often achieved by injection of a local anesthetic solution into the tissue surrounding the nerve innervating the area to be treated. Roughly 4 million local injections are administered by dentists each year,1 and in many patients, effective anesthesia is not achieved. In many cases, this failure is due to anatomical anomalies.
This article discusses four common anomalies of mandibular tooth innervation, possible reasons for local anesthesia failure and ways to overcome these problems. A review of normal anatomy of the jaw, with particular emphasis on the nervous system, is necessary to adequately discuss problems arising from an anatomical anomaly.
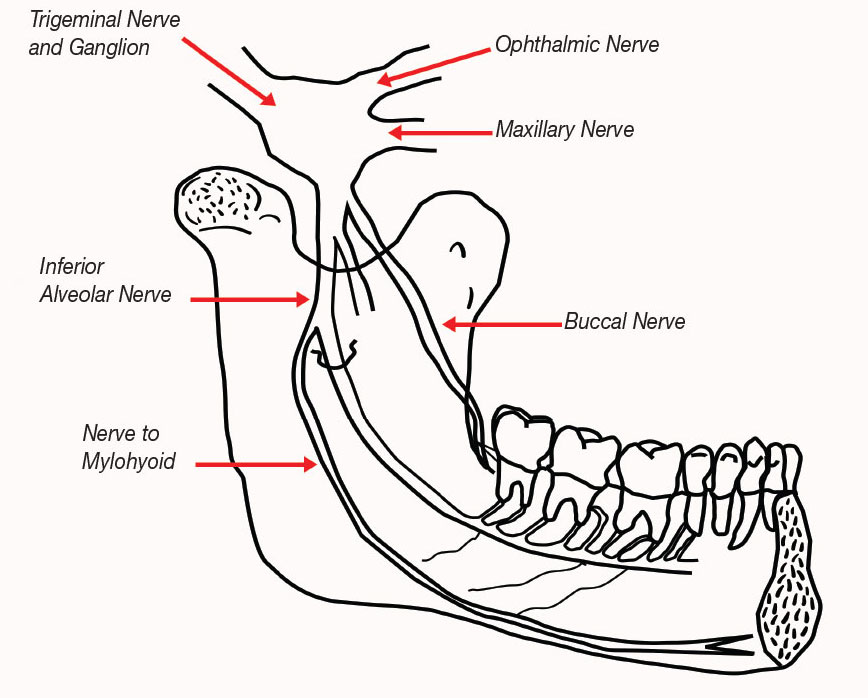
The area of the lower arch of human dentition receives sensory, and some motor, innervation from branches of cranial nerve V, the trigeminal. The fifth cranial nerve trifurcates at the trigeminal ganglion to create the ophthalmic (V1), maxillary (V2) and mandibular (V3) divisions. The mandibular nerve is of particular interest to the dentist trying to achieve mandibular local anesthesia, because it is from this branch that the inferior alveolar nerve furcates (Fig. 1).
The inferior alveolar nerve, through the dental plexus, provides sensory innervation to the teeth and some soft tissue on the ipsilateral side of the mandible. The nerve enters the mandible through the mandibular foramen, which is located on the medial surface of the angle of the mandible. The foramen is bordered by the lingula, a liplike bony prominence that serves a protective function to the nerve and its concurrent artery. It is in this area that the clinician attempts to deposit the anesthetic solution when performing an inferior alveolar nerve block (also known as mandibular block). Once inside the mandibular canal, the nerve develops into the dental plexus, which enter each tooth through the apical foramina of the root(s).
The mandible, unlike the maxilla, is composed of dense cortical bone. This is important to the clinician because of its relative inability to pass fluids, thus making infiltration nerve blocks at areas near the apexes of the teeth less effective than those administered to corresponding teeth in the maxillary arch. The inferior alveolar nerve block, therefore, is the most popular means of providing sensory anesthesia of the mandibular teeth, particularly those of the posterior sextants. Temporary loss of taste is a common side effect when the lingual nerve, another branch of the mandibular nerve, is blocked. This is easily achieved by slowly depositing anesthetic solution while retracting the needle. Blockage of the lingual nerve is an important adjunct to an inferior alveolar nerve block because of the possibility of accessory nerve supply to teeth from fibers of the ipsilateral lingual nerve.
