One-on-One with Dr. Michael DiTolla: Interview with Dr. Erin Elliott
Dr. Erin Elliott practices dentistry in Post Falls, Idaho, a small town just east of the Washington border. Relishing her role as a general practitioner not pigeonholed into a specific subset of the field, Erin continues to grow her practice by learning new areas of dentistry and bringing those treatments to her patients. Discover what this talented clinician has to say about treating snoring and obstructive sleep apnea, and using indirect bonding trays for accelerated orthodontics.
Dr. Michael DiTolla: I’m happy to have with us today Dr. Erin Elliott, who I met not too long ago when I was up at the Idaho State Dental Association meeting. I really liked what she had to say about her practice, because I think her two areas of emphasis are great for any dentist just getting out of school, or for those whose practices are in need of a boost. These two areas that seem to be almost ignored by general dentists are orthodontics — specifically, accelerated adult orthodontics — and snoring and sleep apnea. Erin, before we get to that, let’s go back to dental school. Tell me a little bit about what inspired you to become a dentist, and what you did when you got out that got you to where you are today.
Dr. Erin Elliott: Well, my dad is a dentist. He practiced in Long Beach, California, and I grew up in Orange County, but I didn’t grow up hanging out at his office or anything. I went away to college in upstate New York, always figuring I’d have a career in health care. I never had expectations of becoming a dentist myself; but as it turned out, dentistry was for me, and I absolutely fell in love with it.
MD: My dad was a dentist, too. His practice was three miles from the house, but I didn’t spend any time there, either. I went when I needed to borrow money. Well, it wasn’t really borrowing. I had no intention of paying it back. What was your experience like in dental school?
EE: I went to Creighton University School of Dentistry, and I absolutely loved it because there were no specialties. If I wanted to go place an implant, if I wanted to do third molar extractions, I got to do it. A part of me always felt like they held me back, though. I thought, “You know, it’s not going to take three hours to do a Class II amalgam.” When I graduated, 11 years ago now, I felt like I was ready to go.
MD: I know you’re not going to brag, but I happen to know you did very well and placed very highly in your class — much higher than I did — so maybe they were holding you back in many different ways. When you got out, did you just start doing the regular day-in-day-out, bread-and-butter general dentistry? Or were you immediately attracted to some of these other areas?
EE: I loved doing bread-and-butter dentistry. I still do. One of my professors pulled me aside once and said: “Elliott, I didn’t know you were smart. Why aren’t you specializing?” The reason I didn’t specialize was because I like to do everything, and I knew I could pick and choose what I wanted to do.
MD: It’s funny to hear an instructor say: “You’re smart. Why don’t you go into a specialty?” That’s quite an insult to GPs.
EE: I think so.
MD: Right? Like they’ll pull somebody to the side and say: “You’re dumb. Just be a GP.” Honestly, do you have to be smarter to do nine different things, or to do nothing but endo all day? You know what I mean?
EE: Yeah, I don’t envy endodontists at all.
MD: Right. The great part of being a GP is getting to do lots of different things.
EE: It was probably about five years ago that I discovered that dentists could be a part of sleep apnea treatment, and I started in that because I really like to sleep myself.
MD: That was the attraction? You love to sleep, and you want to help other people sleep as well? We make a lot of snoring and sleep apnea appliances here. For a dentist’s first case, we tend to see the doctor and patient names are matching. So they’re probably making one for themselves.
EE: The guinea pig.
MD: As I got involved with it, I noticed that it was kind of this weird area of health care, where doctors didn’t really learn anything about it in medical school, and dentists didn’t really learn anything about it in dental school, and these poor people suffering from obstructive sleep apnea are kind of caught in between the professions. Dentists stepping in with oral appliances is a great solution for tackling this problem and treating mild to moderate obstructive sleep apnea. When you first got involved, what were your very first steps? Did you make yourself an appliance?
EE: I think my husband wished I would make myself an appliance; there are a couple of videos floating around social media right now of me snoring. I knew there was more to it than taking impressions and handing over an appliance. I knew that we were treating a medical condition, so I didn’t want to mess around with appliances before I understood sleep apnea. I started out with Kent Smith’s course down in Dallas. My dad came with me. He had retired, but he just loved dentistry so much that he decided to come with me. I was like, “OK, as long as we don’t share a room.” But I’m cheap, so we did. It was miserable, because he snores. He had snored his whole life. So as part of the course, we did a home sleep test. He ended up having severe sleep apnea. The scariest part was seeing his heart racing all night long. He got up to 139 beats per minute. That’s a heart rate you’d see during a workout. It scared me because he was supposed to be resting, but his body was working overtime. He was running a marathon without the benefits of running a marathon.
