One-on-One Interview with Chad Duplantis, DDS
Dr. Chad Duplantis maintains a private practice in Fort Worth, Texas, and serves as a consultant for 3M™ Oral Care. In addition, he lectures nationwide about various aspects of digital and CAD/CAM dentistry, with a particular focus on how practitioners can successfully incorporate digital dentistry into their private practices. Here, Dr. Duplantis discusses his entrance into the world of digital dentistry, the “50/50” concept, and how his partner and staff have adjusted to the adoption of new dental technology.
DR. NEIL PARK: Let’s talk a bit about your background. Are you originally from Fort Worth?
DR. CHAD DUPLANTIS: Originally, I’m from New Orleans, Louisiana, but I’ve lived in Texas for the majority of my life. I went to dental school at the University of Texas Health Science Center at San Antonio, and then I did a one-year AEGD residency at Baylor College of Dentistry in Dallas. My wife and I have been in Dallas–Fort Worth for the past 20 years.
NP: Now, back when you did your schooling and your residency, was there any education in the field of digital dentistry?
CD: None whatsoever. It’s funny that you ask — I was walking through the airport recently, and I ran into my operative dentistry professor and the dean of the dental school I went to. He asked me, “Where are you headed?” I said, “I’m off to New Jersey to speak about CAD/CAM dentistry.” And he said, “Oh my gosh, you should see the dental school today. We’ve got so many CAD/CAM devices and scanners and mills.” It was really nice to hear that they’re incorporating the technology now, but we had no idea what it was when I was in dental school.
NP: Things are changing. So how did you become interested in digital dentistry?
CD: In 2004, I bought an older piece of equipment that is still widely used today. This was right after I got out of dental school, and I was trying to find a way to eliminate my lab bill — and it worked “to an extent.” However, I probably tested the limits of the system and used it to do things that it wasn’t intended to do.
NP: Was this a system that was scanner-and-mill?
CD: It was scanner-and-mill — same-day dentistry, all packaged together. I had a humungous payment on the machine, and I felt that I was kind of captive to the device and had to fabricate restorations because I had this payment to make. Granted, it was a great piece of equipment, but I probably used it beyond its capabilities. So, when it did not produce the quality of dentistry that I wanted, I decided to give up the equipment and the technology. I ended up losing a lot of money as a result of my decision to purchase the machine. I think I had false perceptions of the purpose the system was going to serve in my office.
Then, in 2007, I ventured out again and bought a digital impressioning device. This device worked, but I ended up sending it back. It was very, very hard to learn, and even though the products that I received back from the laboratory were great, I still wanted to be able to mill some restorations while sending others off to the lab. I had my growing pains with that piece of technology, but I still yearned to participate in CAD/CAM dentistry and incorporate it into my office.
In 2012, I was approached by 3M to beta-test their new True Definition Scanner. I was a little reluctant at first, but 3M told me that the system would communicate with a mill. Even though I enjoyed milling restorations, I don’t do that exclusively. So I decided to give the system a try, and I haven’t stopped since. It’s been the best addition I’ve made to my office since I began practicing in 2000. It offers the perfect mix for me: I can send some stuff off to the lab while milling other cases in the office.
NP: Right. I recently had the opportunity to hear you speak at a symposium on digital dentistry at the Glidewell International Technology Center, and that’s a point you made very well several times in your lecture: It’s great to have the opportunity to mill in the office, but it’s not what you do exclusively. You talked a little bit about the “50/50” concept.
CD: Right. The 50/50 concept is what works well in my office. A lot of dentists want to mill exclusively, while others want to scan impressions exclusively. I like a mix of the two. I’ve never really intended to be a lab tech — I’ve always just aimed to provide quality dentistry — but I like the hands-on work of designing the restorations. Believe it or not, I liked waxing restorations in dental school. I still get to do that and have a little bit of fun, but if I think the patient is going to be better served by me sending their case off to the laboratory, I’m able to do that as well. So I like the flexibility that I have.
NP: So with this 50/50 concept — where you mill some cases in your office and send others to commercial labs — how do you decide which cases are right for in-office milling and which should be sent out?