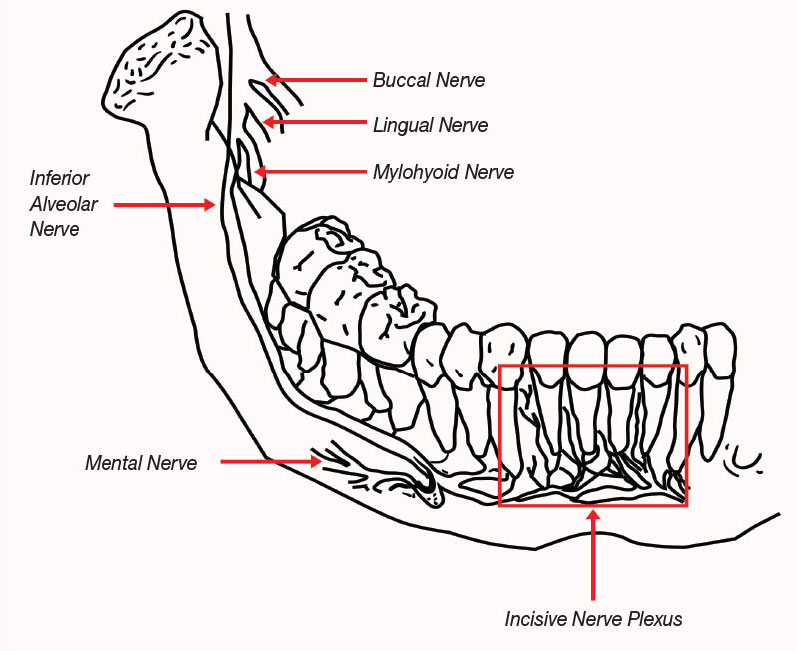
Before its entry into the mandibular foramen, the inferior alveolar nerve gives rise to the nerve to the mylohyoid muscle (or nervus mylohyoideus), primarily a motor nerve. This nerve is composed of both afferent and efferent fibers, and is the cause of many cases of anesthetic failure. On the anterior aspect of the mandible, the inferior alveolar nerve bifurcates again. One branch exits the jaw by traversing through the mental foramina and is called the mental nerve. This provides sensation to part of the buccal mucosa, lip and chin area of the face. The other branch of the inferior alveolar nerve continues to travel within the mandible and is called the incisive nerve. It provides sensory stimulation to the anterior teeth and their associated gingivae.
ACCESSORY MYLOHYOID NERVE
The mylohyoid nerve originates as a branch of the inferior alveolar nerve before the latter enters the mandibular foramen. The mylohyoid nerve is considered to be primarily a motor nerve carrying efferent information to the mylohyoid muscle and anterior portion of the digastric muscles.2 This nerve, however, has also been shown to carry sensory information from some mandibular teeth.
Expression of the dual role of the mylohyoid nerve is evidenced by microdissection studies of the diameters of the neurons composing the nerve.3,4 The results of one study indicated the presence of both motor and sensory neurons.3 In another study, Sillanpää and coworkers injected a local anethetic solution (1.8 milliliters of 3% prilocaine with felypressin) into the area directly below the mylohyoid muscle posterior to the distal root of the first molar, inducing partial anesthesia of that tooth in 21% of the subjects tested.4
Because of this afferent innervation, a conventional inferior alveolar block may be ineffective in achieving mandibular anesthesia. Wilson and colleagues found that the mylohyoid nerve branched an average of 14.7 millimeters from the entry of the inferior alveolar nerve into the mandibular canal.5 This distance could be beyond the area of diffusion of the deposited anesthetic in a conventional mandibular block, thus allowing the accessory nervous supply to continue to transmit pain signals.
These authors also presented evidence of a traceable continuation of branches of the mylohyoid nerve into foramina found on the anterior lingual aspect of the mandible. Sixteen of 37 cadavers (43%) studied had this anatomical distinction, indicating entry of the nerve’s fibers into the mandible.5
Madeira and colleagues demonstrated that 13 of 26 cadavers studied possessed a supplementary branch of the mylohyoid nerve.6 With the aid of a dissecting microscope, they showed contiguity of the nerve with either the incisor teeth and gingivae or the incisive nerve proper.6 The evidence presented demonstrates that an accessory innervation of the mandibular teeth by the mylohyoid nerve can exist. This should lead the dentist to evaluate the possible role of this type of innervation in patients who report pain during dental surgery after receiving a mandibular block.
