Biologic Shaping

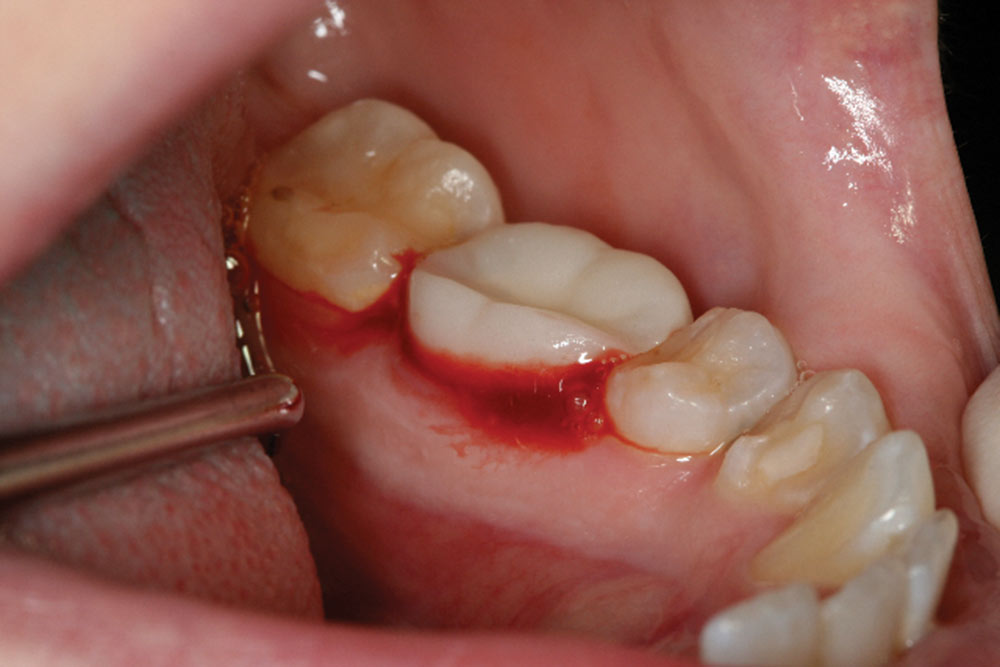
When performing conventional crown lengthening, the previous margin of the old restoration is used to determine the necessary amount of bone to be removed so there will be adequate space for the biologic width. By adequately creating a space for the biologic width, the new margin will not infringe upon it.
A potential problem of this procedure is that a significant amount of bone will be removed, weakening the tooth or creating a weakened furcation area. The more bone removed in the furcation, the greater the likelihood of future problems with maintenance. It is critical to try to preserve as much bone as possible in order to support the tooth, especially in the furcation area. The clinical prerequisites and steps for success with biologic shaping are as follows:
- All previous restorative materials and decay should be removed.
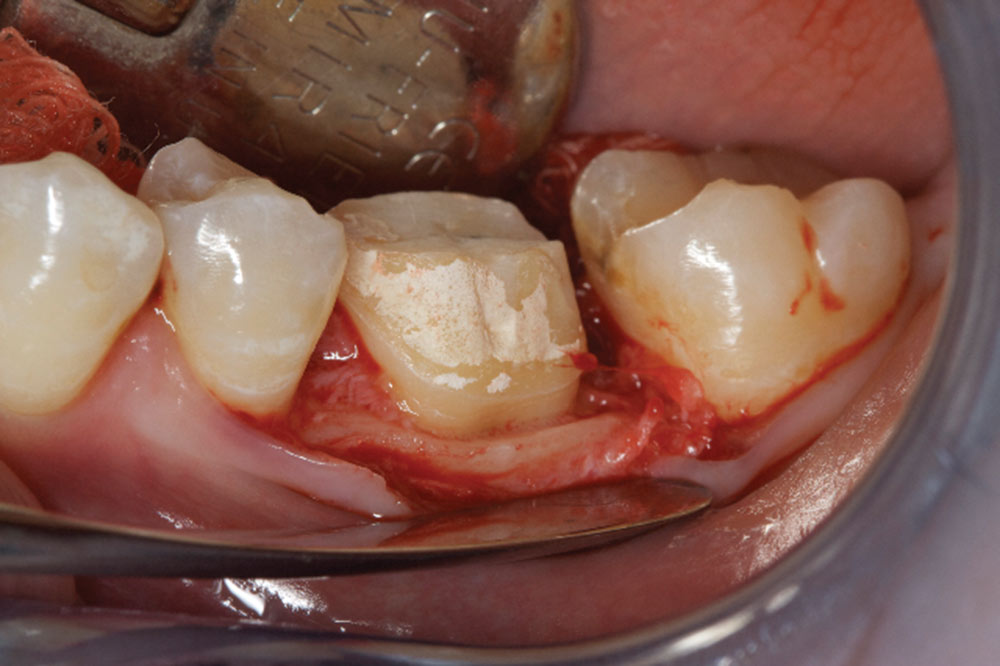
- A core buildup should be placed where necessary to add volume to the teeth. The material should be a composite-bonded resin. The core helps the periodontist determine where the final margin placement of the new restoration will be.
