Does Your Team Know What You Do?

Oftentimes we as treating clinicians can suffer from a little bit of tunnel vision. A patient may come in for elective esthetic treatment, and we get so focused on that, we fail to see the broader picture. It is important to remember that every dental case has both esthetic and therapeutic components that must be blended together. This is especially true of facial esthetic treatment cases, as they relate directly to patients’ orofacial and temporomandibular joint (TMJ) conditions.
Here is a case report from one of our American Academy of Facial Esthetics (AAFE) faculty members, Dr. Elizabeth Slocum, who is an outstanding dental clinician and educator with a practice in Cartersville, Georgia. This case is a prime example of blending the best esthetic and therapeutic outcomes possible for our patients. The other lesson to be learned from this case presentation is to ensure that your team knows all of the treatments that you, the dentist, are competent in and able to deliver to patients.
I present Dr. Slocum in her own words:
Andrea has worked with us for eight years now. She is as beautiful on the inside as she is on the outside. She was excited when I decided to take a course on BOTOX® (Allergan, Inc.; Irvine, Calif.) and dermal fillers with the AAFE. Since completing the course, I have treated her for dentofacial esthetics, and she loves the results.
Through a series of events involving Andrea, I learned a valuable lesson about why it is important to make known all of the techniques and treatments that I’ve been trained to provide; a lesson that is doubly important in light of all that I’ve learned from the AAFE, as my employees, like yours, might not realize that dentists are capable of treating patients for facial esthetics, TMJ pain, orofacial and myofascial pain, and headaches and migraines.
Andrea went home from work early one day not feeling well. She missed the next day, too. She came back to work the third day still under the weather. As we spoke, I realized that she had been absent due to a migraine. I was a little shocked that she hadn’t thought of having me treat her migraine in conjunction with the facial esthetics treatment I had already been providing her. She agreed to treatment, and I made some adjustments that would account for her migraine. I treated her glabellar area, frontalis and crow’s feet areas, as well as her masseter and temporalis muscles. I used Xeomin® (Merz Pharma GmbH & Co. KGaA; Frankfurt, Germany) — available from STATDDS for dentists — a botulinum toxin just like and as effective as BOTOX that is more cost-effective and has been reported to have a faster treatment response. She never looked back. In fact, we still treat her for both facial esthetics and her migraines (which are now under control) on a regular schedule.
Figures 1–4 show the before and after of the procedure.
Again, the lesson here is to share all of the procedures that you do with all of your employees. Every time you learn new material, share it with your entire team. I thought I had shared most of what I had learned, but I had really only talked with them about facial esthetics and TMJ pain — not nearly as much about headaches or migraines. We started doing “lunch and learns” by watching some of the video series available from the AAFE. The staff enjoys them, and it opens the door for them to ask questions about any of the procedures that we offer. They really want to know what we do and how to share the information when speaking to patients.
Everything we learn and bring back to the office is basically an unknown to our team members, unless they go to the training with you — which is now something I do routinely. Think back to the first AAFE BOTOX, fillers, TMJ/orofacial pain, or trigger-point therapy live-patient training course you attended or video you watched — or any dental continuing education course for that matter. There’s so much information out there that clinicians can learn. We bring back new and exciting procedures and have all of that information in our heads or on a handout, but your team members will only learn what you share with them.