MD: What did your mom say? They had always thought it was just snoring.
EE: Yeah. “It’s normal. Dad makes noise.” We’d go camping in the summers, and it was miserable. I like my sleep, and he’d interrupt it. As part of the course, there was an appliance made, and he didn’t know what the heck he was doing when he set it. It wasn’t necessarily in the proper position, but even that first night, his heart was resting and he was quiet. My mom actually thought he was dead the first night because, for the first time ever, he was quiet.
MD: She was calling the paramedics over every night for the first week or two and checking his pulse?
EE: Well, she’s a nurse, so she’d be able to resuscitate him.
MD: Of the tens of thousands of sleep appliances that Glidewell Laboratories made last year, I would guess that the vast majority were prescribed without a sleep study. I think it’s one of the things that holds dentists back, this idea of having to send patients to a sleep lab or send them home with a device to wear. But it’s really not that big a deal, sending people home to wear one of these at-home sleep tests.
EE: It’s really not, and the potential for the average practice is huge. I get at least two consults a day just out of hygiene appointments. There was a study of a hundred people sent for sleep studies where 30% of them didn’t go. The whole reason they didn’t go was because they didn’t want to wear a mask, or because they didn’t want to sleep overnight. Well, guess what? If you remove those hurdles, your patients are all of a sudden like, “OK.”
MD: Yeah, it’s not a big hurdle to send them home with that because it’s such a comfortable way to do it. If you’re able to get two referrals out of hygiene a day, your hygienists must be familiar with what to look for in these patients?
EE: Yeah, screening is paramount. The hygienists know what medications to look for: high blood pressure medications, acid reflux medications. We check blood pressures all the time. There are a lot of dental clues, too: high-arch palates, mouth breathing, acid erosion, scalloped tongue, and small airways. You could also change your health history form to ask if a patient has had sleep apnea, but patients aren’t always as in-tune with their health as they should be. We do ask if they snore, and a lot of patients will say, “Uh, no, I don’t, but my wife says I do.” Or we’ll ask, “Do you feel refreshed when you wake up?” And they’ll look at us like, “Are you supposed to?” Well, yeah, you are. What I really like are the faxed-over referrals because the patients have usually met their deductible, they’re diagnosed, and they’re desperate for help.
MD: Where are they coming from?
EE: Physicians, primary care, nurse practitioners, sleep physicians. As soon as you get in front of physicians, or even treat some of them, it’s amazing how many referrals you can get.
MD: Did you actively go out and kind of court these different groups in order to educate them?
EE: I like that word: “Court.” As soon as you can get face to face with them, they see that they really don’t know a whole lot about sleep apnea, or how to screen for it. They don’t ask those questions. They put their patients on medications for high blood pressure or Type 2 diabetes and send them on their way, when a sleep study should be a part of the diagnosis. Making doctors aware of that has been really fun. You do have to hit the pavement, but it’s fun for me. I put my handpiece down and put my stethoscope on.
MD: When I was practicing with Todd Morgan at Scripps Encinitas, there was a monthly sleep meeting at the hospital where everybody involved with sleep medicine would get together and watch some of the surgeons show slides of their UPPP surgeries and be shocked. It was kind of funny how it would start with CPAP, and then it would go through various levels of surgery and Pillar® implants (Pillar Palatal; Dallas, Texas) and all kinds of things; and then, when everything else had failed, after the doctors had hacked and cut this person all apart, a dentist might be asked to do the “super aggressive” treatment of taking two alginates to make a sleep appliance. Starting with the dental treatment is really doing patients a favor. I don’t think anybody disputes CPAP as the gold standard of treatment, as long as the patient can tolerate wearing it. Have you ever tried sleeping for a night with a CPAP mask on just for fun?
EE: I tried for about five minutes.
MD: You made it that long? That’s good.
