Implant Overdentures: A Superior, Cost-Effective Alternative to Traditional Dentures

Denture fabrication is a conventional method of restoring patients who have lost all their maxillary or mandibular teeth. Although this treatment may enhance esthetics and offers some improvement in function, it is inadequate for many patients. Chewing efficiency is drastically reduced.1,2 Plastic on the palate can be invasive, diminish the ability to taste food, and trigger a gagging sensation. Lower dentures are often uncomfortable and loose-fitting, and in many cases move freely about the mouth. The psychological effect of losing all of one’s teeth can be devastating, impacting the comfort, confidence and social interactions of the patient.3,4 These issues should be considered when discussing treatment options with patients.
Fortunately, dental implants can be predictably placed to support an overdenture, providing retention, added stability and an affordable alternative to conventional dentures. Compared to traditional complete dentures, implant-retained prostheses such as the Inclusive® Implant Overdenture (Glidewell Laboratories; Newport Beach, Calif.) excel in producing the bite force needed for effective chewing.5,6 In addition to improved speech and dental function, implant overdentures have been shown to dramatically increase social confidence, comfort and emotional well-being.7,8,9 For patients, the prosthetic stability afforded by implant overdentures elicits a positive psychological response and an improved quality of life.10,11 Delivering these bnefits to the patient is extremely rewarding to the dentist.
Bone loss is arguably the most detrimental consequence of edentulism. Following tooth loss, the bone regresses both horizontally and vertically. As these bone changes occur, prosthetic support and stability decreases, necessitating denture relinings. Further, as bone resorption worsens, support for the mouth and face is compromised (Fig. 1). The effect this can have on facial esthetics and self-esteem is difficult to overstate. By providing the edentulous ridge with continued stimulation, dental implants mitigate the bone loss that occurs in the absence of teeth.12
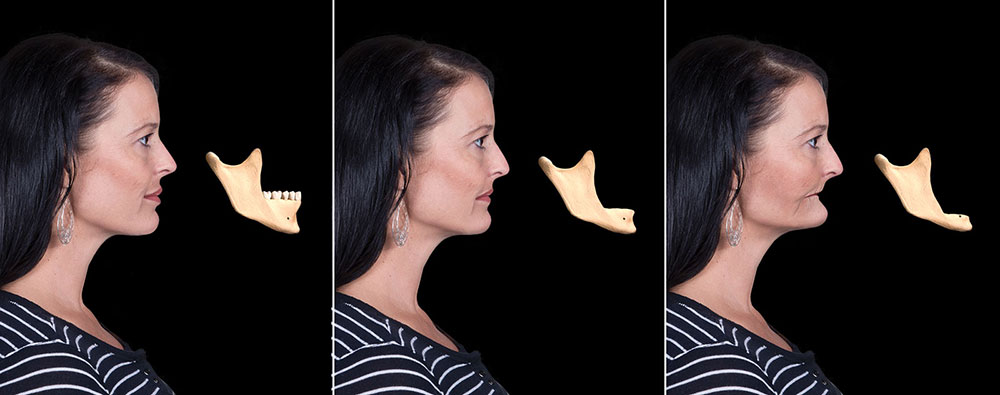
Figure 1: Complete edentulism results in bone loss that can severely impact facial esthetics. This can lead to the gradual collapse of the patient’s vertical dimension as resorption worsens over time.
It has been shown that as many as 75% of denture wearers would have chosen implant treatment had they known about bone loss.13 Many edentulous patients present for treatment because they are no longer satisfied with their existing dentures. Others need new appliances because their old ones no longer fit properly due to bone loss. In comparison, an overwhelming majority of fully edentulous patients report extremely high levels of satisfaction with implant therapy and an improved attitude toward their dental health.14
For practitioners who regularly prescribe traditional dentures, implant overdentures are a logical point of entry for offering this life-changing service. The implant overdenture is a cost-effective solution to complete edentulism and should be presented as one of the primary treatment modalities to edentulous patients. The cost of implants has come down significantly over the years and the surgical protocol has been minimized to the point that implants can be placed promptly and efficiently. Although affordability is dependent on the patient’s desires and wherewithal, the implant-retained overdenture is one of the most economical ways of improving form and function. Further, implant therapy expands the services offered by the practice, increases income and drives incoming referrals due to the higher rates of patient satisfaction.
The Overdenture Concept
Like traditional dentures, implant overdentures are removable appliances that include prosthetic teeth. Unlike traditional dentures, maxillary overdentures are shaped like a horseshoe. This is a godsend for many patients, as the palate of the prosthesis can be eliminated (Figs. 2a, 2b). This affords better comfort, speech and taste. The advantage of the mandibular overdenture is obvious, in that the patient has a stable, retentive prosthesis that does not move around in the mouth. Note that for a small fee, a partial metal framework can be incorporated to lend additional support to the denture teeth and provide an extra measure of durability.