CD: First of all, I think the greatest benefit of the in-office mill is the ability to offer same-day dentistry. If you can provide a patient with that service, the patient is going to be forever grateful that you were able to help them in one visit. I certainly take that into consideration, and I love to be able to provide that service to my patients. However, it’s not going to be for every patient, and you have to realize that, as much as you want to give the patient same-day service, you ultimately have to do what’s best for the patient. And offering that service is not always best for the patient.
Regarding how I decide which cases to mill in office and which to send out, for cases that I send to the laboratory, those involve a tooth that requires a little bit more characterization than I’m willing to provide in the office. For anterior cases, I send the majority of them to the laboratory, because I trust the technicians at the laboratory to stain and glaze those restorations and to characterize them to my patients’ specific needs better than I could. If I were to do it in the office, although I trust the materials I work with, it would take a lot longer, and if I’m working on several units of anterior teeth, the same-day dentistry approach wouldn’t be practical.
As far as a posterior tooth is concerned, if it’s a tooth in the esthetic zone that the patient is going to be able to see, and I don’t want to put the extra effort into staining and glazing, I’ll send that case to the laboratory. If I don’t have enough time in the day or the patient isn’t pressing for a same-day restoration, I’ll send those restorations off to the laboratory as well. So there are several factors that go into it. Same-day dentistry would be great for every patient, but you’ve got to know your limitations along with the patient’s limitations and expectations.
NP: You mentioned that you were an early adopter of intraoral scanning, and in fact you had a couple of false starts. So, as we talk about what a doctor can do to successfully incorporate intraoral scanning into his or her practice, how will a doctor know when his or her practice is ready to incorporate this technology?
CD: Well, first of all, ignore my false starts, because that was all on me. However, I think intraoral scanning has advanced to the point where most doctors are ready to incorporate the technology into their office. I think the workflow has been proven, and the restoration quality you receive from digital scans is superior to that of traditional impressions. On top of that, it reduces procedure time. Once you see all of these benefits, and you actually start using the technology in your office, it’s a very easy transition. More doctors just need to be receptive to the benefits of intraoral scanning. Many doctors are fearful of the way the technology used to be, with its cost and difficulty, along with the requirement of providing same-day dentistry when a lot of doctors don’t actually want to do that. The flexibility of today’s systems, though, allows practitioners to do whatever they want.
Many doctors are fearful of the way the technology used to be, with its cost and difficulty, along with the requirement of providing same-day dentistry when a lot of doctors don’t actually want to do that. The flexibility of today’s systems, though, allows practitioners to do whatever they want.
NP: Great. And how will a practitioner know when he or she is ready to take the next step and incorporate in-office milling successfully?
CD: There’s a greater number of doctors who aren’t ready to incorporate in-office milling than those who aren’t ready to incorporate scanning. I think that a doctor can provide quality restorations with in-office milling; the workflow and materials are proven, and doctors would be able to reduce their bills with the technology. However, in order to be ready to adopt in-office milling, doctors need to enjoy working with their hands, playing with technology, and providing same-day service to patients. Scanning can serve as a gateway to in-office milling, though, and if more doctors start scanning, then I think that the receptiveness to milling would be a lot greater.
To be ready to adopt in-office milling, doctors need to enjoy working with their hands, playing with technology, and providing same-day service.
NP: A lot of doctors have told me that one of the reasons they like in-office milling is because of the degree of control it provides them. They can personally set what their contacts are, and what the occlusion and buccal contours will be. Has that been a benefit for you?
CD: It’s a huge benefit. You have complete control of the restoration that goes into the patient’s mouth.
NP: You mentioned you’ve had experience with several different in-office milling devices, and now you’re using the TS150™ mill (Prismatik Dentalcraft, Inc.; Irvine, Calif.). Can you tell me what got you interested in that mill and what your experience has been working with it?

CD: First of all, the TS150 is backed by Glidewell Laboratories, which is such a large and dynamic lab. They put a lot of research into everything they do, and they provide a great product. The second thing that got me interested was the price point. With the TS150 mill, you can get into milling without having to take out a second mortgage on your house. It’s a very affordable investment. And for my practice, what really intrigued me was that the TS150 offers a manageable number of milling material options. You don’t have this overwhelming feeling of having to decide what material you’re going to use; you only have a few options. In my practice, that works best. I don’t want a cafeteria menu full of options. I want to have a few things that are proven, that work, that have great strength and esthetics, and that will result in a quality restoration in my patient’s mouth.
