Photo Essay: Implants, Edentulism and the New General Practitioner

The positive long-term prognosis for implant dentistry has provided dentists with an optimum treatment option for patients with missing teeth. For decades, the standard of care for a patient presenting with an edentulous space in the area of tooth #3 and #4 would be: a 4-unit fixed dental prosthesis spanning teeth #2–5, or a removable partial denture. This has sufficed to provide patients with the necessary posterior chewing surfaces, but has done little to address other systemic issues that accompany partial edentulism, such as mesial drift of an existing distal tooth, supereruption of opposing dentition, or the atrophy of the residual ridge with bone and soft-tissue loss. Additionally, the fixed dental prosthesis solution required the preparation of adjacent teeth for use as abutments, placing excess stress on the natural teeth and, in concert with bone resorption and possible recurrent decay, compromising the restoration to a 10–15-year shelf life.
With the advent and popularity of root-form dental implants, clinicians now have a better alternative, albeit one that thus far has often been relegated to the purview of specialists. Like many dental disciplines, however, the properly trained general practitioner is potentially well-suited to handle most of these straightforward cases, with the more complicated iterations requiring experienced intervention. In this photo essay, the patient presented with a posterior edentulous space, along with PFM restorations abutting mesial and distal to this space. By restoring the area with two implants rather than a 4-unit fixed dental prosthesis, the patient was restored with four single-unit monolithic crowns, serving to improve the prognosis and address all of the chief functional and restorative concerns.
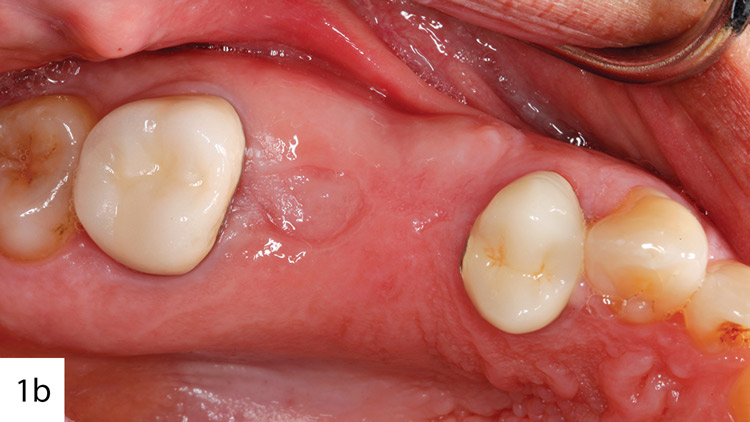
Figures 1a, 1b: The patient presented with an edentulous space in the area of tooth #3 and #4, as well as PFMs on #2 and #5. An oral examination, radiographic imaging and evaluation of a cone-beam CT scan determined the bone was adequate for implant placement, with no initial grafting procedure necessary. To improve esthetics and the long-term viability of the adjacent restorations, the PFMs would be replaced with monolithic BruxZir® Solid Zirconia crowns on the natural teeth to match the BruxZir Solid Zirconia screw-retained implant crowns on the implants.
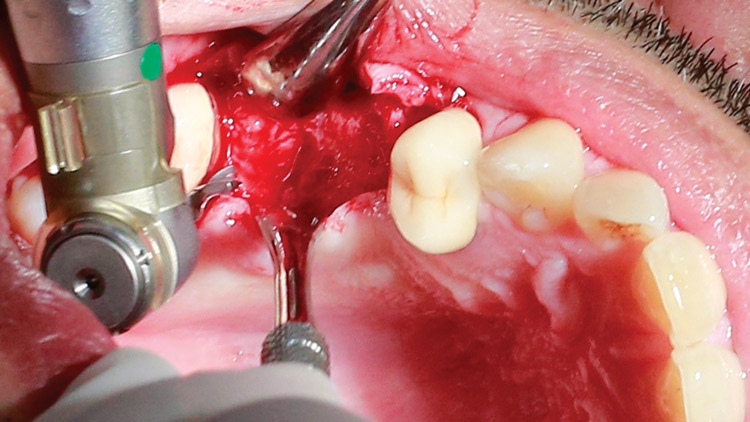
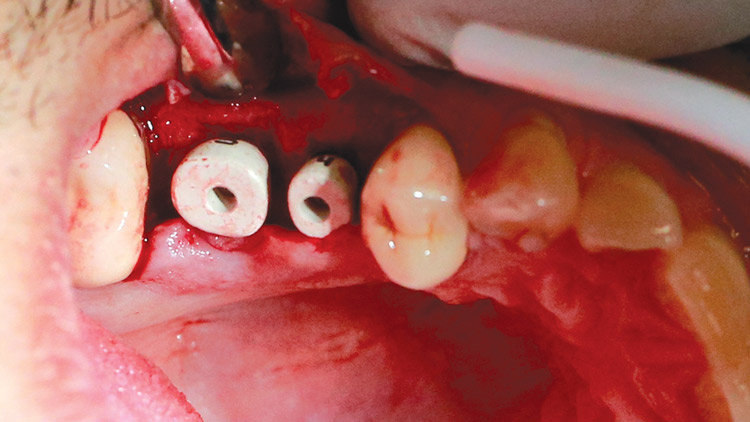
Figure 2: A flap is reflected prior to creating the osteotomy. Although the use of a tissue punch in a flapless procedure is less traumatic to the soft tissue, reflection of a full-thickness flap is necessary to visualize the bone anatomy firsthand, which can present vital intraoperative details. Once the bone is exposed and the initial osteotomies are created to the appropriate depth and angulation, a series of graduated drills is used to complete the osteotomies to the diameter precisely coordinated for the prescribed implants.