Figures 2a, 2b: Maxillary implant overdentures can be created with a palateless design, providing the patient with enhanced stability, comfort and taste.

Figures 2a, 2b: Maxillary implant overdentures can be created with a palateless design, providing the patient with enhanced stability, comfort and taste.
There are many ways of attaching the overdenture to the implants. One of the most efficient and cost-effective is the use of Locator® attachments (Zest Anchors; Escondido, Calif.), which is the retention mechanism employed by the Inclusive Implant Overdenture. The system includes freestanding abutments, or Locator attachments, that connect to the individual implants. “Denture caps” are embedded in the overdenture and provide retention by seating over and engaging both the internal and external surfaces of the Locator attachments (Fig. 3). The retentive caps come in a variety of strengths and are easily changed out as the parts wear or the patient requests greater retention. By stabilizing the overdenture, these retentive devices improve function and chewing efficiency for the patient.
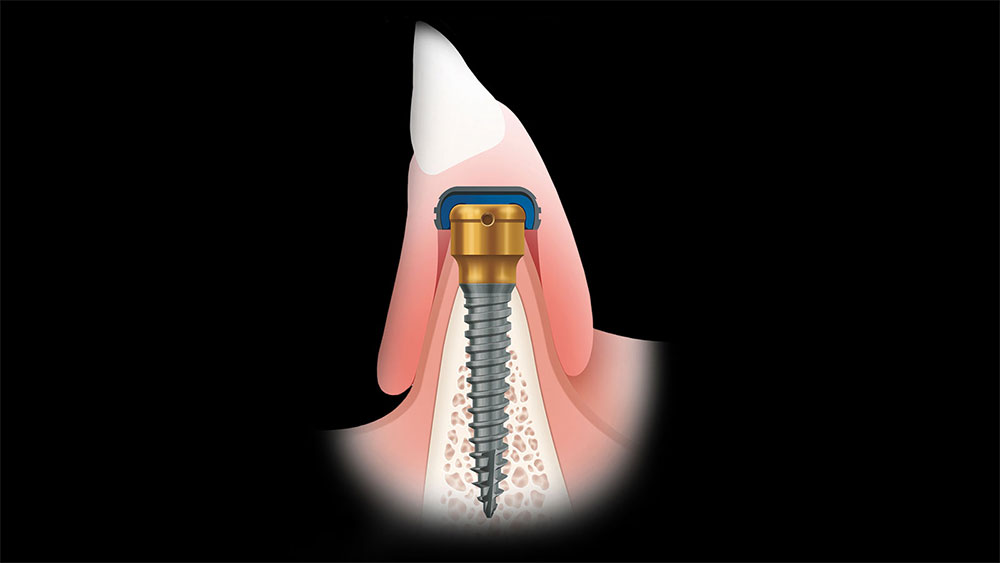
Figure 3: The Locator system holds the overdenture in place via retentive caps embedded in the denture that affix to the specially designed Locator attachment.
Treatment Considerations
The fabrication of Locator Implant Overdentures begins with careful diagnosis and case planning. In many cases, two-dimensional images created using conventional digital radiography are appropriate to determine the vertical height of available bone (Figs. 4a, 4b). However, horizontal bone quantity and anatomic concerns must be determined by other means. These are key considerations not only because avoiding vital patient anatomy is critical, but also because the positioning of the implants greatly influences the final functional and esthetic result.

Figures 4a, 4b: Panoramic radiography was used to assess the vertical bone quantity available to position implants for this patient, who presented with severe periodontal issues and nonrestorable dentition.