On top of that, the majority of us are placing full zirconia restorations in patients’ mouths on posterior teeth, and with the TS150, you’ve got a mill that’s more affordable than competing zirconia mills. That’s huge. So I think that, on top of all of the other things that I mentioned, zirconia is the largest drawing factor for a lot of dentists who are considering the TS150.
NP: Let’s talk a little bit about the materials, because I understand the number of different materials that you can mill with the TS150 has been increasing. What are the main materials that you’re using?
CD: The majority of what I mill is Obsidian® (Glidewell Laboratories; Newport Beach, Calif.), a lithium silicate material. It’s a wonderful material, it’s got great strength and esthetics, it mills beautifully, it comes out of the mill beautifully, and patients seem to love it. I’m also using BruxZir® NOW, which you can mill in your office. It has incredible strength — it offers slightly less strength than what you can get from the laboratory, but it’s way more than you’d ever need in a typical setting. It’s a full zirconia material, and it’s pre-sintered. It’s a beautiful product.
NP: Does “pre-sintered” mean that you do not have to put it in an oven after it’s milled?
CD: That’s right. It mills and it polishes, and then it’s ready to go in the patient’s mouth. There’s no shrinkage that you have to be concerned about, and there’s no additional firing when you pull it out of the mill. It’s a wonderful restoration to be able to offer to a patient, especially in a same-day setting.
NP: And, for example, on a posterior tooth, how do you decide whether to use, say, Obsidian or BruxZir NOW?
CD: For my practice, if it’s a second molar and it’s a full-coverage restoration, I’m going to use BruxZir NOW. If it’s a first molar and it’s a full-coverage restoration, it really depends. If the patient already has BruxZir in their mouth, I’m going to most likely use BruxZir NOW, or if I’m concerned about their occlusal forces — you know, large men have a tendency to break things — I would use BruxZir NOW in that situation. If the patient doesn’t have extremely heavy occlusal forces, I would feel very confident putting Obsidian in the patient’s mouth. Obsidian is a bit more esthetic and toothlike in appearance. That’s not to say that BruxZir NOW is not toothlike, but Obsidian is clearly a more esthetic material.
NP: So it’s a little bit of a trade-off — you exchange a little bit of translucency to get significantly improved strength.
CD: Exactly. And then for premolars, I use Obsidian exclusively. For inlays and onlays, I mill a couple of other materials. I’ll use VITA ENAMIC® (VITA Zahnfabrik; Bad Säckingen, Germany) and Lava™ Ultimate (3M Company; St. Paul, Minn.), which are both nice materials. These are mainly for inlays and onlays, though. For full crown coverage, I use either BruxZir NOW or Obsidian.
NP: You also restore a fair number of implant cases. How do you incorporate implants into the digital workflow?
CD: You know, that’s my favorite aspect of the digital workflow, and it’s really been great to have the scanner in the office for implants. Each implant manufacturer has a scan body. The scan body attaches to the implant, you scan the implant, and from that scan the lab can determine the position of the implant and design the optimal abutment.
NP: So it’s like the digital version of an impression coping?
CD: Exactly. It’s been a wonderful workflow for our office. The beauty of it is that you can have the abutment fabricated while the crown is being milled, and those two will merge on a lab tech’s desk for verification of fit — and then it’s back in your office. It’s a flawless workflow. We’re getting back digital restorations a lot more quickly than when we were doing traditional impressions with the implant workflow. It’s been a great addition to our office. You’re getting a beautiful custom abutment and restoration, and you can do any type of custom abutment and restoration on it. It’s limitless in terms of what you can do.
Another benefit of having the scanner in the implant workflow comes into play when you’re working with a surgeon. Although I do not place implants, I work with our surgeons to determine where we want the implants placed. We’ll scan the patient preoperatively and then take a cone-beam computed tomography (CBCT) scan, and software will merge that data together. We’ll plan the implant placement along with a temporary restoration, and we’ll fabricate the temporary restoration and the guided surgical stent. The implant surgery is performed, and a temporary is delivered to the patient the very same day. It’s a beautiful service for the patient. In addition, the healing is better for the patients, because they have a temporary that was fabricated specifically for that site. So it’s a wonderful workflow.