EE: I have one here at the office. I’ve had my staff try it and I tell them it’s the alternative to sleep appliances. Everyone reading this knows that dentists aren’t just tooth mechanics anymore. Oral health is tantamount to total body health. Sleep appliances are just another tool in our kit to help people. Dentists might be worried that they’re not 100% successful, but they’re thinking like a dentist. Do you think the ENT lost sleep by charging for a $10,000 surgery that didn’t work at all? A surgery that put the patient in all of this pain? You’re not putting your patients in pain, and you’re not charging that much, so you can sleep at night. See? I’m all about good sleep.
Dentists aren’t just tooth mechanics anymore. Oral health is tantamount to total body health. Sleep appliances are just another tool in our kit to help people.
MD: It just seems logical to me to start with the most conservative, least invasive treatment first. You could make a good argument that the least invasive treatment is CPAP, if you can tolerate this air being blown through your airway all night long; and then the second-least invasive would be an oral appliance; and then work your way up if those two don’t work. Roughly how many appliances are you making a month now?
EE: We’re probably averaging about 30 appliances a month. That’s in addition to general dentistry.
MD: What are your favorite appliances?
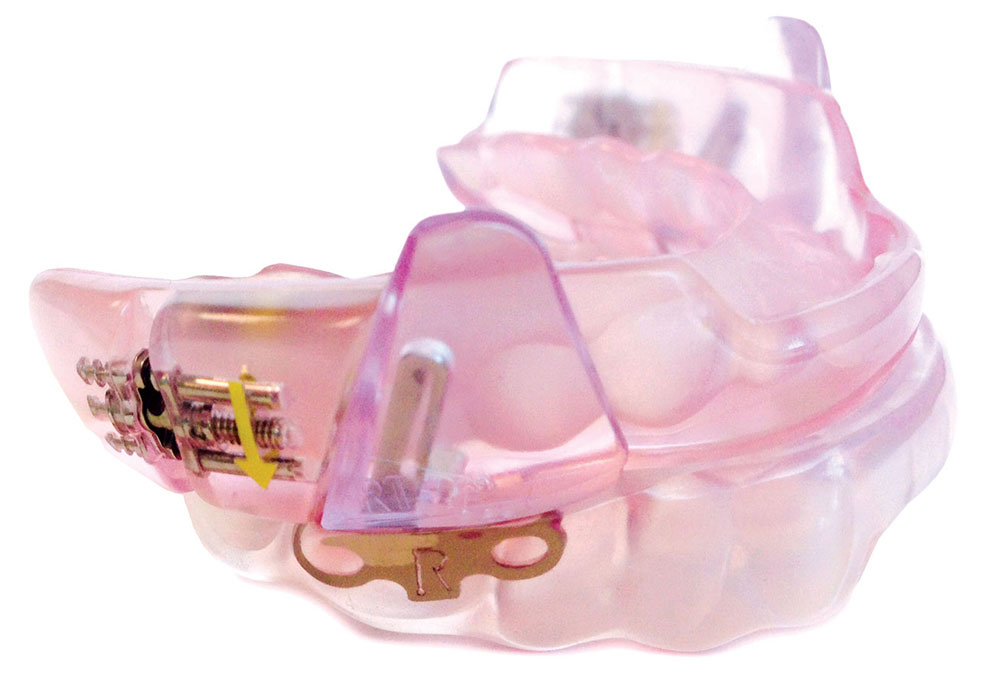
EE: I’ve really been using a lot of the dorsal fin appliance from SomnoMed (Frisco, Texas), as well as Narval™ CC (ResMed Corp.; San Diego, Calif.), which is a CAD/CAM-milled, biocompatible, laser-sintered nylon; virtually indestructible, very comfortable. And of course Medicare doesn’t cover those, so I love the Herbst® (SomnoMed) for my Medicare patients.
MD: What is the Medicare rule for covering an appliance? What does it need to have?
EE: Telescoping hinges.
MD: Telescoping hinges. That’s right! That’s the exact term.
EE: Yeah, what’s interesting is there is a guy out of Utah that sends patients an impression kit, has the patients take their own impressions, and delivers what is basically two bleach trays with a fabric fastener and telescoping hinges on the side. And that’s Medicare-approved.
MD: If you put some lines on there, you can use the fabric fastener to titrate it, I guess. Yeah, that Narval appliance is fantastic. It’s really well thought-out. It’s probably the most expensive one out of all the ones you order, I would guess.