- Acrylic provisionals should be placed with Durelon™ (3M™ ESPE™; St. Paul, Minn.) temporary cement. Durelon is antimicrobial and helps decrease sensitivity.
- Remove provisional at time of surgery for access. Ideally, a mosquito forcep is used with a gentle rock at the incisal third of the occlusal surface of the provisional.
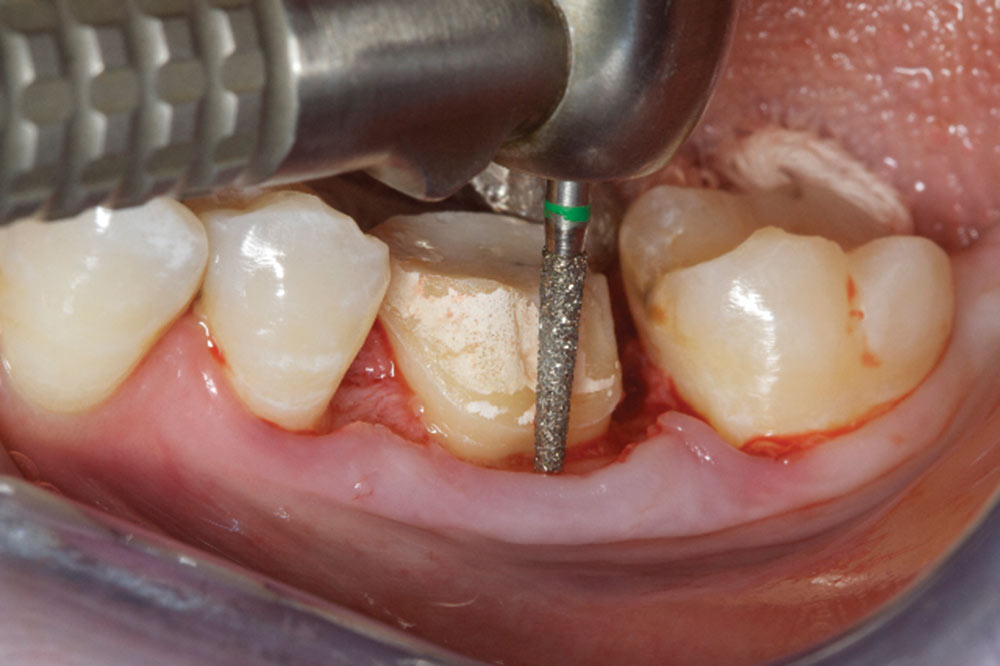
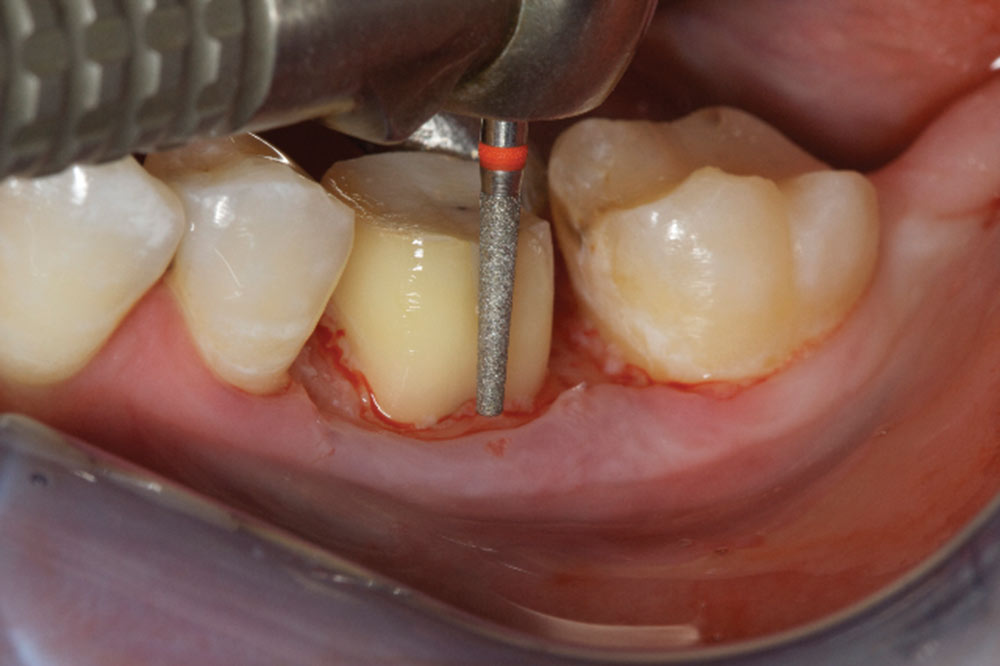
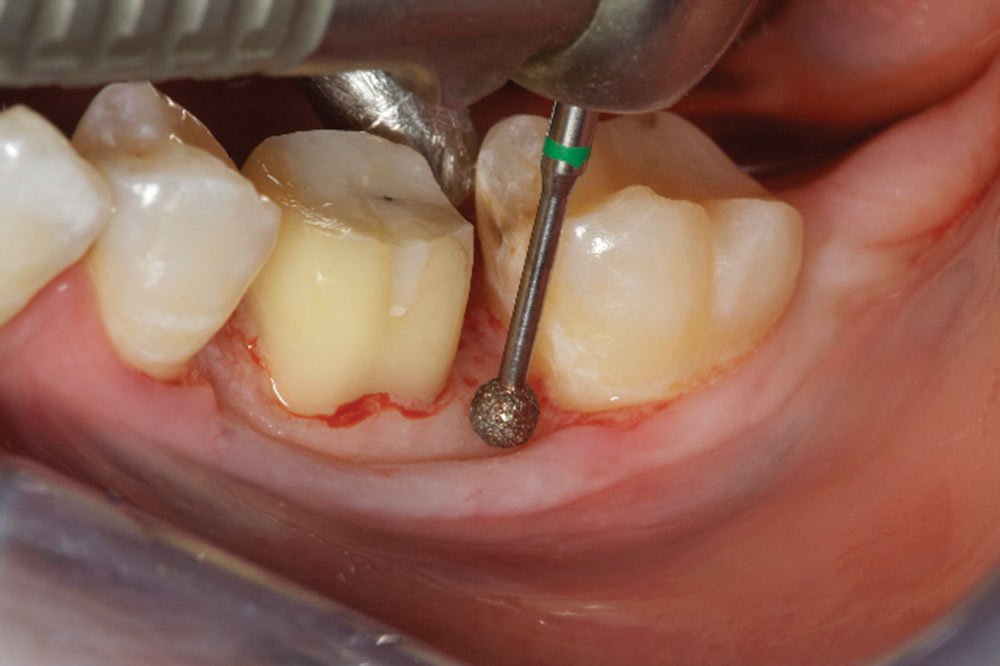
- Shape the tooth surface and remove old margin, as well as 360 degrees of CEJs. A flat-ended bur with a 4-degree taper is best for biologic shaping. A diamond grit is best.
