- Optimizing occlusal schemes through implant positioning and crown design
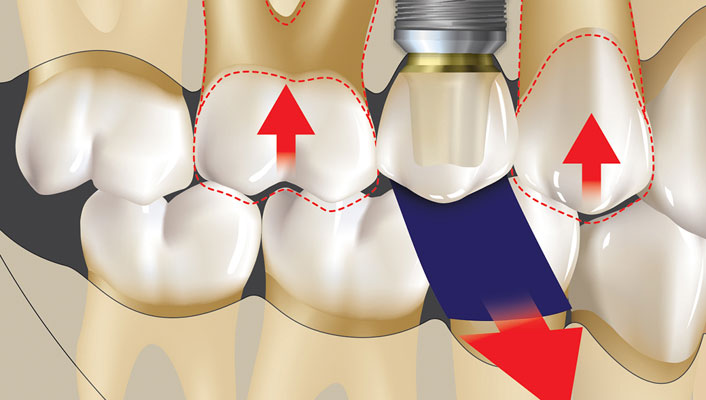
- Differences between ideal and overly large occlusal tables
- Comparisons of natural teeth and implant crowns
- How cusp inclination factors into occlusion
- Evaluation of occlusal contacts under various biting forces
- The consequences of cantilever forces on implant systems
- The effects of an increased proximal contact area
- Mutually protected occlusion
Principles of Implant Occlusion: Part 2 – Recommendations for Single Implant Prostheses
Course Objectives
2 CE Credits
The ideal occlusal scheme for an implant prosthesis is designed to control the biomechanical stress on the implant system, provide a prosthetic and biologically acceptable implant interface, and maintain long-term stability of the marginal bone, soft tissue and prosthesis. Dr. Randolph Resnik discusses the principles of implant-protected occlusion and presents specific recommendations for achieving an ideal occlusal scheme for the single implant prosthesis. Topics include:
Summary
Because of the inherent differences between teeth and implants, careful attention must be given to the development and modification of occlusal schemes for single implant prosthetic rehabilitation. The principles of implant-protected occlusion, a concept developed by Dr. Carl Misch, address several conditions to decrease stress to the implant system. Clinicians should incorporate these principles into their implant restorations to maintain forces within physiologic limits and to provide long-term stability of the implant system.
CAUTION: When viewing the techniques, procedures, theories and materials that are presented, you must make your own decisions about specific treatment for patients and exercise personal professional judgment regarding the need for further clinical testing or education and your own clinical expertise before trying to implement new procedures.
Recognition & Approval
Glidewell Education Center
Nationally Approved PACE Provider for FAGD/MAGD credit
Approval does not imply acceptance by any regulatory authority, or AGD endorsement. 3/1/2024 to 2/29/2028.
Provider ID# 216789
References
- Misch CE. Dental implant prosthetics. 2nd ed. St. Louis: Mosby; 2014.
- Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993 Sep;4(3):151-7.
- Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000 Apr;71(4):546-9.
- Misch CE. Contemporary implant dentistry. 3rd ed. St. Louis: Mosby; 2007.
- Reilly DT, Burstein AH. The elastic and ultimate properties of compact bone tissue. J Biomech. 1975;8(6):393-405.
- Miyata T, Kobayashi Y, Araki H, Ohto T, Shin K. The influence of controlled occlusal overload on peri-implant tissue. Part 3: A histologic study in monkeys. Int J Oral Maxillofac Implants. 2000 May-Jun;15(3):425-31.
- Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005 Feb;16(1):26-35.
- Shillingburg HT, Hobo S, Whitsett LD, et al. Fundamentals of fixed prosthodontics. 3rd ed. Chicago: Quintessence; 1997.
- Dawson PE. Functional occlusion: from TMJ to smile design. St. Louis: Mosby; 2007.
- Misch CE, Bidez MW. Occlusion and crestal bone resorption: etiology and treatment planning strategies for implants. In: McNeil C, editor. Science and practice of occlusion. Chicago: Quintessence; 1997.
-
 Online CE CourseBone Grafting: Selecting Biomaterials Based on the Anatomical DefectUnderstand the best practices for choosing the appropriate bone grafting material based on the anatomical defect that is present.
Online CE CourseBone Grafting: Selecting Biomaterials Based on the Anatomical DefectUnderstand the best practices for choosing the appropriate bone grafting material based on the anatomical defect that is present. -
 Online CE CourseComplete Dentures Part 4: Room for ImprovementUnderstanding the indications and maintenance requirements of implant overdentures is key to improving retention. Dr. Raymond Choi explains the characteristics of optimal retention, from setting proper expectations for patients to identifying recommended procedures to increase success.
Online CE CourseComplete Dentures Part 4: Room for ImprovementUnderstanding the indications and maintenance requirements of implant overdentures is key to improving retention. Dr. Raymond Choi explains the characteristics of optimal retention, from setting proper expectations for patients to identifying recommended procedures to increase success. -
 Online CE CourseComplete Dentures Part 3: Delivery DayMaximize delivery success by integrating proven techniques for comfortable and esthetic dentures. Dr. Sree Koka demonstrates and discusses essential steps such as try-ins, patient instruction, overdenture attachment pick-up techniques and occlusal adjustments.
Online CE CourseComplete Dentures Part 3: Delivery DayMaximize delivery success by integrating proven techniques for comfortable and esthetic dentures. Dr. Sree Koka demonstrates and discusses essential steps such as try-ins, patient instruction, overdenture attachment pick-up techniques and occlusal adjustments.