The Deceptions of Rubber Gloves

It has been more than 25 years since the public panic over AIDS, hepatitis B and infection control prompted government agencies to mandate the use of examination gloves in dental the practice. In response to public outcry, the American Dental Association (ADA), the Centers for Disease Control and Prevention (CDC), and the Occupational Safety and Health Administration (OSHA) established guidelines for infectious disease control that include the routine use of eyeware, face masks and gloves by dentists and their staff as a way of preventing the spread of disease in dentistry. For the most part, these guidelines have been significantly ineffective and, in many cases, harmful. It is time for a change.
To many clinicians and public health scientists, using gloves, masks and eyeware when treating patients seems reasonable and rational. Although these devices are generally assumed and touted to protect both the patient and the dental staff, many dental scientists and clinicians seriously doubt the effectiveness of masks and gloves, citing the rarity of any disease transmission and numerous hazards associated with their use.1-45 In this article, I will focus on examination gloves and document evidence-based facts that support the notion that glove use has been recommended on an unscientific basis and can increase the risk of infection rather than prevent it. Now that the AIDS scare of the 1990s has passed, and the disease is better understood, dependable scientific data is available to back this claim. It is time for a nonemotional re-evaluation of “protection.”
Government regulations, expanding the recommendations of the CDC, now require dentists to wear gloves with all patients. This may not be in the best interest of either the public or the dental professional. It has been proposed that the original recommendations of the CDC be re-applied. Those recommendations state that “gloves and protective ware be recommended, not mandated, for dental care and the use of these tools be determined by the clinician on a case-by-case basis where the benefits to the patient and safety of the dental staff be the prime focus.”
The Use of Gloves
Since 1985, concerns about AIDS and hepatitis B virus (HBV) have renewed emphasis on infection control and the use of barrier-protection devices in dental offices. From the original CDC recommendations, a variety of preventative extrapolations have been made by numerous self-proclaimed experts, organizations and manufacturers in an attempt to one-up each other while seeking wealth, attention and power. These recommendations have a great emotional appeal and range from the use of thicker glove materials and longer lengths to double- or triple-gloving. The ADA, CDC, OSHA and many state dental boards have recommended or mandated the use of gloves for all patient contacts.1,2 Most dentists and their ancillary staffs wear gloves, most often composed of latex, which gives the best control and dexterity of all available glove materials.3 These elaborate exposure-prevention guidelines are based on a minimal amount of scientific data concerning the efficacy of barrier protection against viruses in a dental setting.4,5 Almost all of the scientific data concerning safety and glove use in dentistry are extrapolations from the medical field. The use of gloves by health care personnel has been accompanied by a heightened incidence of glove-related problems.36,38 Knowledge of these serious problems has been ignored or suppressed by many dental institutions in an effort to create a false sense of security among dental workers and patients who are led to believe that practicing Universal/Standard Precautions will protect them from all infections and dangers inherent in dental practice, and that not using Universal Precautions will doom them to certain death.
Barrier Protection and AIDS
Unlike glove materials, there are no known bacterial, viral or fungal life forms that are capable of penetrating intact skin.5 Intact skin is the best protection against infection. Nonsterile (contaminated) latex exam gloves are the choice of most dentists not only because of their lower cost but also because they interfere with dexterity considerably less than poorly fitting vinyl/nitrile gloves. Due to economics, few dentists use the more expensive sterile latex gloves for nonsurgical treatment. Before the 1990s AIDS panic, only about 20% of America’s dentists wore gloves, and this reflected concern mostly about HBV.7,8
Unlike glove materials, there are no known bacterial, viral or fungal life forms that are capable of penetrating intact skin. Intact skin is the best protection against infection.
