Simplifying Accurate Evaluation: Adjustment of Proximal Contacts

BACKGROUND
Very little information is taught in the dental school curriculum about adjusting tight proximal contacts. In fact, very little is written about this subject in the research literature. Dörfer, et al.1 concluded that proximal contact is a manifestation of location, tooth type, chewing and time of day. Furthermore, they concluded that the strength of the proximal contact is a physiological entity of multifactorial origin.1 Proximal contact strength was lower in the maxilla as compared to the mandible. Within the jaws, the lowest proximal contact strength was measured between the canine and the first premolar, whereas the strongest was measured between the second premolar and the first molar. Chewing increased the proximal strength in the maxilla, but there was no change in the mandible. The proximal strength increased significantly from morning to noon and then decreased in the afternoon.
Newell, et al.2 found that although food impaction is generally associated with open contacts, food impaction can also occur in interproximal sites when contacts are tight. They reported that the lack of adequate escape grooves is the primary cause of food impaction. They also stated that uneven marginal ridges and prominent opposing cusps have also been implicated. They found that one or two occlusal adjustments to establish even marginal ridges, reduce prominent cusps, and establish escape grooves eliminates food impaction problems in 13 out of 14 patients (92.9%).2
IN THE AUTHORS' EXPERIENCE
In our clinical experience (more than 60 years combined), tight proximal contacts can be multifactorial. Causes include parafunctional habits such as bruxing and/or clenching (nocturnal and diurnal), occlusal discrepancies, crowding, malposition of teeth, post-orthodontic treatment, and iatrogenic dentistry. Tight proximal contacts can cause not only food impaction, but migration of teeth with consequent crowding and/or repositioning of teeth that can change the occlusion, throwing off the musculature and causing myofascial and temporomandibular joint dysfunction.
Tight proximal contacts can cause not only food impaction, but migration of teeth with consequent crowding and/or repositioning of teeth that can change the occlusion.
IATROGENIC CAUSES
Existing iatrogenic dentistry that can cause tight proximal contacts can present in multiple clinical situations. This could include poor orthodontic treatment, poor fixed/removable prosthetics, and improperly done operative dentistry. In most cases, iatrogenic dentistry needs to be replaced. This replacement dentistry obviously has to be done properly so the iatrogenically caused problem is not repeated.
When replacing existing dental restorations or restoring virgin teeth, proximal contacts need to be restored to appropriate pressure/tightness. There is no true definition for appropriate pressure or tightness of physiological proximal contact other than the fact that there is in fact contact between two teeth. Dörfer, et al. measured contact strength with a calibrated 0.05 mm thick metal strip. The strip was attached to a metal holder that was attached to a strain gauge. As stated earlier, contact strength varied between teeth, arches and with function.1 Dörfer, et al.1 may give us a guide as to the average contact strength, but in a clinical situation it is difficult to determine if the contact strength is 3.61 ± 1.77 N.
There is no true definition for appropriate pressure or tightness of physiological proximal contact other than the fact that there is in fact contact between two teeth.
Kim and Suh3 described proper proximal contact as microscopic clearance or passive contact to relieve pressure between the proximal contact surfaces of indirect restorations and adjacent teeth. The relief of pressure was referred to as interproximal relief. Accurately restoring interproximal space is achieved by properly restoring the deflecting contours and occlusal anatomy of the teeth, thus preventing food impaction. By properly restoring interproximal relief, complete marginal seating of an indirect restoration is achieved and occlusal interferences are prevented.3
In a clinical situation, the patient will usually tell the practitioner if the contact is too tight. Traditionally, the other clinical methods of determining if the proximal contact is too tight have been to pass waxed or unwaxed floss between the contacts, using a 0.05 mm shim stock as a guide, or by placing very thin articulation paper (or articulating film) between the contacts.
In this article, the authors are presenting a clinically practical method for determining accurate proximal contact strength using ultra-thin abrasive diamond dental strips when seating an indirect laboratory-fabricated or CAD/CAM restoration.
TECHNIQUE FOR SEATING AN INDIRECT RESTORATION
Instruct your dental laboratory technician to refrain from adjusting the proximal surfaces of the adjacent teeth on the final cast, in order to retain the natural contour and space between the teeth. If scraping is required, do not exceed 0.10 mm of proximal contact thickness.
First, evaluate the fit, margin, occlusion and proximal contacts of the completed restoration on the articulated model. If fabricating with CAD/CAM technology, you will usually not have a physical working model and will need to evaluate the restoration in the mouth.
Next, place the restoration on the prepared abutment tooth and evaluate clinically the marginal fit with an explorer. If margins are fit, check the proximal contacts using ultra-thin abrasive dental strips to find the heavier proximal contact on either the mesial or the distal. Pressure is felt more distinctively on the strip with the abrasive diamond surface because of friction. The side with more pressure against the strip is the heavier proximal contact side. If the margins are open, and the restoration is not seating properly (so that the restoration is inserted in parallel to the path of insertion), the side with the less-open margin is the side with the heavier proximal contact (Fig. 1).
