The Mylohyoid Ridges: Troublemakers Often Undiagnosed

We dentists have been taught the importance and the benefits of having denture bases for removable prostheses that are fully extended to the functional muscular periphery. This principle is especially important with mandibular denture bases, whether they are for full dentures, overdentures or distal-extension removable partial dentures.
Many dentists have mastered the art of obtaining fully extended “muscle trimmed” impressions utilizing custom impression trays, border molding and “wash” materials. Some clinicians even make a temporary denture of limited accuracy, border-mold it, and do a wash impression, all with the use of tissue conditioner mixed to various states of viscosity. The patient then wears this out of the office, instructed on precautions, before returning in a few days for peripheral additions and possibly another wash impression.
In this manner, extremely accurate functional peripheral borders and surface reproduction can be obtained within a few days to weeks. The clinician then pours the impression/temporary denture combination in stone, submerging it under cold water after the initial set of the stone in order to dissipate the heat of the chemical reaction upon final setting, which could distort the tissue conditioner. Upon separation of the stone cast, the temporary denture is returned to the patient with its tissue conditioner intact, and the clinician has a beautifully accurate stone cast to proceed to the next step of making a final denture for this patient.
THE PROBLEM
As is often the case, after a day or so of wearing this fully extended mandibular denture, with its deeply extended lingual flanges that so effectively prevent lateral displacement of the denture during function, the patient complains of extreme pain and ulceration in the region of the lingual vestibules. After several spot-relieving appointments, none of which seem to help remedy these painful areas, many clinicians acquiesce to a patient’s demands and trim away up to 50% of those wonderful stabilizing lingual flanges that took so much skill and perseverance to make. So what happened? The patient blames the denture for “cutting into my jaw.” However, exactly the opposite is true. The very sharp mylohyoid ridge cut through the oral mucosa from the lingual, pressing against the tissue side of the lingual denture flange, which acted like a “cutting board.” The soft tissue was the “bread”; the mylohyoid ridge was the “knife”; and the lingual flange was the “bread board.” The denture base was not the culprit, but now the stability of this denture has been greatly compromised by its removal, which can be a serious problem to clasped teeth, implants, attachments and retention screws.
The denture base was not the culprit, but now the stability of this denture has been greatly compromised by its removal.
Basically, the lingual flanges are the only stabilizing feature against lateral displacement or “fishtailing” of the denture base during function. The lingual surfaces of the mandible are vertical, while the facial surfaces are sloped. It’s just simple mechanics. This constant lateral movement can loosen, fatigue, or break the retaining screws that hold implant-supported attachments or bar-clip retainers in place. Moreover, it can cause the loss of integration of anterior implants and even cause implant fracture in some cases. It can also prematurely wear out O-ring denture retainers and other denture retention systems. It’s just like having a long cantilever arm connected to the anterior implants.
THE SOLUTION
The solution to this frustrating problem is to follow a strict denture examination protocol with every patient who requires either a reline of an existing full or partial lower denture, or an entirely new denture. Remember, the cause of the pain is not the denture, but the sharp mylohyoid ridge, and that ridge belongs to the patient. The patient’s mylohyoid ridge remodeled over the years and became knife-sharp as a result of bone resorption around it (Fig. 1). It is as though a rainstorm and flood had washed all of the smaller gravel particles from a dirt road, leaving only the larger, jagged rocks exposed. This is the patient’s problem, and you, the clinician, can solve it and still have fully extended lingual flanges. But first you must recognize the problem, and demonstrate and explain it to the patient before starting any denture treatment.
The cause of the pain is not the denture, but the sharp mylohyoid ridge, and that ridge belongs to the patient.
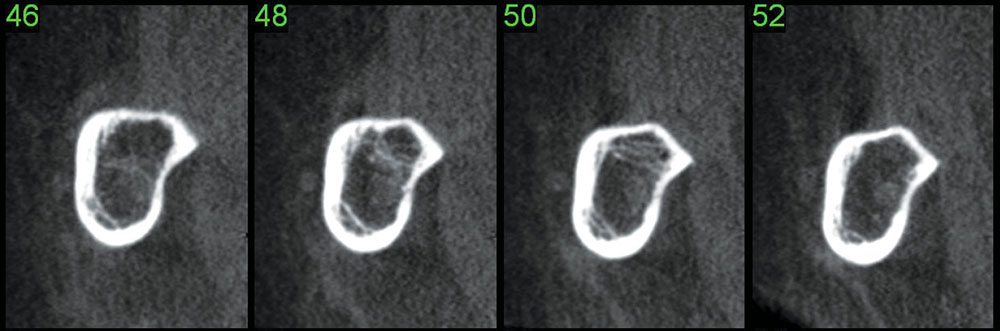
Figure 1: Cone-beam computed tomography can be utilized to visualize the sharp mylohyoid ridge of a patient. The cross-sectional slices individually reveal the clinical situation and can be beneficial in dentist-to-patient communication prior to treatment.
PROTOCOL STEPS
1. Ask the patient to hold his or her breath (to keep from gagging), and then place your index finger deeply into the patient’s lingual vestibule and palpate the mylohyoid ridge. If the ridge is sharp (it usually is), the patient will “flinch” and experience acute pain.
2. Now take the patient’s index finger, guide it into his lingual vestibule, and repeat what you just did yourself. The patient will cause himself acute pain, but will now be convinced that the cause is from his own sharp area on his jawbone.
3. Tell the patient why his bone is so sharp (bone resorption and “gravel road” analogy), and explain why this will produce pain from any properly fitting denture base that you would make for him.
4. Suggest to the patient that you want those sharp bony ridges removed or smoothed away before you start the new denture, overdenture, RPD or reline. Explain that not doing so will surely result in a poorly fitting and unstable denture. If you have surgical skills you can do this procedure yourself, one side at a time, with a one-month interval so as not to cause bilateral pharyngeal edema that could restrict swallowing and frighten a patient. Otherwise, send the case to an oral-maxillofacial surgeon.
Performing this procedure requires good local mandibular and long buccal nerve block anesthesia. A 2–3 cm straight-line incision is made along the posterior ridge crest from the retromolar pad anteriorly to the #20 tooth position. A periosteal elevator is used to reflect a full thickness flap separating the soft tissue from the lingual surface of the mandible. Keep the elevator firmly against the bony surface at all times. This lingual soft tissue separates easily from the bone. Locate the mylohyoid ridge, and with a sharp bone file patiently remove the sharp surface. Gently irrigate and suction the area to remove bone debris. Never blow air from a syringe into the area, as this could cause a submandibular emphysema. Palpate the area to determine whether the bone removal is sufficient before suturing the flap. Psychologically prepare the patient for some unilateral pharyngeal edema and moderate osteitis pain for approximately 5–10 days.
Dr. Garfield is the executive director, advisor-trustee and past president of the Southern California Academy of General Dentistry (SCAGD). Contact him via email at drrobertgarfield@aol.com.