Before 1986, preventing HBV by wearing gloves was only occasionally mentioned in the literature.9 At that time, most dentists chose to operate bare-handed because they favored superior dexterity over questionable barrier protection.7,8 Occupational infection of dentists or staff members was rare and even more rarely reported. In those relatively few HBV cases, the virus was transmitted by accidental needle sticks for which gloves would not offer protection.1,9 The rarity of dental-related infections (HBV, herpes), low mortality rate and the recent development of HBV vaccines has made HBV a relatively preventable disease and therefore of less concern than in the past.10
AIDS, more than any other disease, prompted interest in barrier protection.1,2,3 This poorly understood, fatal (now chronic) disease originally inspired fear and panic among the health care, government and public communities.11 In the 1990s, fueled by media attention, civil rights of gay people, and governmental and scientific politics, AIDS took on the undeserved reputation as the nation’s “number one” disease. In reality, cardiovascular disease, cancer and diabetes killed millions more people each year.
The U.S. mortality rate for AIDS (2007) is 14,561 persons per year.12 This is a statistically insignificant number (0.0005%) compared with the total population of the U.S. (305 million), yet it was once the highest funded and publicized disease.
Fear of contracting occupational-derived AIDS caused many professionals to quit their jobs or deny HIV/AIDS patients humane care. This irrational fear — fed by unsubstantiated anecdotal stories of infection from media, politicians, activists and “safety” merchants — required extreme action from the government and the surgeon general at the time, Dr. Charles Everett Koop. The CDC responded to the call with the concept of Universal Precautions. This was a form of cover-up ritual with enough emotional and quasi-scientific appeal to placate the professional and nonprofessional populace. Patients relaxed and those with HIV received treatment.
The technique of “protecting” oneself has been used throughout history. Although ineffective, it calms widespread panic. During the 14th century plague in Europe, physicians “covered up” in special cloaks to confuse the disease devils (Fig. 1). In the 1918 swine flu epidemic, useless cloth masks covered many faces in an attempt to protect from the flu, which killed 60 million people. (Some people were shot for failing to wear a mask.) In the 1950s, in preparation for a nuclear war, schoolchildren were taught to duck and cover under their desks (and not to run to the nearest bomb shelter). In the 1990s it was gloves, mask and eyeware to “cover” the skin and stop the spread of AIDS, which can only be transmitted from unprotected sex and IV drug use.
The first case of AIDS was reported in 1959, and since there have been no documented cases of occupational HIV infection in any dental health care worker.1,13 There have been billions of dental patient visits worldwide with no disease transmission. There is one botched CDC investigation involving Dr. David Acer, an openly gay Florida dentist with HIV, who was alleged to have infected some patients (with secret high-risk behaviors). But even Dr. Acer wore gloves during all patient contact. In 1992, the U.S. General Accounting Office investigated and reported that this case was so bizarre, and the CDC did such a poor job in its investigation, that no reliable public policy should be drawn from the matter.14,15 The GAO report did state that “gloves do not prevent most injuries caused by sharp objects, however, and so do not necessarily reduce contact rates.”14 The CDC also published six to seven “possible” HIV transmissions in dentistry, but these, in the words of CDC officials, “were short on science.”17
Primarily because of HIV-AIDS concerns, universal barrier protection, including the wearing of gloves, has been recommended and/or mandated for all dental staff when in direct contact with a patient.1,2,3,7 This recommendation is still in effect. This has increased the use of gloves, along with problems associated with their use, for both staff and patient. Knowledge of these problems and hazards and the option of wearing gloves in appropriate situations are important for the health of the dentist, the dental staff and the patient.