Figures 4a, 4b: Panoramic radiography was used to assess the vertical bone quantity available to position implants for this patient, who presented with severe periodontal issues and nonrestorable dentition.
CBCT scanning techniques have improved our diagnostic abilities dramatically, allowing the practitioner to visualize all dimensions of the edentulous bone. Quality and quantity of bone can typically be determined prior to surgical intervention, and the vital anatomy can be specified (Fig. 5). Any bone volume issues or defects can also be determined, as well as implant type, size and shape. Once properly situated within the available bone, endosseous dental implants with appropriate retention designs serve as reliable retainers for overdentures and are proven to provide a positive long-term prognosis.15
The amount of anterior premaxillary bone needs to be determined with conventional radiographs, bone calipers or CBCT analysis. This helps determine the height and width of existing bone in the potential surgical sites. Placement of dental implants in the maxilla may be hindered by the size and position of the right and left maxillary sinuses. As teeth are lost in the posterior maxilla, bone is lost vertically. Implants must be placed in the remaining viable bone. As teeth are lost in the mandible, bone will recede apically and lingually. This may lead to an inability to position implants away from the mandibular nerve. Because of this, mandibular implants are often placed toward the anterior — in the symphysis and in front of the mental foramen (Fig. 6).
Angulation of implants also needs to be carefully considered. It is imperative that the implants used to retain an overdenture using individual Locator attachments be placed as parallel as possible in all three dimensions across the long axis of the bone (Figs. 7a, 7b). Failure to do so can result in decreased retention, problems seating the prosthesis, and increased wear on the Locator attachments.
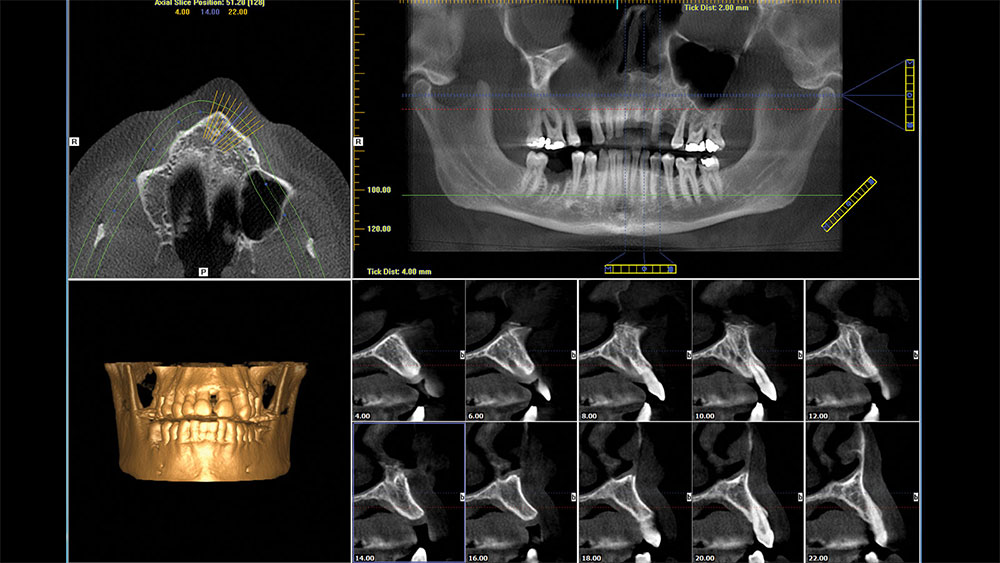
Figure 5: Example of CBCT scanning being used to assess anatomical structures and bone volume of a patient with nonrestorable dentition.
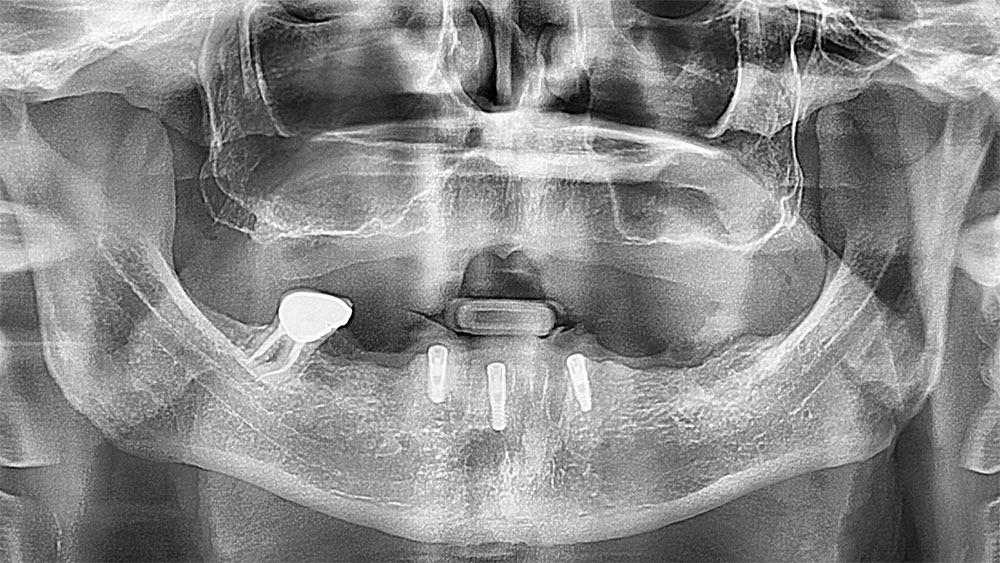
Figure 6: Example of implants placed in the symphysis area, anterior to the mental foramen, in order to retain a mandibular overdenture.

Figures 7a, 7b: Note how in this case the Locator attachments are nearly parallel along the axial plane, allowing for a passive fit of the prosthesis.

Figures 7a, 7b: Note how in this case the Locator attachments are nearly parallel along the axial plane, allowing for a passive fit of the prosthesis.
General Treatment Protocol
The basic treatment protocol utilized in the fabrication of Locator Implant Overdentures is straightforward. Many of the restorative steps incorporate conventional denture techniques and will thus be familiar to GPs accustomed to treating fully edentulous patients.
In the edentulous maxilla a minimum of four dental implants should be placed. When treatment planning mandibular restorations, the clinician has more flexibility and the option of placing two or more implants to support an overdenture (Figs. 8a–8c). This decision can hinge upon the amount of bone that is available and the finances of the patient. The mandibular symphysis area often provides favorable bone quality and quantity for implant placement. Although two implants with Locator attachments indeed provide increased retention of the overdenture, the more implants that are placed around the arch, the better the stability of the prosthesis.