NP: That’s great. You know, as I talk to our colleagues around the country who are involved in digital dentistry, a lot of them have some concerns about whether the model is optional. As you mentioned, you can get an abutment from one mill and get a crown from another mill or even a different lab. They go together, and there’s no model involved. How have you adapted to digital dentistry without a model?
CD: It was a hard shift, because I had a little pregame routine I went through when I went to see the restoration that I used the model for. I didn’t receive a model after I sent my first case to Glidewell Laboratories, and my mind was a little bit blown, but the restoration seated beautifully. After sending a few more cases, I realized that the model wasn’t really necessary — and of course I enjoyed the cost savings from not having a model. I still prefer models on my implant restorations, but that’s just because it’s something that I’m used to. I think that working without a model is not a bad thing. It’s something you should try to do a few times, and I promise you won’t be disappointed.
NP: I love your term: the “pregame routine.” That’s exactly what it is. We like to look at the crown on the model, and look at the contacts and how the crown hits against the opposing. However, the truth of the matter is that those things have already been looked at digitally, and they’ve already been established in the design and in the milling. So it’s kind of interesting, and of course the significant cost savings that you realize by not having a model probably helps make the habit change easier.
CD: Absolutely.
NP: OK. Tell me a little bit about your practice.
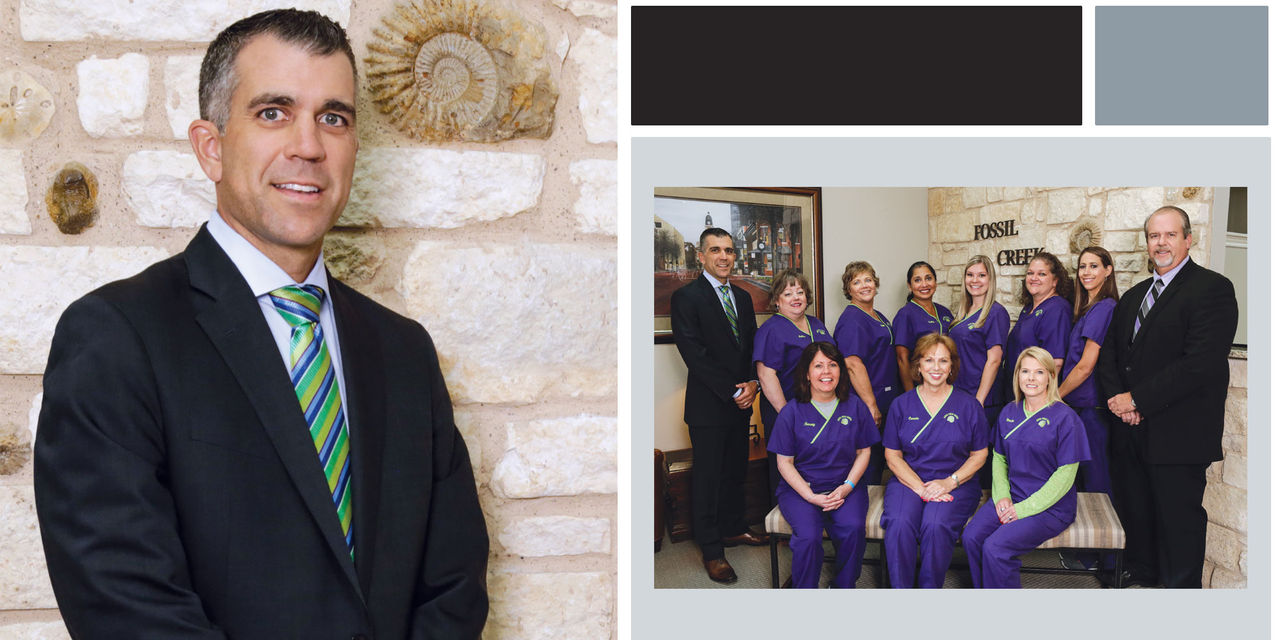
CD: We like to call ourselves an “esthetic and restorative practice,” and we treat patients of all ages, from children to the elderly. There are nine staff members and two doctors. I have been in practice with my partner since 2003, and my partner has been in practice in the Forth Worth area since 1987. It’s been a great transition. We feed off one another, and we practice by the motto, “Two eyes are better than one, and four are certainly better than two.” So we use each other a lot in our clinical decision-making and treatment planning, and it’s wonderful to have that camaraderie between the two of us. We have a wonderful staff that’s been in place for a long time.