Adjust the heavier proximal contact side first by placing the abrasive diamond dental strip into the interproximal space with the abrasive side facing the fabricated restoration. Hold the restoration between the thumb and index finger and press it gently onto the prepared tooth while moving the diamond strip buccolingually five to six times. One should feel the restoration settling onto the abutment tooth as the abrasive diamond dental strip relieves the pressure at the proximal contact.
Now pass the abrasive diamond dental strip through the opposite proximal contact and adjust that side, if needed. When more pressure is detected on one side or the other, pass the abrasive diamond dental strip buccolingually a few more times until there is light resistance. When equal light resistance is felt in both interproximal spaces, accurate proximal contact adjustment of the restoration is complete.
You may now cement the restoration with your choice of cement. Remove the excess cement with an explorer. Gently pass the serrated dental strip buccolingually (do not press down) to cut and clean out the remaining cement in the distal and mesial interproximal spaces.
Polish the proximal surfaces of the restoration with the ultra-fine finishing strip by gently passing it through the mesial and distal proximal surfaces to polish and restore to a natural fine finish. Accurate proximal contacts can be confirmed when the ultra-fine finishing strip passes through the interproximal contacts with light resistance. Dental floss can be then passed through the interproximal contacts with heavy resistance, snapping in and out. This completes the placement of the restoration.
CASE REPORT
Diagnosis and Treatment Planning
A 55-year-old male patient came to the office complaining of a decayed tooth. Tooth #8 presented with large bilateral Class IV composite restorations that were loose and becoming dislodged due to recurrent dental caries. After examination, an all-ceramic crown (VITA® [VITA Zahnfabrik; Bad Sackingen, Germany]) was recommended as the treatment of choice and the patient consented.
Clinical Treatment and Laboratory Fabrication
The tooth was prepared for the crown; a vinyl polysiloxane impression (Aquasil Ultra [DENTSPLY Caulk; Milford, Del.]) was taken and sent to the dental lab for fabrication. The dental laboratory technicians were instructed (1) to adjust the proximal contact surfaces of the adjacent teeth on the mesial and distal of the final stone model with two strokes (each stroke reduces 0.01 mm) using a lab diamond dental strip (Clear, LAB Diamond Strip [ContacEZ; Vancouver, Wash.]), which scraped 0.02 mm on each side (Fig. 2), and (2) to restore accurate occlusion.
Crown Delivery Appointment
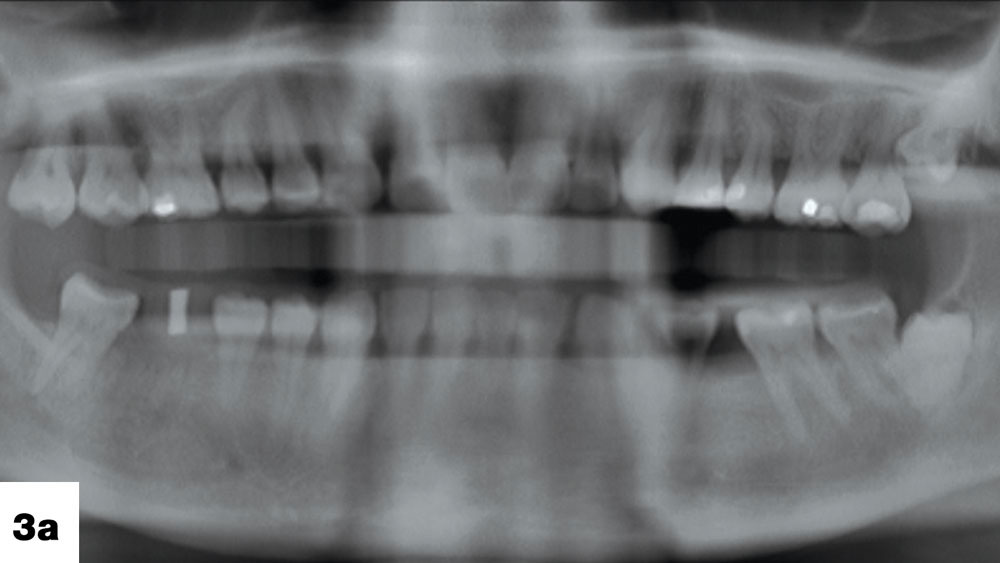
After the patient’s provisional crown (Nu-Crown™ [Efficient Dental Technologies; Springfield, Ore.]) was removed, the porcelain crown was tried on the prepared tooth. The proximal contact was found to be slightly heavy and needed adjustment (Fig. 3).
The proximal contact adjustment was performed before cementation as follows: First, a diamond dental strip (0.06 mm, black [ContacEZ]) was inserted into the distal interproximal space with the abrasive side facing the porcelain crown. The strip was passed through the interproximal space buccolingually a few times (Fig. 4). Next, the strip was moved to the mesial interproximal space and passed through a few times. It was found there was more pressure on the strip in the mesial interproximal space indicating a heavier proximal contact on the mesial of the crown. Finally, the strip was passed through the mesial interproximal space an additional six times (Fig. 5), equalizing the light, accurate interproximal pressure on the distal aspect. Proximal contact adjustment was completed.