The evidence presented demonstrates that an accessory innervation of the mandibular teeth by the mylohyoid nerve can exist.
This problem must be overcome if local anesthesia is to be achieved in patients with this anomaly. Although the technique described by Sillanpää and coworkers of injecting anesthetic solution directly into the posterior aspects of the muscle is plausible,4 extraoral nerve blocks are not widely accepted in general dentistry and should be avoided. Perhaps more practical is another nerve block described by the Australian dentist George Gow-Gates. This “high mandibular block” permeates nearly the entire pterygomandibular space, with the final optimal deposition of anesthetic solution just inferior to the insertion of the external pterygoid muscle where the pterygomandibular space is largest.
Because the pterygomandibular space contains limited fascial restricting planes, anesthetic solution may infiltrate throughout the space to anesthetize the inferior alveolar, lingual and buccal nerves.7 As stated above, the branching of the mylohyoid nerve often occurs higher than the deposition of the solution in the standard inferior alveolar nerve block. Jastak and colleagues hypothesized that with the Gow-Gates technique, the mylohyoid nerve will also be sufficiently anesthetized while it is still in the pterygomandibular space.7
Many studies have shown that the Gow-Gates block is indeed more reliable than the standard technique. Watson and Gow-Gates reported a 100% effectiveness rate with this type of injection.8 Other, perhaps more impartial researchers, have reported anywhere from a 20% to 30% increase in efficacy when using this technique.9 Although we are speculating, it is perhaps not coincidental that the reported increase in efficacy with the Gow-Gates block is roughly equal to the reported mean occurrence of accessory mylohyoid innervation.4,5,6
Although the incidence of positive blood aspiration is reported to be lower with the Gow-Gates block than with conventional inferior alveolar nerve blocks,10 aspiration techniques are imperative when injections are administered so close to major intracranial/extracranial blood vessels. Dryden has reported cases of ophthalmological emergency.11
BIFID MANDIBULAR NERVE
The bifid mandibular nerve is another anatomical variation often observed. This phenomenon often can be detected easily on panoramic radiographs because of the necessary presence of an accessory mandibular foramen and lingulae. Nortjé and coworkers used this method of detection in a retrospective study of 3,612 patients. Thirty-three (0.9%) of the subjects had a bifurcation of the nerve with dual ipsilateral canals.12
Grover and Lorton performed a similar study, using the panoramic radiographs of 5,000 U.S. Army recruits. However, they found only four of the radiographs to be highly suggestive of this anomaly.13 Although this represents less than one-tenth the incidence observed by Nortjé and co-workers, the findings still suggest that the bifid mandibular nerve could be responsible for inadequate mandibular anesthesia. Considering the number of different patients a dentist will see during a career, the probability is high that he or she will observe this anomaly.
Nortjé and colleagues reported that among the 33 patients with the bifid canal, no specific pattern of divisions or duplications was seen in the mandibles studied.12 This makes it difficult to predict the efficacy of inferior alveolar nerve block injections. Because the problematic bifurcations occur before the nerve enters the mandibular foramen, a normal inferior alveolar nerve block injection may be insufficient to block stimulus conduction for both branches. A high inferior alveolar nerve block, such as the Gow-Gates, may be effective in anesthetizing this accessory nerve at or above its branch point. If panoramic radiographs are available, the dentist should be aware of this possible anomaly and look for evidence of an accessory mandibular foramen on the radiograph.