Mechanical Hazards of Gloves
Gloves pose a number of mechanical problems for the wearer:
Gloves do not offer protection against needle punctures, the leading cause of HBV and HIV infections in health care workers.1,2,13,14,16 Eighteen of the 25 healthcare workers in North America and Europe who reported HIV occupational seroconversion during the years when AIDS first became a concern developed their infections from large-gauge needle puncture wounds.1,13 This percentage has increased substantially over the years as the few new contamination cases reported needle stick-sharps injuries as the prime cause of seroconversion among medical staff. There have been no documented cases of dental staff occupationally seroconverting. Sharp punctures are not prevented by gloves.1 In fact they have been shown to increase penetrating injuries.17,18 The hazards of reduced touch sensation caused by gloves tends to contribute to clumsiness, which often results in increased skin penetrations due to the insulation of proprioceptive nerve endings in the skin of a dentist’s hands.17,18 Solovan, et al. reported 2.3 times as many tissue lacerations in dental prophylaxis patients treated with gloves compared with work done bare-handed.8
- In the largest clinical dexterity study to date, 50 dentists who practice in Lake County, Illinois, were tested for the average threshold for perception of light touch using a dynanometer.18 Results were 4.4 grams without gloves and 6.7 grams with their favorite gloves, which represents a 52% reduction in light-touch proprioception. There was a 16-fold increase in percutanious injuries while manipulating endo files (gloved) in a manual dexterity exercise as compared to the same dentists working bare-handed.18
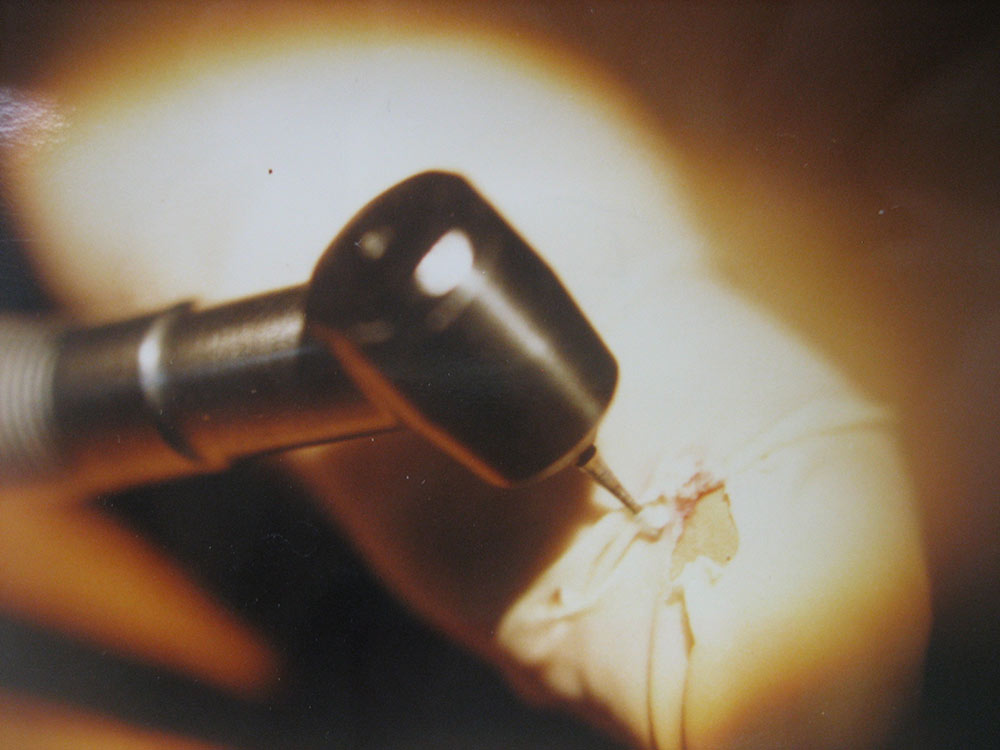
- Dental burs, especially those designed to cut acrylic, tend to snag the late rubber and drive the bur into the flesh of the operator’s hand, creating a deep penetrating wound19 (Fig. 2). There is considerable danger in wearing gloves around rotating machinery.
- Dental lathes and rotary devices can snag gloved fingers and have caused bone fractures among dental personnel.20
- Both latex and vinyl gloves are flammable and pose a danger with the use of open flame (e.g., wax in prosthodontics)21 (Fig. 3).
- Gloves increase the difficulty of handling small instruments such as pins, burs and endodontic files.18,21 This impairment increases the time required to perform normal dental procedures and increases the opportunity for drop and aspiration accidents.22
- Gloves are also poor barriers to many solvents used in dentistry, such as alcohol, eugenol and methacrylates, as well as composite bonding agents and some impression silicones.36,37 This allows contaminates to enter the gloves.