The crown was then cemented with a glass ionomer cement (Fuji I® [GC America; Alsip, Ill.]) using finger pressure, and excess cement was removed after setting. The excess cement in the interproximal space was removed using a serrated dental strip (0.035 mm, white [ContacEZ]) (Fig. 6). A waxed dental floss (Reach® Mint Waxed [Johnson & Johnson; New Brunswick, N.J.]) was used to clean the interproximal spaces.
After excess crown cement was cleaned off, a final polishing strip (0.04 mm, gray [ContacEZ]) was used to confirm interproximal relief.3 The strip was passed through the mesial and distal interproximal spaces with light resistance, confirming accurate proximal contact (Fig. 7). Using a friction-grip silicone mini-point (Brownie Mini-point [Shofu; San Marcos, Calif.]), minimal occlusal adjustment was performed finishing the seating procedures. The patient commented that there was no pressure with the new all-ceramic crown, and that he felt as comfortable as if it was his own tooth. He said, “I don’t feel the new crown in my mouth!”
DISCUSSION
When a clinician receives a finished crown from the dental laboratory, the crown usually presents with heavy proximal contact bilaterally. The clinician not only needs to adjust both contacts but also needs to determine which contact is heavier. It is usually a guessing game as to which contact is heavier. Many times the assumption is wrong, resulting in an open proximal contact on one side, with the heavy proximal contact left intact on the opposing side. The crown then has to be sent back to the dental laboratory for an addition to the open contact, or sometimes a complete remake of the restoration. Using an ultra-thin diamond dental strip (0.04 mm to 0.06 mm), the heavier contact side is easily detected and reduced. By applying this protocol, a clinician cannot make a mistake, thus ensuring an accurate proximal contact every time.
Traditionally, adjustments of proximal contacts of indirect restorations (crowns, inlays or onlays) are performed by the clinician holding the restoration between his or her fingers, using an indicating medium such as articulating paper and reducing the heavy contact with a rotary instrument. Small restorations such as crowns, inlays or onlays are not only difficult to hold, but they are also difficult to see. In addition, they frequently get caught in the folds of the glove material, ending up on the floor. Furthermore, incremental adjustments with this method require multiple trials. Taking the restoration in and out of the patient’s mouth can be quite tedious and time-consuming for the clinician. This can also be very uncomfortable for the patient. In a clinical situation, the patient will usually tell the practitioner if the contact is too tight.
Traditionally, another clinical method to test for proper proximal contacts is to pass waxed/unwaxed floss between the contacts. Clinically, this can be quite subjective and results will vary depending on the operator. In contrast, using an ultra-thin diamond dental strip, interproximal relief is easily confirmed. Ideal proximal contact of restorations can be achieved quickly and accurately, enhancing patient comfort and functionality immediately upon final cementation.
Ideal proximal contact of restorations can be achieved quickly and accurately, enhancing patient comfort and functionality immediately upon final cementation.
CONCLUSION
When seating indirect restorations, interproximal relief should be restored as it exists in natural dentition. An excellent method for clinicians is to use ultra-thin diamond dental strips to achieve definitive interproximal relief and accurate proximal contact. The benefits of using an ultra-thin diamond dental strip in proximal contact adjustment include: achieving complete marginal seating of indirect restorations easily, quickly and safely; minimizing the need for occlusal adjustment; preventing adjacent tooth movement due to excessive interproximal pressure; eliminating the tedium of using articulating films and rotary instruments; and enhancing patient comfort and satisfaction with the restorative result.
Dr. Kim is in private practice in Vancouver, Washington. He lectures at dental scientific sessions, dental seminars and study clubs. He can be reached via email at dankimdds@gmail.com.
Dr. Rothchild is in private practice in Chicago, Illinois, and Durango, Colorado, and is assistant professor of surgery at Rush University Medical School, Chicago, Illinois, and associate professor of dental medicine emeritus, Capital University of Integrative Medicine, Washington, D.C. He can be reached at jrothchild@aol.com.
DISCLOSURES
Dr. Kim is the inventor and founder of ContacEZ Restorative Strip System and has financial interest for ContacEZ, LLC. Dr. Rothchild reports no conflicts of interest.
Reprinted by permission of Dentistry Today. ©2010, Dentistry Today.
References
- ^Dörfer CE, von Bethlenfalvy ER, Staehle HJ, Pioch T. Factors influencing proximal dental contact strengths. Eur J Oral Sci. 2000 Oct;108(5):368-77.
- ^Newell DH, John V, Kim SJ. A technique of occlusal adjustment for food impaction in the presence of tight proximal contacts. Oper Dent. 2002 Jan-Feb;27(1):95-100.
- ^Kim DS, Suh KW. A proximal contact adjustment and interproximal relief method. J Prosthet Dent. 2007 Apr;97(4):244-5.