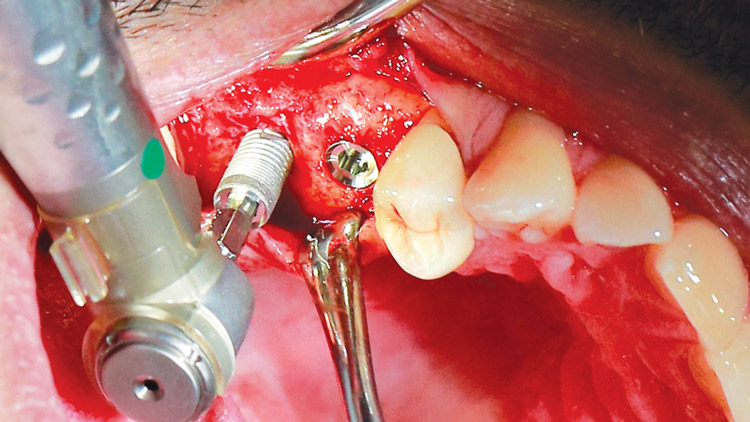
Figure 3: Each implant is threaded to bone level with the implant handpiece and driver and often hand-torqued into final position utilizing a torque wrench. Direct visualization ensures the appropriate seating of the implant into the osteotomy and at the bone level. Primary stability can be tested at this stage if immediate loading is desired; however, for this case, custom tissue-contouring healing abutments were prescribed with loading set to occur only after completion of the full-term healing phase and osseointegration.
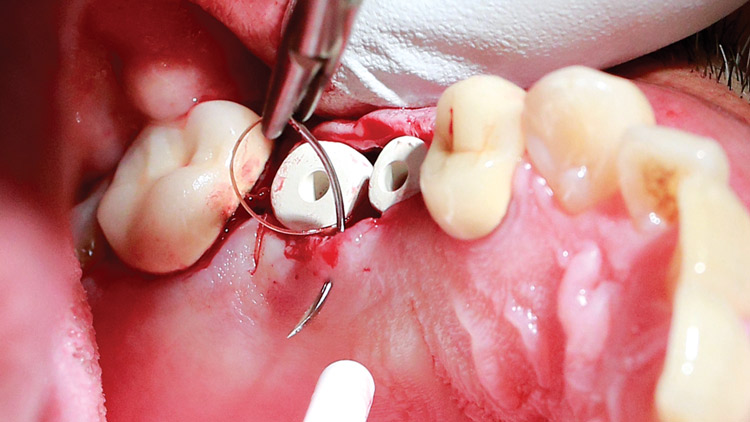
Figure 4: Although stock healing abutments would be sufficient in this case, custom healing abutments were chosen to help ensure a proper emergence profile from the shoulder of the implant through the mucosa. In this case, tissue-contouring healing abutments led to a more natural-looking emergence profile, created support for a wide, stable crown base, and reduced the likelihood of unhygienic contours.
Figure 5: The buccal and lingual tissue was approximated with three interrupted sutures. The close approximation of the soft tissue allowed for a near primary closure, which helped ensure proper healing circumferentially around the custom healing abutments.
Figures 6a, 6b: The patient returned one week post-implant-placement for a follow-up appointment and possible suture removal. Due to the amount of bone present buccolingually, no vertical releasing incisions were created and the patient’s healing time was kept to a minimum.
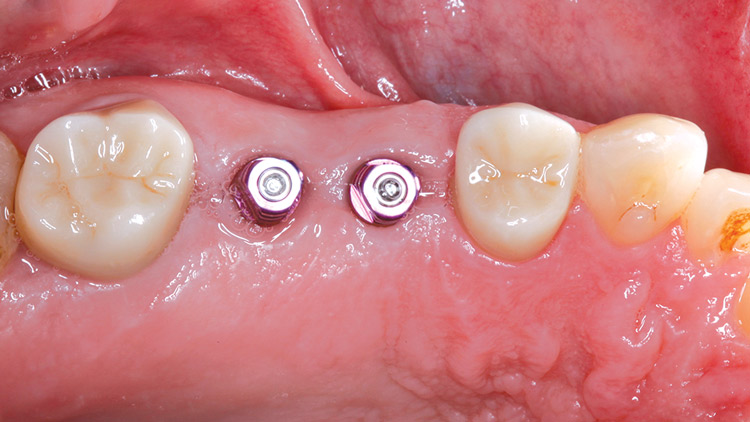
Figures 7a, 7b: At the two-week postoperative appointment, the tissue exhibits desirable adaptation to the healing abutments with no sign of inflammation or suppuration. Note the soft tissue healing interproximally at the follow-up visit. This initial post-op appointment is just to confirm that the patient is healing with no postoperative complications, and to prevent potential concerns before they exacerbate. If all looks well, the implants will be allowed 4–6 months to fully osseointegrate and achieve ideal stability prior to the restorative phase.