Problems with Barrier Protection
The primary purpose of the gloves is to provide a barrier to the transfer of microorganisms and other agents. They are fairly effective against organisms that are 10 microns or larger (e.g., bacteria), but there is little evidence that they effectively protect the wearer from viruses encountered in practice.9,23 There have been numerous studies done that show minimal benefits for those who wear gloves.9,15,24
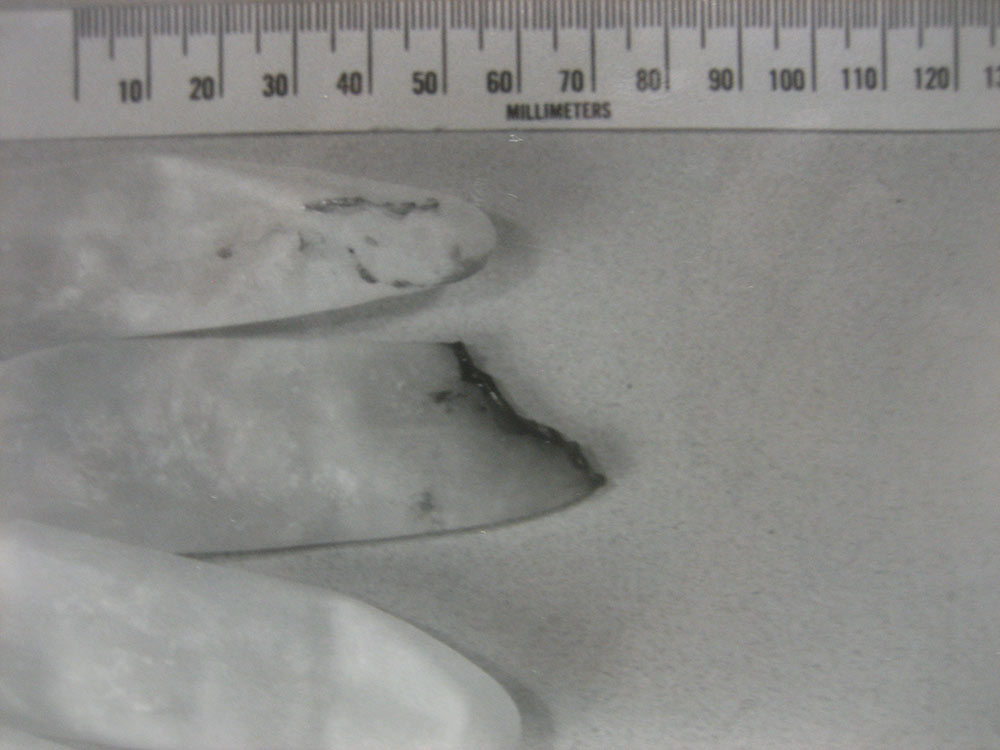
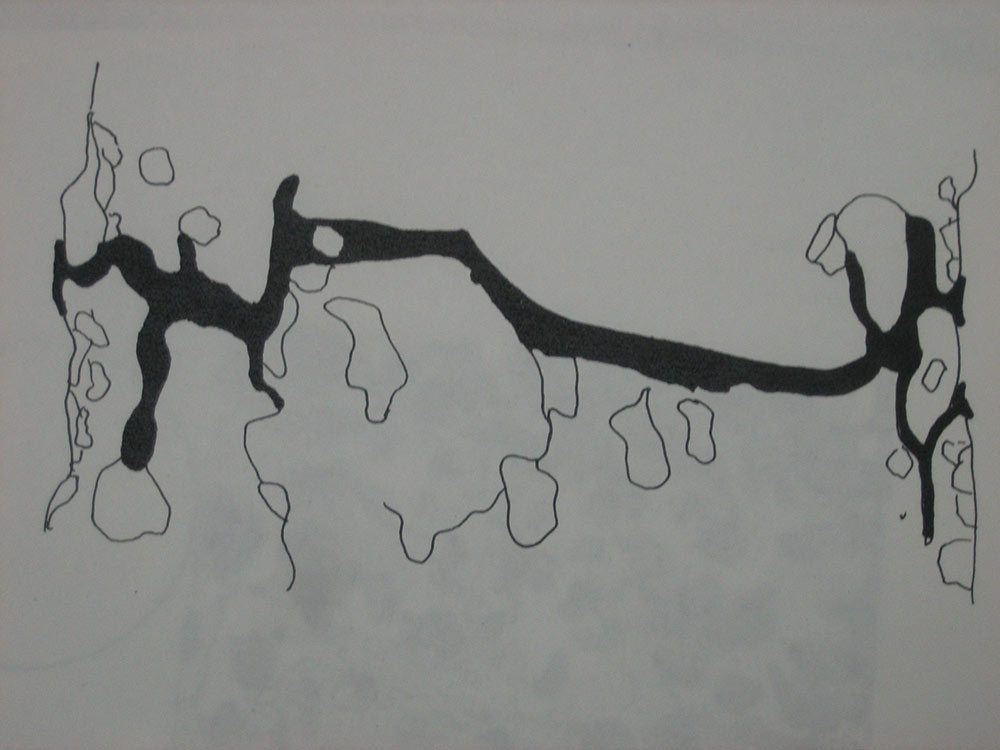
New latex gloves have numerous porosities that are three to 15 microns in diameter.24 These porosities increase in size and number when the gloves are stretched and used. Ten micron voids are the smallest imperfections that can be detected by usual testing methods.24,26,27 The capsid of HIV is 0.1 to 0.12 microns in diameter.27 A hundred of these viruses could pass side by side through one of the “natural” 10-micron openings in latex gloves. The HBV virus of hepatitis B is even smaller, 0.042 microns, which may partially explain why it is more infectious than HIV29 (Fig. 4). Vinyl and nitrile gloves have significantly more rips and openings.
Besides their natural porosity, latex gloves frequently have manufacturing defects in the form of visible holes 50 microns or larger in diameter.27,30 From 2% to 36% of unused latex gloves and 23% of unused vinyl gloves examined had tears or holes that could allow fluids in a patient’s mouth to leak into the glove, causing “wet finger syndrome.”26,27 These voids increase in size and number as the latex is worn or just exposed to atmospheric ozone28,31 (Fig. 5). This was corroborated in a report by Brough et al., which revealed holes in 37% to 70% of used postoperative surgical gloves.32