RETROMOLAR FORAMEN
The appearance of a retromolar foramen, with or without the presence of bifid inferior alveolar nerve canals, also often predicts the presence of accessory innervation to the mandibular molars.14 This innervation is thought to arise from either the long buccal (branch of cranial nerve VII) or early accessory branches of the inferior alveolar nerve.15 Carter and Keen reported that in almost 40% (three of eight) of human mandibles with retromolar foramina, the inferior alveolar nerve was contiguous with molar teeth via the retromolar foramina.16
Retromolar foramina are thought to occur in a significant percentage of the population. Sawyer and Kiely reported retromolar foramina in 7.7% of 234 adult human mandibles.17 These authors reported no statistically significant difference in the incidence of retromandibular foramina between the sexes,14,17 but it was more prevalent among Native Americans than among subjects of European, Asian, African or Indian descent.14
The dentist who experiences difficulty achieving local anesthesia of the mandibular molar area should consider accessory innervation via retromolar entry. To overcome this problem, we recommend that a small amount of local anesthetic be deposited directly into the tissue of the retromolar area. Use of the Gow-Gates block or other high pterygoid entry injection is also recommended.15
Theoretically, this high pterygoid block would affect the inferior alveolar nerve in the pterygoid space before any branching occurs, while depositing anesthetic solution directly into the retromolar area may affect any accessory nerves from the long buccal nerve as they traverse the soft tissue before entering the mandible.
The dentist who experiences difficulty achieving local anesthesia of the mandibular molar area should consider accessory innervation via retromolar entry.
CONTRALATERAL INNERVATION OF ANTERIOR TEETH
A fourth cause of considerable anesthetic failure has been identified in the anterior portion of the mandible. As stated above, the terminal portion of the inferior alveolar nerve branches to become the incisive and mental nerves. It is widely accepted that the incisive nerve is extensively branched and offers anastomoses over the midline to the contralateral side, thus creating a crossover effect in the innervation of the anterior teeth (Fig. 2).18 This observation is, however, disputed by some on an embryologic basis.19
The mandible and the mandibular nerve are formed by the fusion of the bilateral first pharyngeal arches approximately during the fifth week of gestation.20 The mandible, therefore, is divided at the midline by the symphyseal cartilage until after the first year of life. Theoretically, this makes the possibility of crossover innervation low.21
However, crossover innervation of this region has been shown to exist in both animal and human studies.22 In a 1976 study, Rood21 assessed 62 incisor teeth given only an inferior alveolar block for their ability to achieve adequate anesthesia for an operative dental procedure. The method of administering the anesthetic agent was standardized throughout the experiment. Thirty percent of the incisors failed to become completely numb after the first ipsilateral injection.
Rood attributed the continued stimulation to two things: crossover of the inferior alveolar (incisive) nerve and the possibility of accessory stimulation from such nerves as the buccal, facial and cervical plexus.21 The mylohyoid nerve can also offer accessory stimulation to this area.23 Whatever the source of the innervation, it can pose obvious problems for the clinician attempting to achieve adequate local anesthesia of this region.
When complete local anesthesia of the anterior teeth is not achieved after an ipsilateral mandibular block has been administered, steps must be taken to block sensation due to any potential crossover or accessory fibers. One option is the use of a contralateral incisive nerve block. This procedure is technique sensitive because the injected solution must pass directly through the opening of the mental foramen to block the nerve. The foramen is normally located in the area of the apex of the second premolar.7 If possible, the dentist should consult radiographs to help him or her properly place the needle.
After the local anesthetic is deposited in this area, finger pressure may facilitate the solution’s entry into the foramen.24 Achieving both contralateral and ipsilateral nerve blocks would rule out the possibility of failure caused by crossover. Alternatives to bilateral mandibular nerve blocks for procedures on the anterior of the mandible include mental/incisive nerve blocks or periodontal ligament injections. Bilateral mandibular nerve blocks create significant inconvenience for patients because complete mandibular anesthesia leads to postoperative difficulties with speech, eating, drinking and salivary control.
As stated above, the simple supraperiosteal deposition of anesthetic solution to permeate to the apexes of mandibular teeth is of relatively low therapeutic value because of the adult mandible’s dense cortical plate. However, if the accessory innervation arises from branches from the buccal, facial or cervical plexus, and these branches are traveling in the soft tissue of the area previous so the entry into the mandibular foramen, as Rood suggests, infiltration blocks (supraperiosteal injections) may prove successful in deterring the secondary innervation.21 The mandible of the pediatric patient does appear to lack the full bone density it will acquire in the maturation process, and some success has been shown with mandibular infiltration injections alone within this patient population.25
CONCLUSION
When assessing local anesthesia failures, dentists must have a strong working knowledge of both normal and variant human anatomy. The clinician must be able to assess whether operator error or anatomical anomaly is to blame for inadequate pain management. As with any procedure in the medical or dental profession, record-keeping is of paramount importance. This is particularly true for dentists experiencing problems anesthetizing patients.