Figures 8a–8c: Depending on the bone volume and wherewithal of the patient, practitioners have the flexibility of placing two implants or more in the edentulous mandible. All three of these cases are shown with Locator abutments in place, which engage with the retentive caps of the overdenture to stabilize the prosthesis.

Figures 8a–8c: Depending on the bone volume and wherewithal of the patient, practitioners have the flexibility of placing two implants or more in the edentulous mandible. All three of these cases are shown with Locator abutments in place, which engage with the retentive caps of the overdenture to stabilize the prosthesis.

Figures 8a–8c: Depending on the bone volume and wherewithal of the patient, practitioners have the flexibility of placing two implants or more in the edentulous mandible. All three of these cases are shown with Locator abutments in place, which engage with the retentive caps of the overdenture to stabilize the prosthesis.
The number of implants can also depend on the physical nature of the patient. A smaller person may only require two implants to establish prosthetic stability, while a larger person with heavier jaws and a stronger bite relation may require more. Note that, when allowed for by sufficient bone volume, spacing the implants around the edentulous jaw in an arch-form helps maximize anterior-posterior stability (Figs. 9a, 9b). When determining mesial-distal implant positioning for an overdenture, practitioners should be mindful that the distal cantilevers of the prosthesis should be approximately 1.5 times the A-P spread (Fig. 10). Essentially, the greater the A-P spread, the more stable the prosthesis. The All-on-4 configuration is commonly used to establish adequate spacing around the arch by tilting the posterior-most implants axially to avoid vital patient anatomy or accommodate limited bone while increasing the anterior-posterior spread.