In separate hallmark studies, both Reingold9 presented data showing that the use of gloves provides dentists little protection against HBV. Reingold studied 434 oral and maxillofacial surgeons and found that only the number of years in practice correlated with the number of infections these surgeons had incurred. The use of gloves showed no increase in protection. Gonzalez reported only a less than 3% decrease in HBV prevalence for dentists who wore gloves routinely compared with those who did not. His conclusion, that gloves are effective barriers, was criticized because it did not support his own data, which was statistically insignificant (p=less than .05). Reingold observed that many of Gonzalez’s HBV-positive reactors had more years in practice than glove-wearing nonreactors, which explained the greater number of HBV cases.9
Most reports on the effectiveness of gloves against viruses involve assumptions only. Hadler’s report,34 which is unique because it was distributed by the CDC, is a typical example in which HBV was supposedly transmitted to patients by an oral and maxillofacial surgeon carrier. Prior to this discovery, the surgeon did not routinely wear gloves. No other HBV transmissions were noted after he began wearing gloves. The conclusion was that the gloves prevented further transmissions. Omitted from consideration was the later discovered shorter incubation period for HBV infection, the probability that the surgeon’s carrier status changed and that newly infected patients did not immediately test positive after the test surgeon began wearing gloves. This and three other similar studies were extrapolated by the CDC to apply to HIV infections and became the prime “scientific” rationale for the recommendation that gloves be worn as an element of Universal Precautions.1 At that time, the AIDS epidemic was peaking and any rationale, scientific or not, would suffice for CDC action.