EE: Hey, I’ve got good taste. But we’re getting medical insurance coverage for it. To me, it’s not my bottom line; it’s what the patients are going to wear and have a good experience with. It’s been really fun integrating this into my practice and having some good months because of it.
MD: It’s interesting, I’ve been hugged by more men as a result of this than anything else. They say things like: “I’m not falling asleep every day driving home from work”; “I now believe I’m going to be alive to see my two daughters get married”; “I forgot what it felt like to feel good. I felt like crap for the last 15 years, and I thought that’s how everybody felt.”
EE: Yeah, they just lived with it.
MD: You’ve seen that same kind of reaction?
EE: Oh, yeah. Again, I’m in a small community, so we’ll go to a restaurant, and I’ll get hugs from a wife and husband, and they’ll tell all the friends they’re sitting with that I saved their life and saved their marriage. My husband will see this from a distance, and as soon as I come back to the table, he goes, “That was a sleep apnea patient, wasn’t it?” Your regular dental patients love you, but it’s just not the same.
MD: Yeah, it’s not the same. Do you feel like this aspect of dentistry — treating OSA — could be good for a doctor who suffers from back pain caused by routine procedures like prepping teeth or endo?
EE: I sure do. I have all sleep apnea on certain days, and I come back home just refreshed and rejuvenated. There are definitely a lot of hoops to jump through with medical insurance and all that, but it’s worth it for me because I love it.
MD: It just seems like lower stress as well, even though there’s complicated paperwork. Your staff has probably been well-trained on how to get medical insurance reimbursement for these appliances.
EE: I’m all about delegation.
MD: Did you have any exposure to OSA or snoring treatment at Creighton?
EE: Not at all. I keep hoping that maybe they’ll get it in there at least a little bit.
MD: It just seems like a real disservice to patients. I feel that we are well-qualified, especially since we’re going to be seeing them twice a year anyway if they’re already dental patients. So out of all your patients over the last five years that did a home sleep test, what percentage do you think would end up benefiting from an appliance?
EE: That’s hard to guess. We know the average is one in four men and one in 10 women have sleep apnea. And then there are primary snorers, because when they include primary snorers in studies with oral appliances, their fatigue has gone down quite a bit. When you get over the age of 50, it’s up to 50%, and we have a pretty aged population here. So it’s hard to judge, but I have quite a few patients.
MD: What’s your favorite OSA appliance for an edentulous patient?
EE: I do make a Herbst, usually acrylic. My partner places implants, so if their dentures aren’t fitting well and we want to get a better-stabilized appliance, we can do implants for them.
MD: The other area of dentistry that I know you’re very involved with is orthodontics. I know that you love doing Six Month Smiles® (Six Month Smiles LLC; Scottsville, N.Y.). Tell me a little bit about how you originally got interested in doing Six Month Smiles.
EE: I think I got about as much ortho education as I did sleep apnea education in dental school. I did Invisalign® (Align Technology, Inc.; San Jose, Calif.) for a while, but it was very frustrating. It wasn’t until I became my own Invisalign patient that I realized that I needed to do something different. I was never really satisfied with the results or the process; even on myself, I just took them out. I’m the most noncompliant patient you could ever meet. Do as I say, not as I do.
MD: I did it in the opposite order. I did the traditional ortho first and then the aligners after that. In America — even in Idaho — there’s such an instant-gratification mindset. It’s really difficult to get adults to commit to something for two years. Kids do it because they don’t have a choice. They do what their parents say.
EE: And because their peers are all doing it. So I went and took the Six Month Smiles course and absolutely fell in love with it because you can control the teeth so much more. You can move them faster, and patients don’t mind them. I’ve gotten some spectacular results. A lot of patients will say they like their smile if I ask; but if I ask about a specific tooth, they’ll say they hate that tooth, and it’s because they think they need to go get metal braces for two years to fix it. They’ll just shut it out of their mind. I just fixed a diastema on a 62-year-old man with the biggest Idaho beard — you hardly see his teeth — who wanted to fix the space. His wife said she never realized how much it bugged him, and was really glad that he finally did something about it.
A lot of patients will say they like their smile if I ask; but if I ask about a specific tooth, they’ll say they hate that tooth, and it’s because they think they need to go get metal braces for two years to fix it. They’ll just shut it out of their mind.