Practitioners may want to consider placing enough implants to later upgrade the patient to a fixed prosthesis. This involves placing four or more implants and establishing an anterior-posterior spread greater than 10 mm. The cost of the screw-retained hybrid denture or monolithic zirconia implant restoration is significantly higher than that of an overdenture, but some patients may eventually want to transition to a nonremovable appliance.
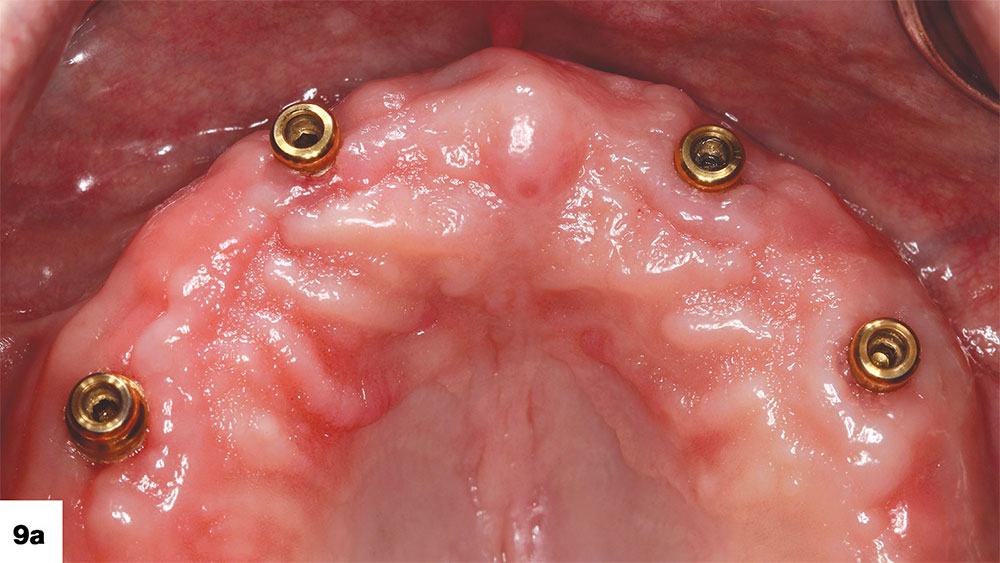
Figures 9a, 9b: Examples of implants placed around the span of the jaw to create an arch form, allowing for outstanding stability and function of the overdenture.
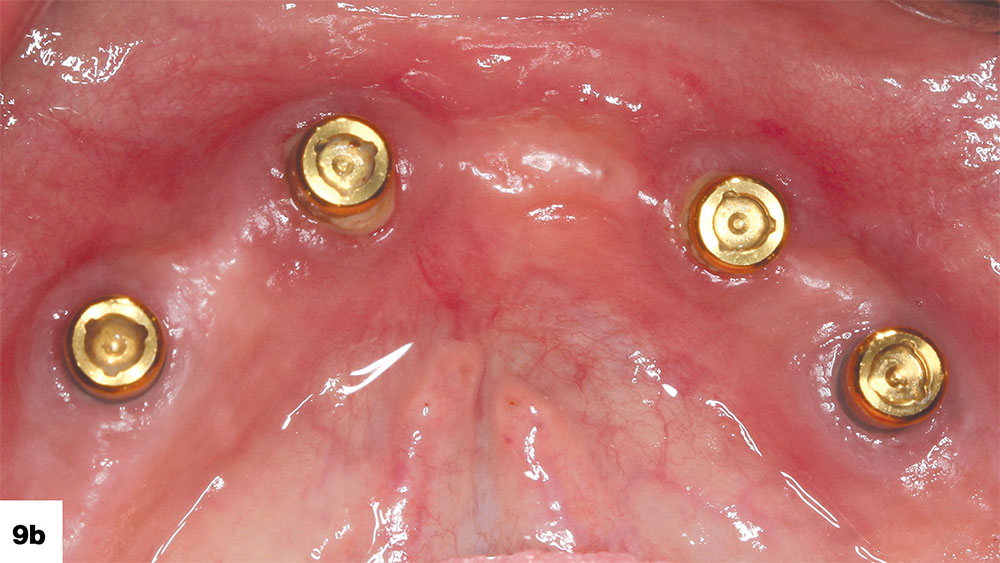
Figures 9a, 9b: Examples of implants placed around the span of the jaw to create an arch form, allowing for outstanding stability and function of the overdenture.
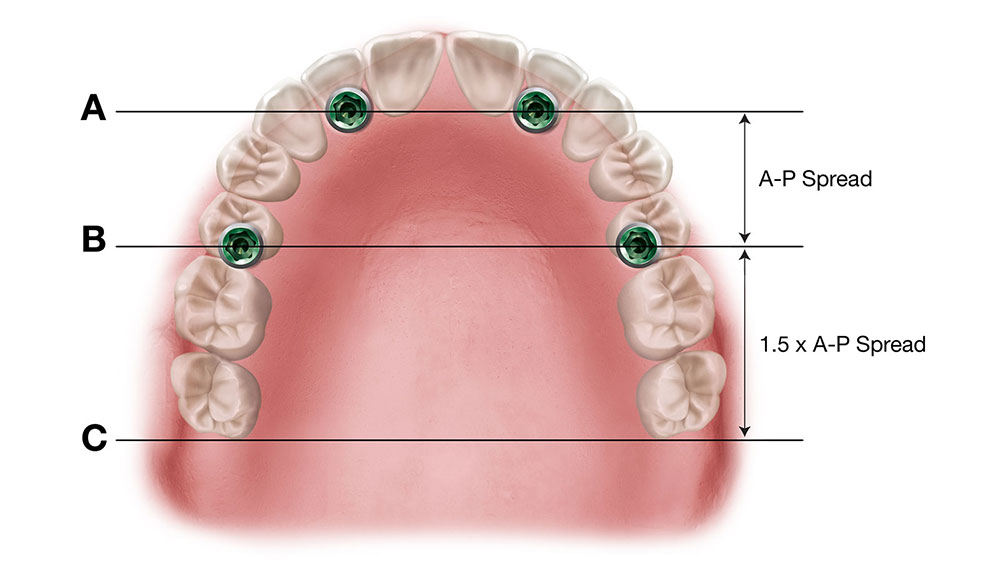
Figure 10: The approximate length of the overdenture’s distal cantilevers can be determined by measuring the A-P spread and multiplying that value by 1.5.
After placing the implants, the patient’s existing denture can be relined to seat over the healing abutments. For extraction cases, an immediate denture can be produced in advance and modified at the implant placement appointment. Provided sufficient initial implant stability, some clinicians favor an approach where the implants are loaded with a provisional appliance.
Once the implants have osseointegrated and the soft tissue has healed, the patient returns for the restorative phase. The chairside techniques to determine the prosthetic design are very accessible to practitioners accustomed to traditional dentures. The restorative process begins with an open- or closed-tray impression of the edentulous arch, from which the lab produces the master cast, wax rim and setup (Fig. 11).