If a technique is found to be ineffective in any particular patient, a thorough investigation (via radiographs and other diagnostic tests) should be undertaken. If a cause is found, the dentist should note it in the patient’s dental record to avoid any future unnecessary pain, operator frustration and wasted chair time.
References
- ^Wong MK, Jacobsen PL. Reasons for local anesthesia failures. J Am Dent Assoc. 1992 Jan;123(1):69-73.
- ^Gray’s anatomy. 37th ed. New York: Churchill Livingstone; 1989.
- ^Frommer J, Mele FA, Monroe CW. The possible role of the mylohyoid nerve in mandibular posterior tooth sensation. J Am Dent Assoc. 1972 Jul;85(1):113-7.
- ^Sillanpää M, Vuori V, Lehtinen R. The mylohyoid nerve and mandibular anesthesia. Int J Oral Maxillofac Surg. 1988 Jun;17(3):206-7.
- ^Wilson S, Johns P, Fuller PM. The inferior alveolar and mylohyoid nerves: an anatomic study and relationship to local anesthesia of the anterior mandibular teeth. J Am Dent Assoc. 1984 Mar;108(3):350-2.
- ^Madeira MC, Percinoto C, das Graças M, Silva M. Clinical significance of supplementary innervation of the lower incisor teeth: a dissection study of the mylohyoid nerve. Oral Surg Oral Med Oral Pathol. 1978 Nov;46(5):608-14.
- ^Jastak JT, Yagiela JA, Donaldson D. Local anesthesia of the oral cavity. Philadelphia: Saunders; 1995.
- ^Watson JE, Gow-Gates GA. The clinical evaluation of the Gow-Gates mandibular block technique. N Z Dent J. 1976 Oct;72(330):220-3.
- ^Levy TP. An assessment of the Gow-Gates mandibular block for third molar surgery. J Am Dent Assoc. 1981 Jul;103(1):37-41.
- ^Watson JE, Gow-Gates GA. Incidence of positive aspiration in the Gow-Gates mandibular block. Anesth Pain Control Dent. 1992 Spring;1(2):73-6.
- ^Dryden JA. An unusual complication resulting from a Gow-Gates mandibular block. Compendium. 1993 Jan;14(1):94-100.
- ^Nortjé CJ, Farman AG, Grotepass FW. Variation in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977 Jul;15(1):55-63.
- ^Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983 Mar;41(3):177-9.
- ^Ossenberg NS. Retromolar foramen of the human mandible. Am J Phys Anthropol. 1987 May;73(1):119-28.
- ^Loizeaux AD, Devos BJ. Inferior alveolar nerve anomaly. J Hawaii Dent Assoc. 1981 Jul-Aug;12(2):10-1.
- ^Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971 Apr;108(3):433-40.
- ^Sawyer DR, Kiely ML. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent. 1991 Summer;50(1):16-8.
- ^Evers H, Haegerstam G. Handbook of dental local anaesthesia. Denmark: Schultz Medical Information; 1981.
- ^Rood JP. The analgesia and innervation of mandibular teeth. Br Dent J. 1976 Apr;140(7):237-9.
- ^Langman’s medical embryology. 6th ed. Baltimore: Williams & Wilkins; 1989.
- ^Rood JP. The nerve supply of the mandibular incisor region. Br Dent J 1977;143:227-30.
- ^Roda RS, Blanton PL. The anatomy of local anesthesia. Quintessence Int. 1994 Jan;25(1):27-38.
- ^Chapnick L. Nerve supply to the mandibular dentition: a review. J Can Dent Assoc. 1980 Jul;46(7):446-8.
- ^Cohen S, Burns RC. Pathways of the pulp. St. Louis: Mosby-Year Book; 1994.
- ^Wright GZ, Weinberger SJ, Marti R, Plotzke O. The effectiveness of infiltration anesthesia in the mandibular primary molar region. Pediatric Dent. 1991 Sep-Oct;13(5):278-83.
Reprinted by permission of the American Dental Association, ©1996 American Dental Association.