MD: When you’ve had your eyes opened to this type of adult orthodontics, you begin looking at teeth in a slightly different way. You begin noticing that almost every adult has lower anterior crowding and other small issues. So how did you get started? Where was your first training class, and when was it?
EE: It was in Chicago with Tony Feck. And I’ll tell you what; it’s perfect for general dentists and easy to do with assistants. I can’t sit down for an hour and place brackets. I just don’t have the time, and that’s not profitable. So it’s just a great system in which they give you the trays with the preset brackets, and you can bond the brackets indirectly. The wires are white, and the “donuts” are clear, so they don’t catch your eye like traditional braces. Patients really love that. I have at least one member of my staff in Six Month Smiles at all times.
MD: Whether they need it or not, you’ve got one of them in it?
EE: Pretty much.
MD: When I was doing ortho, we were placing brackets on teeth manually using measurements and a positioner to line them up with the long axis of the tooth and get them properly centered. To a large extent, that placement determines how successful your result is going to be. It’s an indirect method with Six Month Smiles. You have somebody — a trained technician — putting the brackets on a study model out of the mouth without any lips, tongues or saliva getting in the way, and then doing a thermoformed tray over that and sending it to you. All you need to do is be able to get acid-etch in the middle of the tooth, rinse it off, apply bonding agent, put it down with the cement, cure it, and peel it off, and instantly everything’s in the right position.
EE: And everything is esthetic.
MD: And six months for them is not a huge commitment. Do you guarantee that?
EE: We say, “Would you like to have straight teeth by your next cleaning?” Which is a good way to put it. Sometimes they’re stubborn teeth, sometimes it’s a more advanced case, and if it is more advanced, then I’ll let them know. But for the most part, it’s ortho relapse or some crowding that someone’s always hated, and it’s just unraveling those teeth and getting the nice arch forms that the wire provides you. So we always say about six months.
MD: Are you doing anything for retention at the end of these cases? Removable? Fixed? What do you find most adults like?
EE: Yes, the patients all need to sign off on the retention knowing that it’s vitally important when we’re done. We have a new braided wire system from Six Month Smiles called Ortho FlexTech® (Reliance Orthodontic Products, Inc.; Itasca, Ill.) that I place on the maxillary if I can, or if not, at least on the anteriors of the mandible; and then clear Essix® (DENTSPLY Raintree Essix; Sarasota, Fla.) retainers that I make in-house. You can also do an indirect lingual wire that the lab at Six Month Smiles makes and places for you with the trays. Again, it’s a no-brainer — you just place it. But I don’t like to wait. I just want to take them off and get my patients smiling again. You can get tears occasionally with that, which is really rewarding.
MD: The day the hardware comes off is such a great day.
EE: Actually, I have a photographer across the street, and he does a free photo session for them afterwards.
MD: Oh, that’s a great idea. How many cases did it take before you really started to feel comfortable with it?
EE: I did my first 10 cases on patients that I knew personally. I treated them at a discounted rate because during training you can buy a pack of 10 or so and get a discounted lab fee. But after that, there’s so much support on the forum for those new to it; in fact, I’m a mentor on the forum now. They really do help you through it, and it’s a really nice system.
MD: Can you compare the learning curves of Six Month Smiles and getting involved with snoring and obstructive sleep apnea?
EE: For snoring and sleep apnea, it’s a matter of learning all of the information that’s out there; for Six Month Smiles, it came down to my assistant and I getting familiar with the protocol. It really doesn’t take a whole lot of time. The learning curve would be more treatment planning and knowing what cases you can and can’t do, and what to tell your patients to expect.
It really doesn’t take a whole lot of time. The learning curve would be more treatment planning and knowing what cases you can and can’t do, and what to tell your patients to expect.
MD: I’m sure in the course, there’s equal emphasis on what cases to treat and what cases not to treat.
EE: And which patients — as far as personalities — to treat. Do you really want to be married to them for the next six months?
MD: Ah, well, six months. I used to do it for two years. It’s really nice to be able to do it in six months, so you can see the goal and at least have an idea of when the treatment is going to end.
I think you have a real willingness to jump in and learn something new. And if you don’t like it, then you just don’t do it anymore, right? It’s not a lifelong commitment that you’re making.