The lab designs the wax rim and setup to seat over the Locator abutments, which are transferred from the cast to the patient’s mouth before the jaw relations are taken and the wax setup is tried in (Figs. 12a, 12b). This ensures an accurate fit of the eventual restoration and proper alignment of the Locator attachments with the retentive denture caps. At the next appointment, wax rims are used to record the jaw relationship (Fig. 13). As with traditional dentures, the lab then produces a wax setup, which is tried in to evaluate considerations like vertical dimension, centric relation, occlusion, phonetics, lip support, and tooth size, shape and position (Fig. 14).
After determining the definitive prosthetic design via the wax setup process, the lab produces the final implant overdenture for delivery. The appliance that the clinician receives includes processing inserts that will need to be swapped out for the appropriate attachment caps after trying in the prosthesis and making any necessary adjustments. These inserts come in a variety of retentive levels (Fig. 15). The appropriate level of retention depends on the strength of the patient. According to the manufacturer, the attachments resist wear and maintain satisfactory retention for up to 56,000 cycles of function.
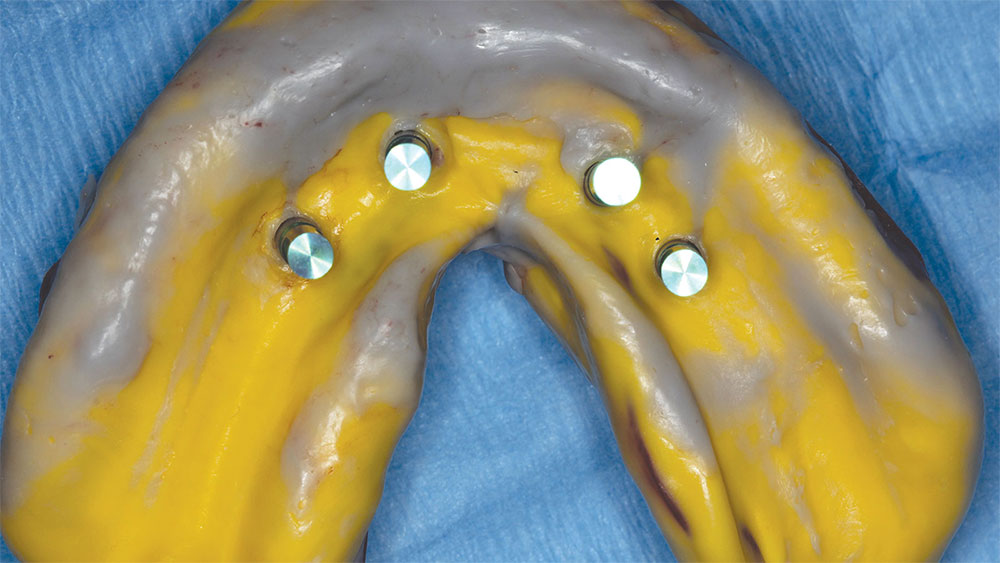
Figure 11: Example of a clean, accurate closed-tray impression produced using Panasil® vinyl polysiloxane impression material (Kettenbach; Huntington Beach, Calif.). From this a master cast is fabricated, beginning the restorative process.
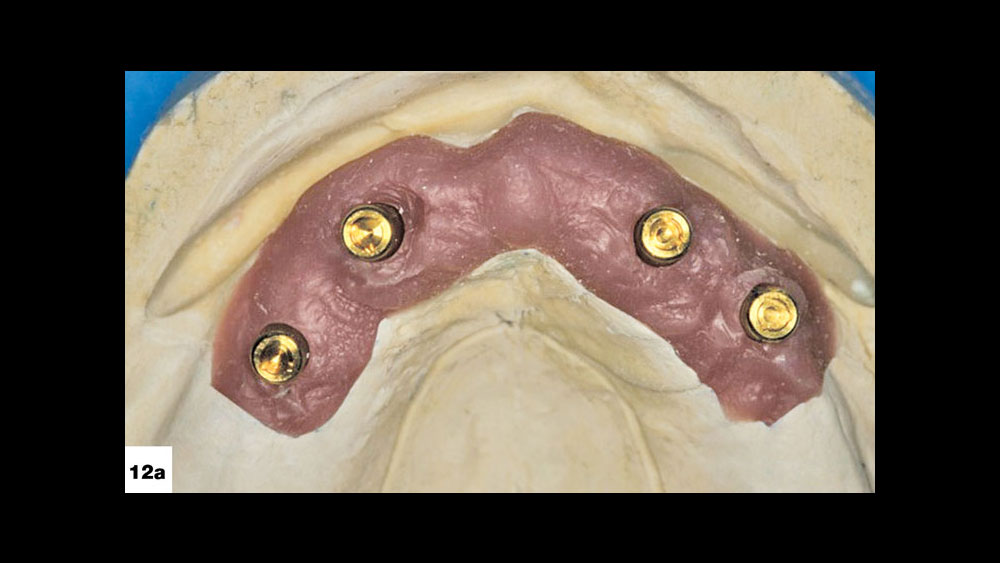
Figures 12a, 12b: The Locator abutments are transferred from the master cast to the patient’s mouth prior to seating the wax rim and setup.