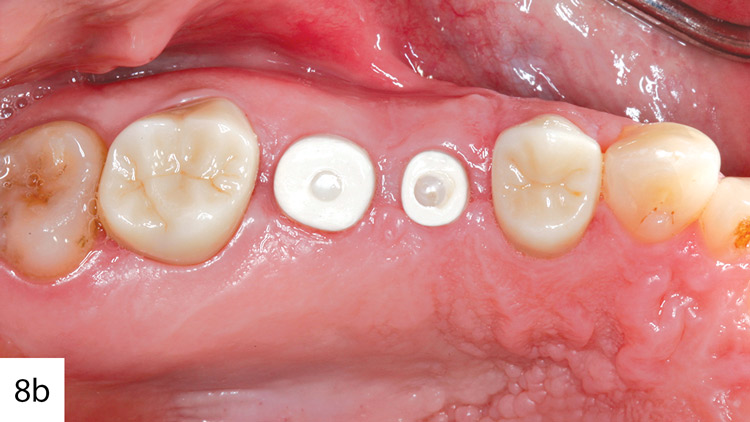
Figures 8a, 8b: Four months after the implant placement procedure, the tissue has conformed well to the shape of the custom healing abutments. For the sake of efficiency, as the implants were going through the osseointegration phase, the adjacent PFMs were replaced with full-contour BruxZir crowns. The BruxZir crowns were contoured with the goal of restoring the implants with single-unit restorations in mind. It is important to communicate the final goal to the laboratory in order to create proper contours and mesial-distal width of crowns on the natural teeth.
Figure 9: For the restorative procedure, the patient returned for the final impression, where the healing abutments were removed and closed-tray impression copings were placed and confirmed to be seated properly with radiographs. A full-arch impression was made utilizing medium- and heavy-body vinyl polysiloxane impression material. By adhering to proper protocol and using materials with adequate rigidity, studies have shown the accuracy of the less labor-intensive closed-tray impression to be statistically equal to that of an open-tray impression.1,2
Figures 10a, 10b: Once the final impression was made, the impression copings were connected to implant analogs and placed back into the impression. It goes without saying that the more accurate the information you can provide to the laboratory, the better the final results will be. A full-arch impression tray must be used on both the working and the opposing arch in order to give the laboratory sufficient data to determine appropriate occlusal clearance and prevent excursive interferences, which is vital to avoiding overload of the implants.
Figures 11a, 11b: Buccal and occlusal view of the final BruxZir implant restorations in place alongside the BruxZir crowns on #2 and #5. The long-term prognosis for these crowns is highly favorable because they allow the patient to clean each tooth individually with dental floss and normal brushing habits. The emergence profile on the implant restorations was improved with the utilization of the custom healing abutments.
Figure 12: Radiographic imaging confirms the ideal position and osseointegration of the implants with no crestal bone loss, as well as the full seating of the BruxZir crowns. The CAD/CAM design of the restorations allows for consistency throughout the manufacturing process, creating final restorations with a highly accurate fit.
By adhering to proper protocol and using materials with adequate rigidity, studies have shown the accuracy of the less labor-intensive closed-tray impression to be statistically equal to that of an open-tray impression.
Conclusion
The restorative phase of implant dentistry has become routine in a general practitioner’s office. With the proper training, implant placement can also be more commonplace in the general practice. As with any field within dentistry, acquiring the skills to both place and restore implants takes dedication, time and patience. Organizations such as the American Academy of Implant Dentistry and the Academy of Osseointegration help to promote such learning, and often provide hands-on training to aid with continuing education for general dentists and specialists. For clinicians interested in dedicating a portion of their practice to implant dentistry, that achievable goal can come to fruition because of the commitment we have invested in our field that have made these opportunities available.
References
- ^Pera F, Pesce P, Bevilacqua M, Setti P, Menini M. Analysis of different impression techniques and materials on multiple implants through 3-dimensional laser scanner. Implant Dent. 2016 Apr;25(2):232-7.
- ^Rashidan N, Alikhasi M, Samadizadeh S, Beyabanaki E, Kharazifard MJ. Accuracy of implant impressions with different impression coping types and shapes. Clin Implant Dent Relat Res. 2012 Apr;14(2):218-25.