NP: You mentioned that your partner is a bit senior to you.
CD: Yes.
NP: And we know that doctors adopt technology at different rates. Has that been the case in your practice?
CD: Yes. I love the guy dearly, but he was very hesitant to adopt the technology, and that’s partially because he saw our challenges with the first two systems that we had. When this new technology came in, he was interested, but he wasn’t ready to completely embrace it. I would catch him occasionally peeking into the operatory to look at the technology, and he’d briefly contemplate the prospect of scanning before changing his mind.
I think a turning point for him came when he had a complex implant case with several units in it — and the patient happened to be his wife. I said: “You’ve just got to scan this case and send it to Glidewell Laboratories. Let’s see how it goes, and we’ll get it back.” And he said, “OK.” I gave him scan bodies, and then he inserted them into the implant. He scanned it and sent it off, it came back, it dropped in beautifully, and now he’s exclusively scanning all of his implant cases. He’s starting to scan some crown & bridge restorations, and I recently helped him fabricate his first chairside restoration — which dropped in beautifully.
So it’s been a slower shift for him, but now that he’s seeing the merits of the equipment in the office, I think that he’s going to start using it with much greater frequency. I think that it’ll be a great addition to his practice as well as to mine, and I’m hoping he gets to the point of using it enough where we’ll have to purchase a second scanner.
NP: It sounds like you’re both benefiting from the partnership.
CD: Absolutely.
NP: How has this adoption of new technology worked out for your staff members?
CD: Whenever I tell them I’m bringing something new into the office, it doesn’t matter how small or big it is — I get the eye roll. They know me well enough to know that some of the things I bring in become part of our everyday routine, while others get stuck in a closet.
NP: Right — “Let’s dig in, and maybe this will all blow over.”
CD: Yes. They rolled their eyes when I brought the scanner in because my staff’s been with me for a long time. They saw our first two systems come and go, and now they were there for the third. We started using it, and I was determined this time for us to make it work. I thought: “The workflow is proven and the technology is there. Let’s do this.” And my staff has really embraced the technology. When we had the scanner in 2007, I would place the scanner in the room, yet when I’d walk into the room, the scanner would be in the hallway and the impression material would be next to the patient, because they knew that was what I was going to do anyway. They knew it was going to be easier and quicker for me to not use the scanner.
Now I don’t even have to tell them — the scanner is in the room and it’s ready to go. In a lot of cases, my staff has actually coaxed me into using the scanner. I would never have done my first partial with a scanner unless my staff said, “I think we should try and scan this.” For my first nightguard, my assistant said, “I think we should try and scan this.” So we’re scanning everything that we’re doing. They’re loving it and I’m loving it. They’ve really embraced the technology.
NP: That’s great. I appreciate the effort that you’re making to bring all of us in the profession into the future. What trends are you seeing in digital dentistry?
CD: The continually increasing number of scanners and mills in the marketplace is going to force the manufacturers to really step up their game. I think there’s a lot of behind-the-scenes stuff that’s going on, with manufacturers staking their claim that they’re the best, they’re the most accurate, they’re the market leader. I think there are a lot of changes, which creates a lot of confusion, but there’s also a lot of good products on the market. And if it’s not a good product, it’s not going to make it to the market. I see the cost of the units possibly even coming down over time, but I think there’s a limit as to how far they can come down.
I also see the laboratories will follow Glidewell Laboratories by going almost exclusively digital. They’ve already embraced the technology that’s benefited them, whereas before it really hurt them. So I see a lot of change in the future, and I think it’s all going to be for the better. I think that the indications are going to continue to open up among the scanners and mills. I think the milling choices are going to be greater, and I think the future is bright for digital dentistry and clinical dentistry in general.
NP: Some great thoughts. Thank you so much for joining us today.
CD: Thank you.