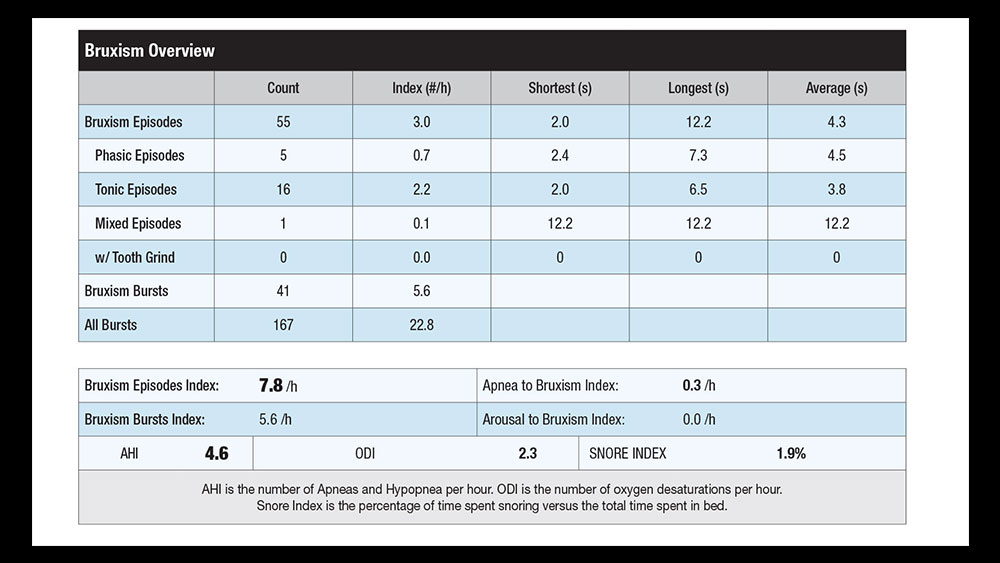
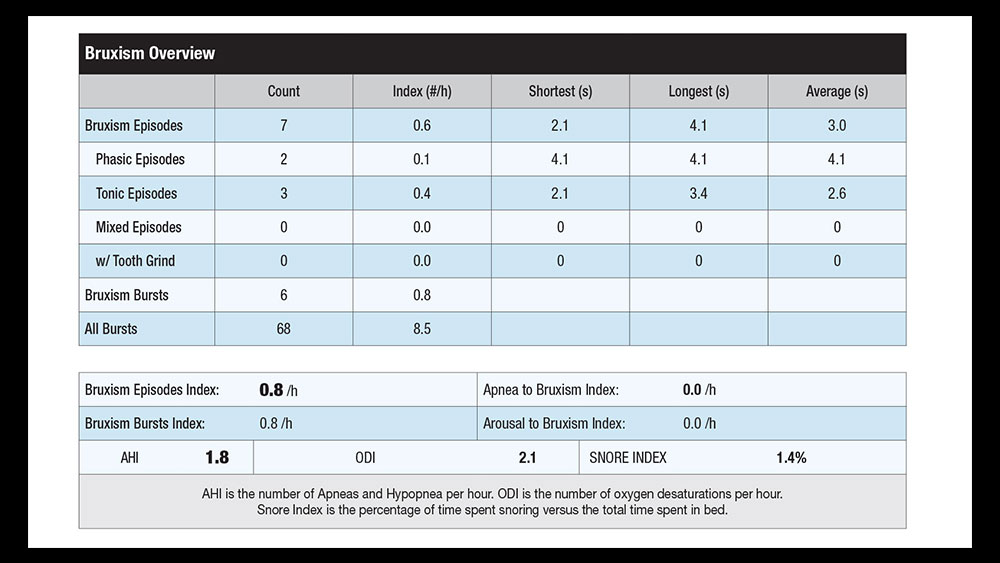
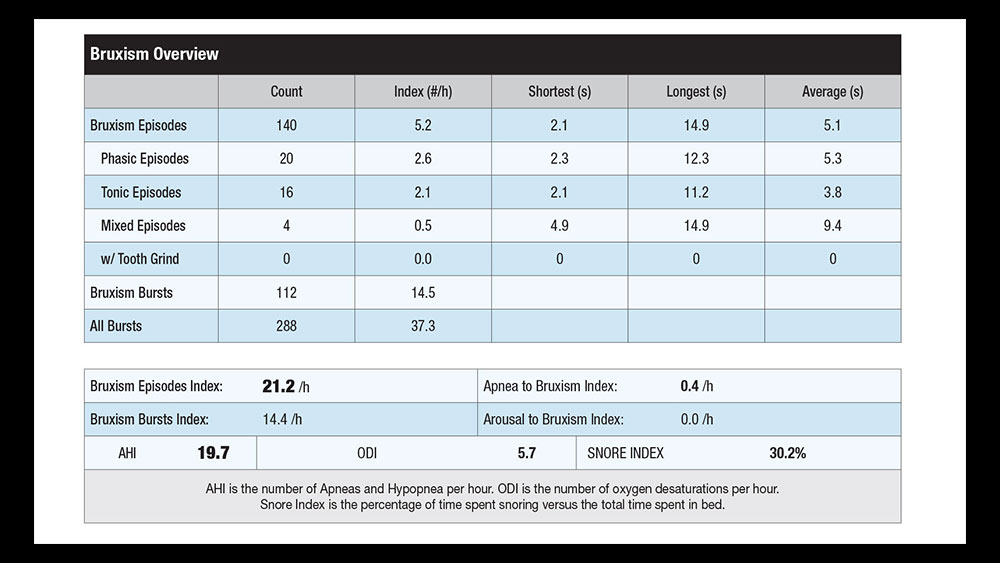
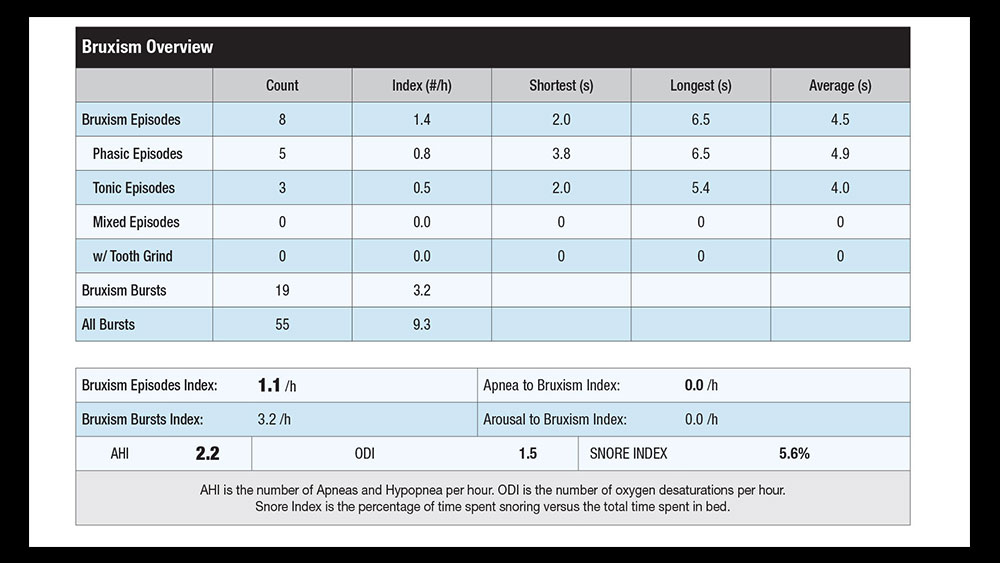
Today, the AAFE uses the STATDDS® Bruxism and Sleep Monitor (STATDDS; Cleveland, Ohio) to establish a baseline bruxism-episodes index number as part of the patient’s initial diagnostics in order to better evaluate and treatment plan bruxism, TMJ pain and orofacial pain cases (Fig. 5). This monitor will also tell us whether or not the patient will have sleep disorders that might be a co-morbid condition or can be the cause of TMJ and orofacial pain.
The results of the STATDDS Bruxism and Sleep Monitor will directly guide the dental clinician as to which bruxism appliance or oral appliance for dental sleep medicine is the best choice for each individual patient (Figs. 6–11).
This article’s two main points are these: First, make sure your team knows all of the services that you are trained to provide. It is time for every dental practitioner to take his or her team along to continuing education, especially when introducing new services to the practice. Second, let’s start obtaining objective data on bruxism, which affects one out of every three patients. I will measure most patients first with a STATDDS Bruxism and Sleep Monitor test and then let the data drive the treatment plan. This is especially helpful in choosing appliances and deciding the correct muscle treatment.
Education — especially live-patient training — is absolutely essential in the areas of bruxism, restorative dentistry, orofacial pain, dental and facial esthetics, dental sleep medicine, and oral appliances. The continued education of clinicians is important so we can ensure favorable long-term restorative prognoses for patients across the span of our careers. Successful restorative, bruxism and orofacial pain treatment has now entered a new era with the use of cost-effective qualitative objective testing, botulinum toxin, and the known relationship of bruxism and OSA. The AAFE (facialesthetics.org) offers comprehensive live-patient training in the areas of botulinum toxin, dermal fillers, frontline TMJ/orofacial pain, dental implants and bruxism/sleep therapy. Get trained today!
Dr. Malcmacher is a practicing general dentist and an internationally known lecturer and author. He can be reached at 800-952-0521 or via email at drlouis@facialesthetics.org.
Disclosure: Dr. Malcmacher is president of the American Academy of Facial Esthetics (AAFE) and is a consultant for STATDDS.
Visit facialesthetics.org for information about live-patient frontline TMJ/orofacial pain training, dental implant training, frontline dental sleep medicine, bruxism therapy and medical insurance, and BOTOX and dermal fillers live-patient training. You can also download Dr. Malcmacher’s resource list and sign up for a free monthly e-newsletter at the site.