Eventually, the errors in this study forced the CDC to recant and recommend that vaccination be the only effective preventative measure for HBV. Retracting Universal Precautions would be embarrassing and spark the AIDS panic again and thus was not implemented. This constituted an official deception that had serious future consequences.
Gloves: An Expensive Contamination Hazard
Most dentists use nonsterile latex gloves instead of sterile gloves because of their lower cost.6 A 100-pair box of nonsterile exam gloves costs between $5 and $11 at most supply firms. Sterile gloves usually cost 10 times as much ($50–$95). The average dentist and staff uses $4,000 worth of nonsterile gloves per year (36 patients a day).11 Extrapolating to the 150,000 dentists in America, the nation’s annual cost for dental gloves comes to at least $600 million. This is a tremendous expense for minimal to no benefit, because the wearing of gloves in dentistry has shown no significant improvement in reducing HBV (now addressed by vaccination) or AIDS (no documented cases of occupational transmission in dentistry before or after 1985). To invest this level of resources for a useless exercise defrauds the dentist, who pays the supply bill, and the patient, who pays the dentist.
Because the CDC and OSHA are primarily interested in protecting the dental staff member rather than the patient, the contamination potential (for patients) of nonsterile exam is placed secondary to the costs of glove supply. Both organizations, however, sensibly recommend sterile gloves for some surgical procedures. It is ironic that the nation’s health organizations insist on stringent infection control measures and advertise the fact as a safety promotion to the public, yet what they are advocating is that dental staff use contaminated (infected) exam gloves, rather than freshly washed and disinfected hands as was done before 1985.
Of course, using sterile gloves for all procedures would increase the cost of providing dentistry to such an extent (more than $5 billion annually) that no one would be able to afford dentistry. It is estimated that using sterile gloves as we do examination gloves would cost each dentist $40,000 more in supplies each year.11 In spite of this, infections from bare-handed and gloved (sterile/nonsterile) dentists have been historically very rare and insignificant. Evidence-based science shows it doesn’t matter whether you wear gloves, and it never did. Yet dentists continue to believe that placing contaminated gloves on a compromised patient’s oral mucosa is safe and beneficial.
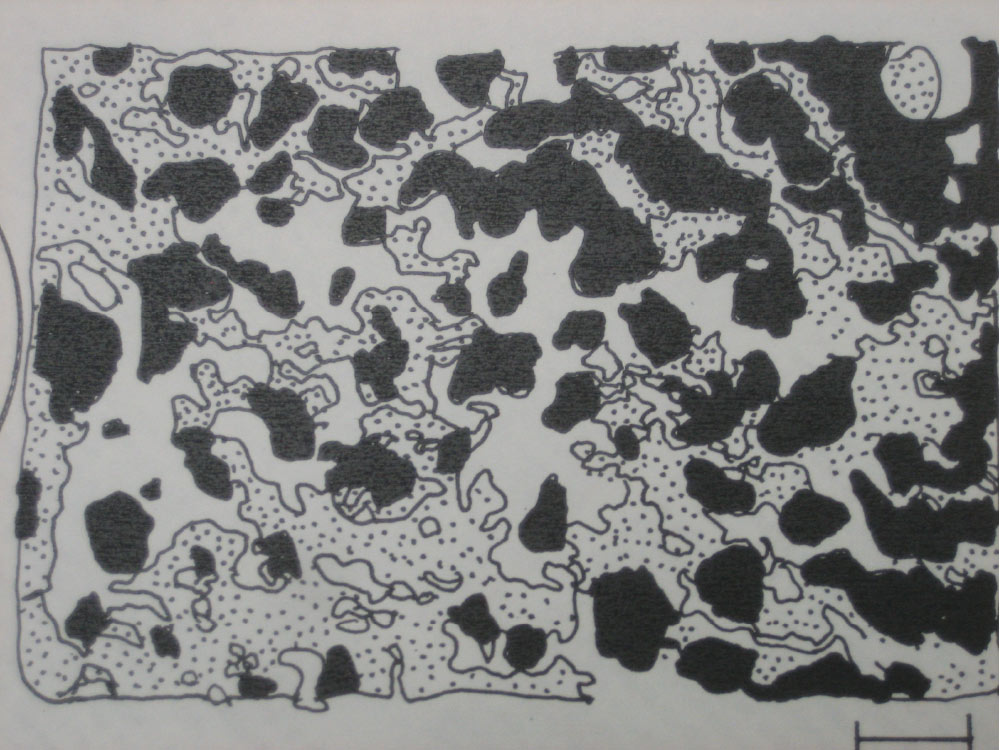
This is with the consideration that most latex glove products are manufactured and hand-packed in Third World countries, where facilities are hygiene-primitive and the bathroom hygiene of many latex workers consists of using the left hand as toilet paper. Soap and clean water is a rarity (Figs. 6, 7). Because exam gloves are considered already contaminated (nonsterile), they are seldom checked for pathogens. It is assumed that contaminated gloves are not clean. The hope is that they will be “kitchen clean,” which the CDC, dental organizations and dental boards assume is good enough for the population.