Figures 12a, 12b: The Locator abutments are transferred from the master cast to the patient’s mouth prior to seating the wax rim and setup.

Figure 13: Conventional denture techniques are used to record the jaw relationship information needed to produce an implant overdenture.

Figure 14: Wax setup being evaluated for function and esthetics in preparation for a maxillary implant overdenture.
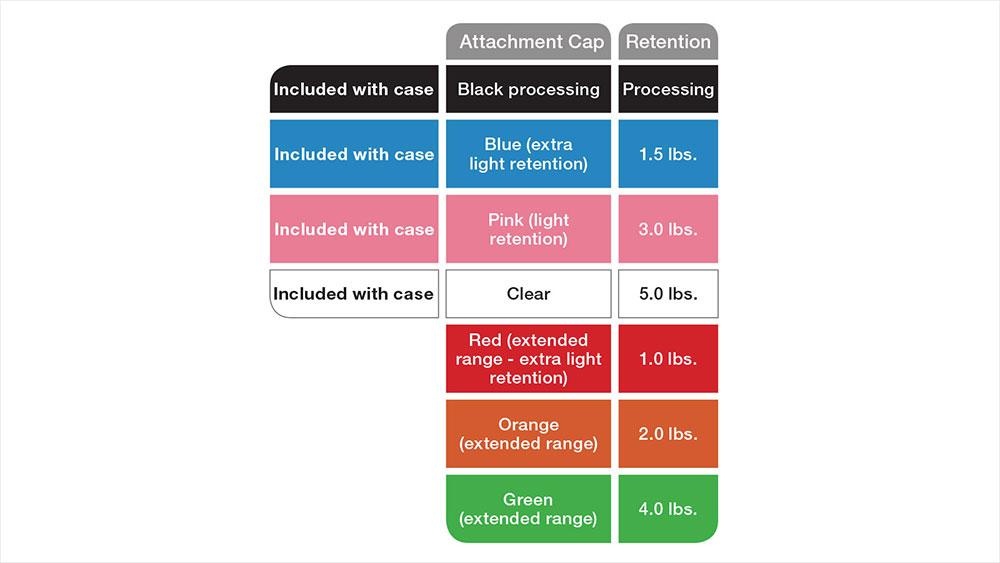
Figure 15: Locator Implant Overdentures are connected to the implants using retentive caps that are available in a variety of strengths and selected based on the number of implants and the bite force of the patient.

Figure 16: Final implant overdenture being tried in over Locator abutments.

Figure 17: The black processing caps are removed from the metal housings.

Figures 18a–18c: In this dual arch overdenture case, the black processing caps were replaced with pink retention caps. These implant-retained appliances provided the patient with an esthetic, highly stable restoration that greatly improved upon the function afforded by the traditional dentures with which he presented for treatment.
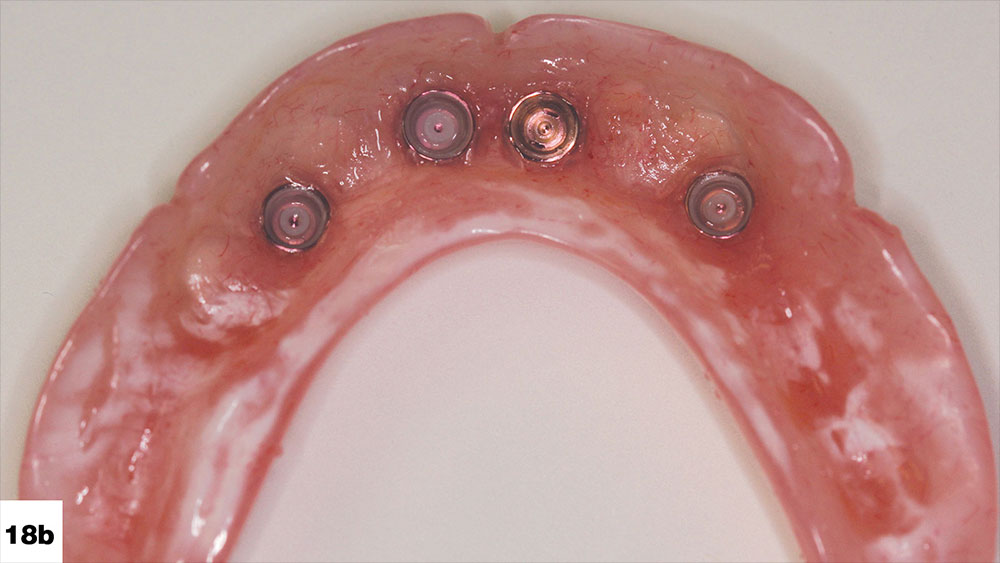
Figures 18a–18c: In this dual arch overdenture case, the black processing caps were replaced with pink retention caps. These implant-retained appliances provided the patient with an esthetic, highly stable restoration that greatly improved upon the function afforded by the traditional dentures with which he presented for treatment.