EE: Well, yeah. You should never do anything if profit is your only motivation. And these areas are ones that I absolutely love doing, so I don’t mind the learning curves. I love doing braces, and changing smiles and changing lives.
MD: Would you also classify the Six Month Smiles treatment as being less backbreaking than, say, typical general dentistry?
EE: Definitely. I sit down, look at it, and do an overview. I’m not putting in the wires or the “donuts.” So yeah, I’m not bending over my patients all day.
MD: That’s the experience I think most of us had when we were kids going through ortho. When I visit my orthodontist friends, I see the staff doing pretty much everything after the diagnosis and treatment planning. It makes me jealous of orthodontists. And then I get just flat-out angry with orthodontists when they want four bicuspids extracted, and they don’t even have the technical fortitude to do the extraction themselves.
EE: They probably don’t even have anesthetic.
MD: I’ll be happy to ship some over to them along with some forceps. They’re going to charge $5,500 for an ortho case where their assistants are going to do 95% of the work, and they want me to take out four perfectly healthy teeth on a 15-year-old for $150 each?
EE: Without breaking off the palatal root tip.
MD: Yeah, exactly. No, I refuse. They can do it themselves. Do you have Six Month Smile-only days, kind of the same way that you have obstructive sleep apnea-only days?
EE: Yeah. I tend to do them on the same days because I can have my assistants line it up, and I can go back and forth.
MD: So after that first Six Month Smiles course you took, did you come right back and start treating patients?
EE: I did. I had patients lined up before I even went. Once I got all the information and informed consents and all that, I was out the gate, ready to go. I did go back to check my notes a few times, but I felt prepared.
MD: It’s amazing to see how easy it is to move teeth. Do you have any advice for dentists who have thought about getting involved with either of these areas of dentistry, but have been nervous to do it?
EE: There are a lot of great courses out there for sleep apnea, and I think they are a great place to start. There’s a lot to learn; it’s a lot more than just making an impression and giving your patient a piece of plastic. I’d be more than willing to email those that might want more information on where to go and how to get started. For Six Month Smiles, there are a ton of courses with great instructors all over the country. I’ll be attending one in Vegas this year. My favorite part is that all of my colleagues offering this service are in the same boat. No one is competing against each other, so it’s a great community.
MD: It’s all about making things easier on the patient and the dentist. And the more dentists in your community who do this, the more legitimacy it gets. It’s kind of like how CEREC® (Sirona Dental Systems, Inc.; Charlotte, N.C.) was the only chairside CAD/CAM system for decades, but now that there’s four or five other commercially available ones, they don’t seem like such crazy renegades anymore. You going out and sharing this raises the water for everybody.
EE: Well, that’s why I loved your lecture at the Idaho State Dental Association meeting about digital impressions and how it made you a better dentist. I’m kind of disappointed you showed some of my preps and impressions that I sent down to Glidewell, but that’s OK.
MD: I spared you by not saying your name. Usually, I do that. I show a bunch of bad impressions, and then say, “Now, the interesting thing is all of these impressions are from dentists sitting in this room.” And the room goes totally quiet. Everyone who was talking or chatting on their phone just stops because they’re all terrified of seeing their own bad impressions. At which point I let them know that I’m just kidding.
I think it’s fantastic that you’ve embraced these two areas of dentistry and really incorporated them into your practice to help make it more successful. I speak with a lot of dentists who say their practices are down and they’re looking for a way to bring it up. I know you’re up, and a big part of the reason you’re up — besides your personality — is the ability to offer patients what they want. They want to feel good when they wake up in the morning. They don’t want to fall asleep when they’re driving home. They don’t want to hear their husbands snore anymore. They’d like to have straight teeth and then bleach them afterwards. And these are all things that are more appealing than scaling and root-planing and some of the other things that we have to do. These are things that people want, and that’s part of the genius of it all.
You mentioned if someone wanted to email you, you’d be happy to email back and forth. Can you give your email address for anybody who wants some more information?
EE: Sure! It’s erinelliottdds@gmail.com.
MD: Well, Erin, thank you so much for your time today. It was a pleasure getting to spend some time with you up in Idaho and then speaking again with you today. Hopefully, you’ll be an inspiration to dentists interested in these areas. Thanks so much.