Microbe contamination is not the only problem. Gloves often are coated with talc or cornstarch, which act as lubricants and absorbents. There are problems with this, most notably that talc and starch are physical irritants.36,37 They can cause inflammation in lesions on the wearer’s hands and can irritate wounds in the patient. Latex rubber ingredients have been identified as contributing to various degrees of dermatitis, as well as local and systemic allergic reactions.39 Both talc and starch are irritants when inhaled and can cause asthmatic exacerbations in susceptible individuals.28,36,40 The talc and starch will absorb latex proteins, become airborne and get inhaled by susceptible individuals. This can cause life-threatening conditions to breathing-compromised people (e.g., asthmatics). The incidence of latex sensitivity has increased from 3% to 6% in the general population since 1985 concurrent with widespread latex glove use. Some researchers consider this to be an epidemic in itself. The incidence of latex sensitivity in the dental community has soared from 3% to more than 22%.47 This appears to be the direct result of wearing latex gloves and exposing skin and mucosa to the allergenic protein, as this problem did not arise until gloves became mandated. This is a dangerous change of events: Many deaths and thousands of serious reactions have been reported due to the increased latex exposure.47 Another deception dentists and patients face is that gloves not only won’t be of much help in preventing disease, but they can cause considerable morbidity and mortality for which our patients and staff are seldom warned. This situation wastes money, endangers lives and discredits the dental profession.
This is with the consideration that most latex glove products are manufactured and hand-packed in Third World countries, where facilities are hygiene-primitive and the bathroom hygiene of many latex workers consists of using the left hand as toilet paper.
Starch is easily broken down into simple sugars that provide an ideal growth medium for microbes and contribute to bacterial and fungal growth on the warm hands of a glove wearer. This increase in resident and “leaked” microbial growth presents a danger to both the patient and the operator.28,32 The components of latex (and other) gloves have been implicated as contamination hazards that may contribute to urticaria, nonhealing wounds, asthma, facial edema and toxic shock in health care workers.30,38,41 Forty of the 50 dentists (80%) in a Lake County, Illinois, study wore gloves at least 85% of the time.21 Twenty-five (50%) of these dentists reported hand lesions concurrent with the wearing of gloves. Three of the remaining 10 dentists, who intermittently wore gloves, also reported hand lesions. All but one of these dentists attributed the lesions to the wearing of gloves.18 Tightly fitting gloves keep contamination close to the wearer’s skin surface. This increased contact encourages growth and spread of pathogens and increases the likelihood of allergies and/or reactions.