Figures 18a–18c: In this dual arch overdenture case, the black processing caps were replaced with pink retention caps. These implant-retained appliances provided the patient with an esthetic, highly stable restoration that greatly improved upon the function afforded by the traditional dentures with which he presented for treatment.
At the final delivery appointment, the implant overdenture is seated over the Locator attachments, and the fit, retention and occlusion of the appliance are confirmed (Fig. 16). The black processing inserts are then removed from the metal housings in which they are embedded in the overdenture (Fig. 17). The appropriate retentive caps are selected and seated into the metal housings, and engage the Locator attachments firmly upon final delivery of the appliance (Figs. 18a–18c). The end result is a dramatic improvement of the patient’s chewing function and efficiency, as well as quality of life. The attachments are easily maintained by the patient with brushing or a simple wipe with a washcloth.
Incorporating Implant Overdentures into the Dental Practice
Practitioners who are new to implant overdentures can either learn to place implants or refer the surgical procedure out to an experienced specialist. The only prerequisite is that the dentist must be proficient in designing and fabricating conventional dentures. For clinicians who have not yet learned to place implants or wish to maintain a strictly restorative practice, there are specialists, as well as many qualified general dentists, available to execute the surgical phase of treatment. However, it is imperative that the restorative doctor be the team leader. Dental implant therapy is now prosthetically driven. Visualizing the final case prior to surgery is critical to restorative success. Thus, the general dentist needs to determine and provide the implant surgeon with guidance on the design of the eventual prosthesis.
With proper training, dental implants can be placed to support an overdenture with great predictability by the general dentist. There are numerous programs available that can elevate the general dentist to a level of proficiency suitable for many implant overdenture cases. Programs that combine practical lecturing and hands-on training are ideal. Courses offered at the Engel Implant Institute (engelinstitute.com) and the Glidewell International Technology Center (glidewellcecenter.com) are excellent examples. At the Engel Implant Institute, programs are available in which attendees actually place an implant under a strict protocol and the direction of a mentor dentist.
As with any procedure, there is a learning curve that must be appreciated and understood, so starting out with procedures where the vital anatomy is not a concern and where bone quality and quantity is adequate is ideal. Becoming proficient in a procedure comes with time and experience, and there will always be cases that need to be referred out to the specialist for implant placement. However, placing implants in cases that are appropriate and within the comfort zone of the practitioner presents many advantages.
Conclusion
For clinicians looking to provide their edentulous patients with better function, stability and quality of life, the Locator Implant Overdenture is an excellent, cost-effective option. The restorative protocol is relatively easy to learn and presents an accessible gateway to implant therapy and the tremendous benefits it affords both the patient and the practice.
References
- ^ Haraldson T, Karlsson U, Carlsson GE. Bite force and oral function in complete denture wearers. J Oral Rehabil. 1979 Jan;6(1):41-8.
- ^ Kapur KK, Soman SD. Masticatory performance and efficiency in denture wearers. 1964. J Prosthet Dent. 2006 Jun;95(6):407-11.
- ^ Singh H, Sharma S, Singh S, Wazir N, Raina R. Problems faced by complete denture-wearing elderly people living in jammu district. J Clin Diagn Res. 2014 Dec;8(12):ZC25-7.
- ^ Papadaki E, Anastassiadou V. Elderly complete denture wearers: a social approach to tooth loss. Gerodontology. 2012 Jun;29(2):e721-7.
- ^ Rismanchian M, Bajoghli F, Mostajeran Z, Fazel A, Eshkevari Ps. Effect of implants on maximum bite force in edentulous patients. J Oral Implantol. 2009;35(4):196-200.
- ^ van der Bilt A, Burgers M, van Kampen FM, Cune MS. Mandibular implant-supported overdentures and oral function. Clin Oral Implants Res. 2010 Nov;21(11):1209-13.
- ^ Hyland R, Ellis J, Thomason M, El-Feky A, Moynihan P. A qualitative study on patient perspectives of how conventional and implant-supported dentures affect eating. J Dent. 2009 Sep;37(9):718-23.
- ^ Pan YH, Ramp LC, Liu PR. Patient responses to dental implant-retained mandibular overdenture therapy: a 6-year clinical study. Chang Gung Med J. 2007 Jul-Aug;30(4):363-9.
- ^ Zembic A, Wismeijer D. Patient-reported outcomes of maxillary implant-supported overdentures compared with conventional dentures. Clin Oral Implants Res. 2014 Apr;25(4):441-50.
- ^ Geckili O, Bilhan H, Mumcu E, Dayan C, Yabul A, Tuncer N. Comparison of patient satisfaction, quality of life, and bite force between elderly edentulous patients wearing mandibular two implant-supported overdentures and conventional complete dentures after 4 years. Spec Care Dentist. 2012 Jul-Aug;32(4):136-41.
- ^ Turkyilmaz I, Company AM, McGlumphy EA. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology. 2010 Mar;27(1):3-10.
- ^ Kordatzis K, Wright PS, Meijer HJ. Posterior mandibular residual ridge resorption in patients with conventional dentures and implant overdentures. Int J Oral Maxillofac Implants. 2003 May-Jun;18(3):447-52.
- ^ Institute for Dental Implant Awareness; Health Letter; 2000.
- ^ Grogono AL, Lancaster DM, Finger IM. Dental implants: a survey of patients’ attitudes. J Prosthet Dent. 1989 Nov;62(5):573-6.
- ^ Slot W, Raghoebar GM, Vissink A, Huddleston Slater JJ, Meijer HJ. A systematic review of implant-supported maxillary overdentures after a mean observation period of at least 1 year. J Clin Periodontol. 2010 Jan;37(1):98-110.