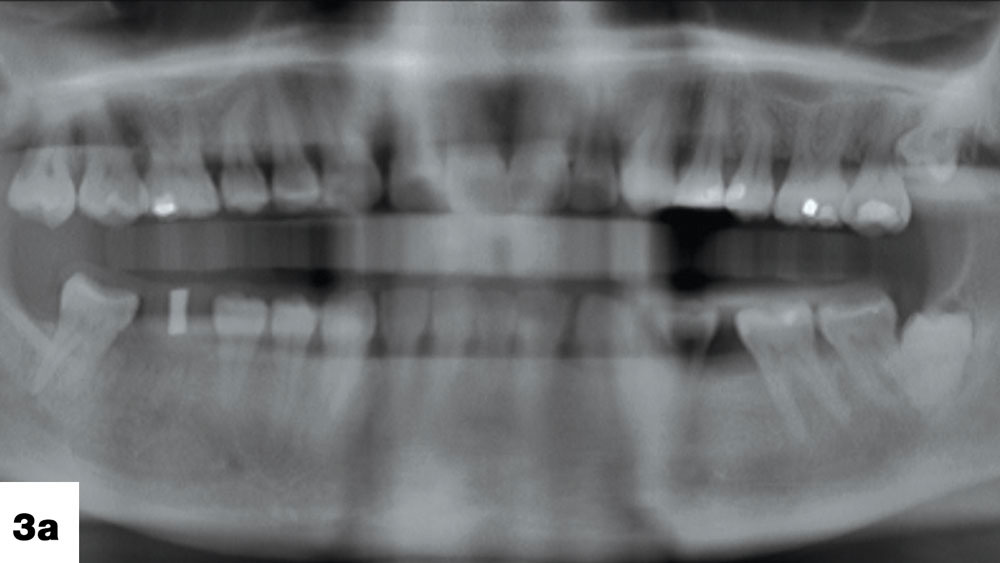
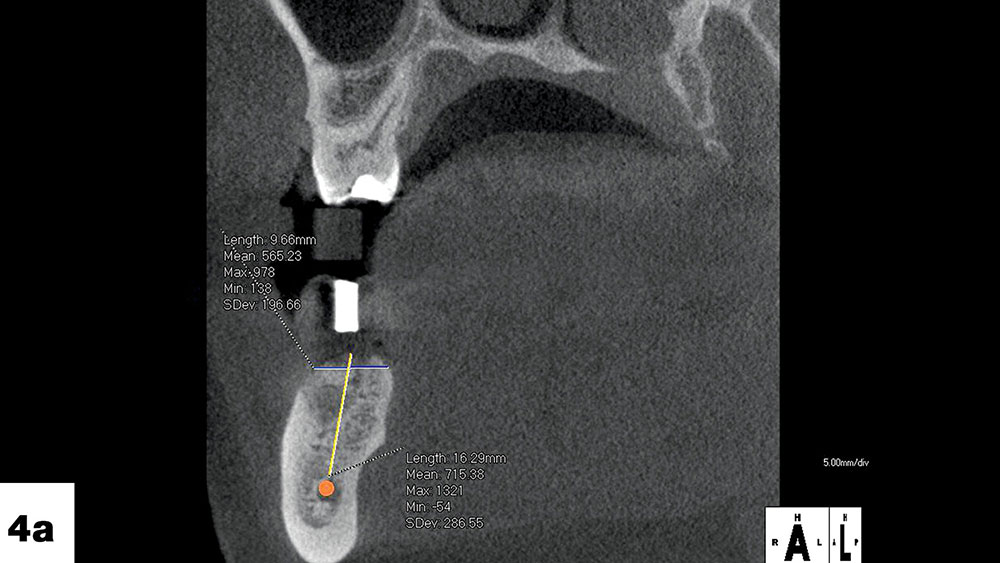
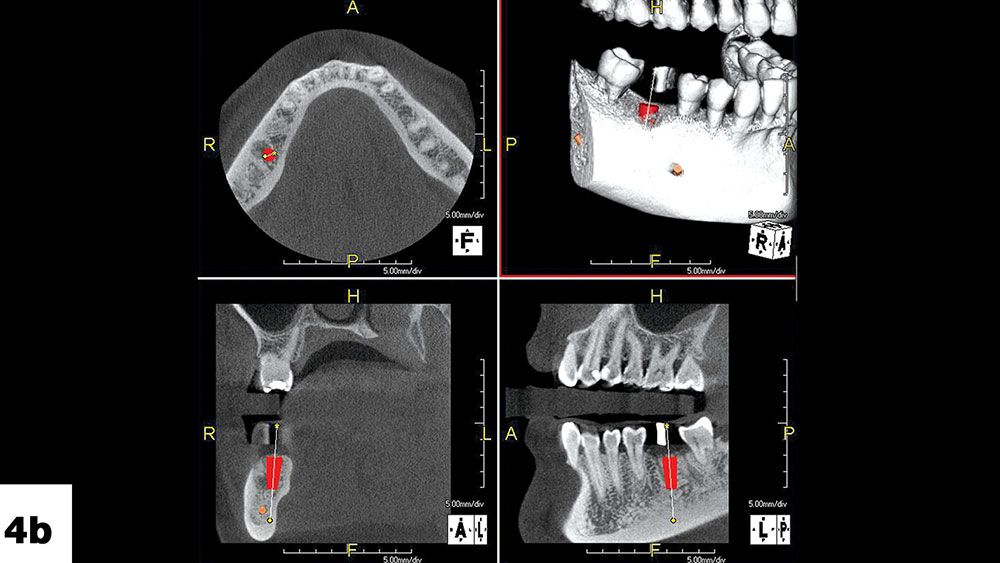
Photo Essay: Providing Implant Treatment and Protecting Dentition with an Astron Occlusal Splint

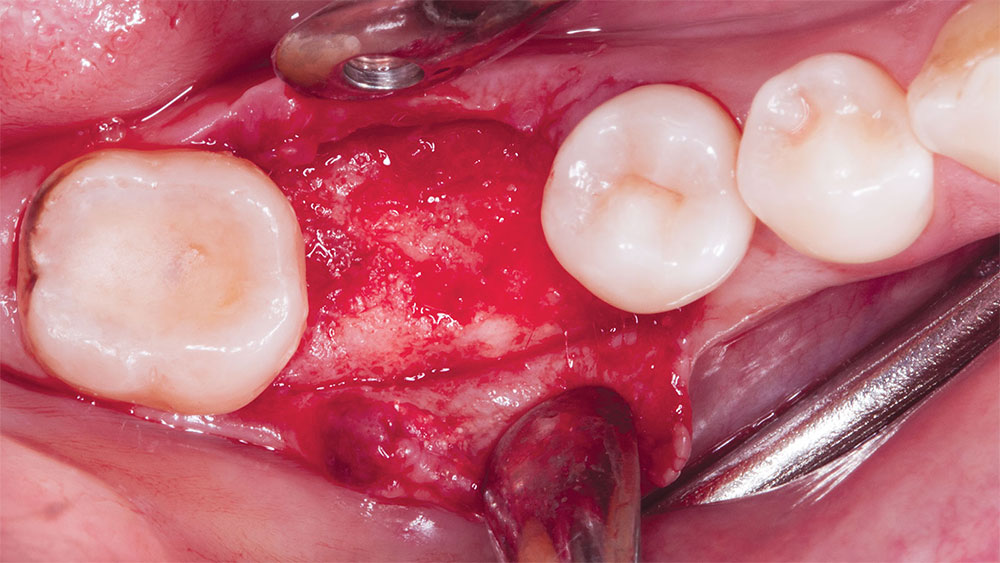
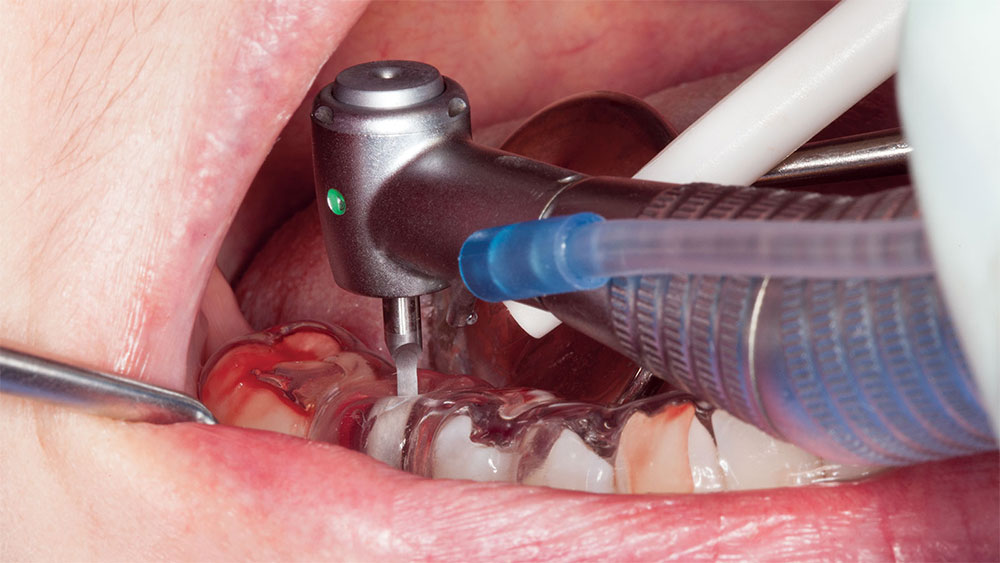
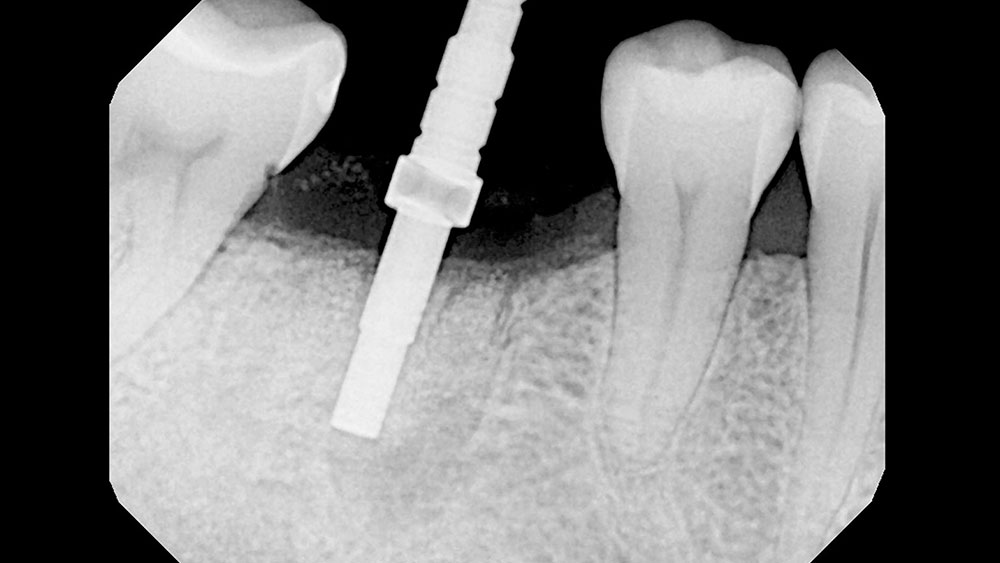
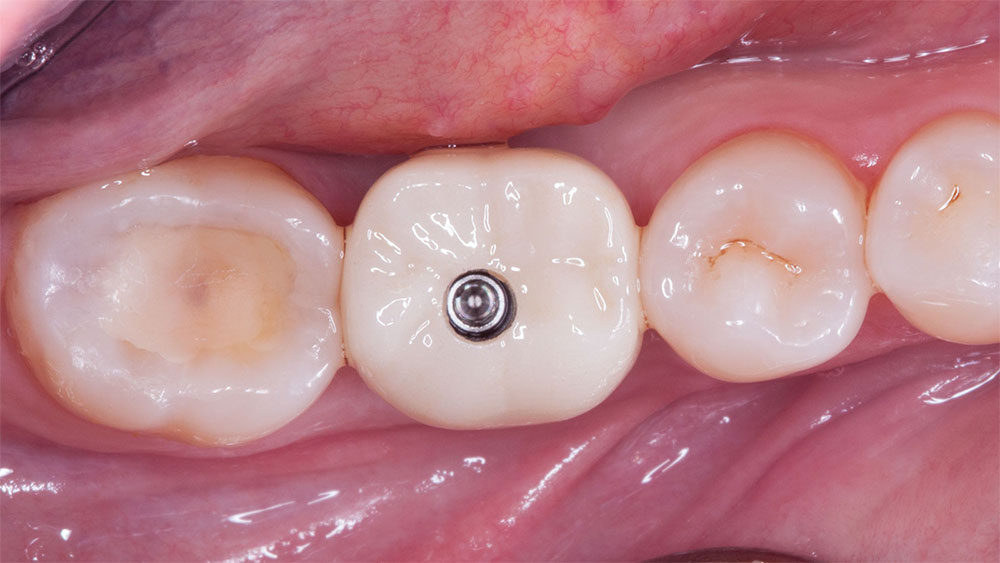
When faced with partial edentulism cases complicated by bruxism, clinicians’ treatment plans necessarily broaden beyond the mere placement of implants. Their armamentarium needs to acquire an ally that can defend the restoration against these excessive forces, and occlusal devices such as bite splints can fill the role. This photo essay, which is Part 2 for detailing this case, shows how implant treatment fit the patient’s need to restore function and esthetics; during and after treatment, an Astron bite splint continued to be the occlusal device of choice. (Find Part 1 here.)
References
- Rosen P, Clem D, Cochran D, et al. Peri-implant mucositis and peri-implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol. 2013 Apr;84(4):436-43.