Inspired by a passion for improving lives through oral health, Glidewell Clinical Education provides contemporary, continuing education for dental professionals. Read our chief publication, Chairside® magazine, for cutting-edge clinical techniques and industry news, or take a free online CE course to expand your skillset. Listen to our “Chairside Live: Dental Insights” podcast or check out our library of over 10,000 education videos.
Education
-
 Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary
Online CE CourseIntroduction to Digital Dentistry for the Dental Auxiliary -
 Online CE CourseIntroduction to Dental Sleep Medicine
Online CE CourseIntroduction to Dental Sleep Medicine -
.png/_jcr_content/renditions/thumb-png-mobile-full.png) Online CE CourseImplant Treatment Planning: The Contributing Factors
Online CE CourseImplant Treatment Planning: The Contributing Factors -
 Online CE Course4 Ways to Provisionalize Dental Implants
Online CE Course4 Ways to Provisionalize Dental Implants -
 Online CE Course10 Things I Learned the Hard Way
Online CE Course10 Things I Learned the Hard Way -
 Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation
Online CE CourseGuided Bone Regeneration: 8 Steps to Successful Ridge Augmentation -
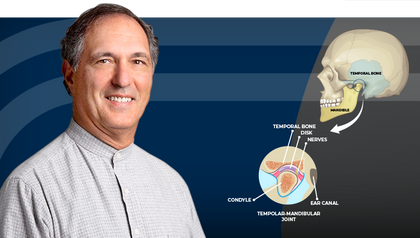 Online CE CourseTemporomandibular Disorders and the Human Jaw
Online CE CourseTemporomandibular Disorders and the Human Jaw -
 Online CE CourseRestoration of Implant Overdentures
Online CE CourseRestoration of Implant Overdentures -
 Online CE Course11 Steps to Increase Practice Production Right Away – Part 2
Online CE Course11 Steps to Increase Practice Production Right Away – Part 2 -
 Online CE CourseUsing Laboratory-Fabricated Provisionals
Online CE CourseUsing Laboratory-Fabricated Provisionals
-
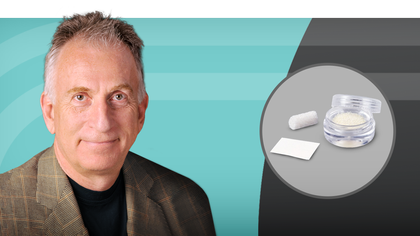 Online CE CourseBone Grafting: Selecting Biomaterials Based on the Anatomical DefectUnderstand the best practices for choosing the appropriate bone grafting material based on the anatomical defect that is present.
Online CE CourseBone Grafting: Selecting Biomaterials Based on the Anatomical DefectUnderstand the best practices for choosing the appropriate bone grafting material based on the anatomical defect that is present. -
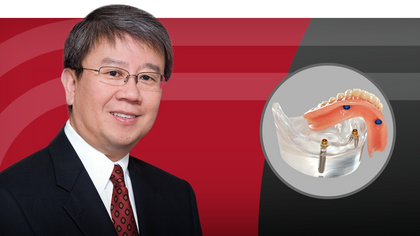 Online CE CourseComplete Dentures Part 4: Room for ImprovementUnderstanding the indications and maintenance requirements of implant overdentures is key to improving retention. Dr. Raymond Choi explains the characteristics of optimal retention, from setting proper expectations for patients to identifying recommended procedures to increase success.
Online CE CourseComplete Dentures Part 4: Room for ImprovementUnderstanding the indications and maintenance requirements of implant overdentures is key to improving retention. Dr. Raymond Choi explains the characteristics of optimal retention, from setting proper expectations for patients to identifying recommended procedures to increase success. -
 Online CE CourseComplete Dentures Part 3: Delivery DayMaximize delivery success by integrating proven techniques for comfortable and esthetic dentures. Dr. Sree Koka demonstrates and discusses essential steps such as try-ins, patient instruction, overdenture attachment pick-up techniques and occlusal adjustments.
Online CE CourseComplete Dentures Part 3: Delivery DayMaximize delivery success by integrating proven techniques for comfortable and esthetic dentures. Dr. Sree Koka demonstrates and discusses essential steps such as try-ins, patient instruction, overdenture attachment pick-up techniques and occlusal adjustments.
The best educational resource in the dental industry