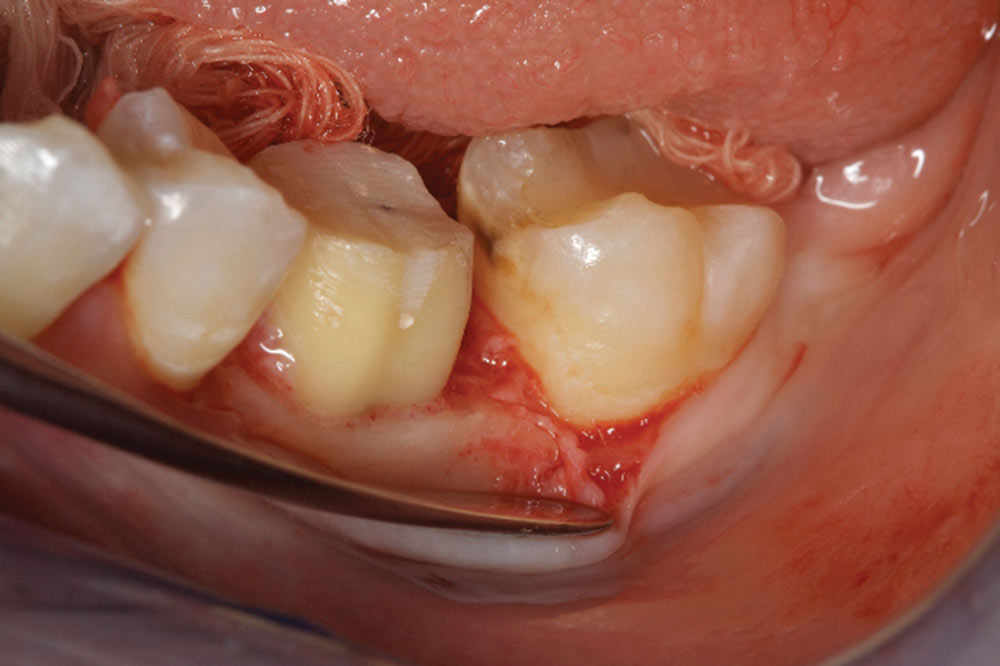
- Correct any reverse architecture and remove any necessary bone where biologic width issues are still present. The goal is to create an osseous contour identical to the soft tissue contours that take place when forming a new biologic width.
- Add sufficient connective to protect the bone from bacterial infiltration. The connective also protects underlying periodontal tissues from impression material and cementation irritation.
- Once the flaps are adapted using 5-0 chromic gut suture just coronal to the osseous support, potassium oxalate should be used to help decrease sensitivity. The liquid is applied to the root surface for 45 to 60 seconds and then lightly air-dried. Repeat two to three times.
- Cement provisional with polycarboxylate cement (i.e., Durelon or DENTSPLY Tylok®; York, Pa.). Tylok may be more ideal for cementation during surgery, as it is water-soluble.
- Homecare consists of chlorhexidine used twice daily, in both the morning and evening. PreviDent® (Colgate; New York, N.Y.) should be used at bedtime to help decrease sensitivity. After meals, the patient should rinse with water or Listerine to remove excess food particles.
- At four weeks, the provisionals are either remade or relined leaving 1 mm of space to allow for continued biologic width growth in a coronal direction. No margination of the tooth surface should take place at this time.
- At 14 weeks, chamfer margins are placed just coronal to the gingival collar and impressions are taken. A recommendation of one #7 SilTrax® (Pascal Company; Bellevue, Wash.) cord be placed in the sulcus for retraction of tissue. When endodontics is present the new margin may be placed within the sulcus. In these cases, a ferrule effect is recommended.
Reasons for Biologic Shaping
- Replace or supplement the current indications for clinical crown lengthening.
- Minimize removal of supporting osseous structure.
- Facilitate supragingival or intrasulcular margins to preserve the biologic width.
- Eliminate developmental grooves.
- Eliminate previous subgingival restorative margins.
- Reduce or eliminate furcation anatomy and thus facilitate margin placement.
- Allow supragingival or intracrevicular impression techniques.
- Facilitate hygiene and maintenance procedures.
- Reduce or eliminate cervical enamel projections.
- Facilitate ideal restorative emergence profile. Flat is better than fat contours.
Daniel J. Melker, DDS, is in private practice and can be reached at 727-725-0100.