Nonsterile gloves are not only contaminated during manufacture but are also quickly contaminated by the natural flora of the hands. To illustrate, this author did an experiment. Thirty-one unused, multibrand, nonsterile gloves were swabbed with sterile saline/cotton swabs and individually plated on typto-soy media. Cultures were incubated for 24 hours. Six (19%) of these gloves were contaminated with gram-positive cocci, spore formers and fungi. There are numerous other studies that repeat these findings.16,23,24,26,29
Considering that these microorganisms are augmented with a starch growth media, warmth and moisture from the wearer’s hands, the potential for increased contamination and skin breakdown of both the wearer and the patient is greatly increased. This is why the CDC recommends that dental health care workers who have exudative lesions or weeping dermatitis, particularly on the hands, should refrain from all direct patient care and from handling dental patient care equipment.1 Because most dentists and their staff have microbreaks and other skin lesions as described above, obeying this order would essentially furlough 20% of the nation’s dental staff at any one time.
Allergy Hazards of Latex Gloves
Urticaria is a common complaint associated with the use of gloves.36,39 In a Lake County, Illinois, study, half of the glove wearers experienced dermatitis.18 Increased IgE reactivity of wearers and patients has resulted in thousands of lifethreatening allergic reactions, such as anaphylaxis and asthma, to latex glove materials.39,40,41 Additional allergic problems have resulted from the starch or talc used inside the gloves.36 Contact with latex gloves by sensitized individuals has been life-threatening, as mentioned above.39,40,41
Between 1988 and 1992, the FDA received reports of more than 1,100 life-threatening systemic and 15 fatal reactions to latex. In recent years, as the population continues to be sensitized to latex (e.g., rubbing a gloved finger along the oral mucosa), this rate of anaphylaxis cases continues to increase. Both dentist and patient are at risk, and the deception that everything is safe cannot ethically be maintained.
Miscellaneous Hazards
Gloves also produce other problems not previously mentioned.
- Latex has a negative taste and “sour rubber” odor to many people.42 Multi-flavored gimmick gloves are a poor attempt to correct this problem.
- Hands are compressed by the elasticity of latex gloves. This restricts the flow of blood, which increases tension and muscle fatigue.43 Although proper fit is important, the recommended snug fit is a disadvantage of glove use due to the elastic nature of latex and the wearer’s nerve pathology caused by the constant compression.35
- Gloves impede productivity by restricting movement, limiting manual dexterity and consuming time while gloving and degloving.22,37,45 Assuming it takes 30 seconds to put on or take off gloves for each patient, a dentist who treats 100 patients a week for 50 weeks of the year loses 83 hours of productivity annually. This makes dentistry less efficient and more costly, and deprives the relative poor of needed care.
- Many patients, especially small children, are offended by the use of gloves.35 They interpret gloves as a threat or as an insult that they are dirty or diseased. This level of mistrust interferes with positive doctor/patient relationships.35
- The use of gloves has become an issue among the media, patients and dentists.4,35 Many patients insist on being treated with or without gloves based on information gleaned from magazine articles, news reports and word of mouth. Most patients believe gloves are being worn for their protection, but OSHA recommends barrier protection for the expressed benefit of the dentist and other members of the dental staff, not the patient.2 There will be serious consequences when the media learns that most dentists are treating their patients with contaminated exam gloves.
- There are additional problems associated with wearing gloves. The use of adhesives, impression materials and electric pulp testers, which require direct skin contact, are all compromised.45
- Gloves are made of latex and plastic, which deplete natural resources, divert crop land (in the starving Third World) from food production and engorge our limited waste landfills with useless, unrecyclable garbage. If not buried, most gloves, being considered medical waste, are incinerated, producing hydrocarbon air pollution and CO2, and increasing the effects of global warming. Therefore, gloves are not green.
Politics
The most serious deceptions are in the political arena. The directives on Universal Precautions came from the CDC, a branch of the U.S. Department of Health and Human Services. This decision was made by a closed committee of public health bureaucrats, most of whom had never been in dental practice. It was an attempt to silence the AIDS panic, not to find the most efficient form of disease prevention.
Surgeon General Koop devised and promoted his UP concept for medical and dental personnel without any consideration of cost or effectiveness or outside input. On Oct. 29, 1999, The New York Times printed an expose reporting Koop was financially tied to a prominent glove firm, Allegiance Healthcare Corp. The article stated that he had received options to purchase 500,000 stock shares of the firm for a 1994 (low) price in exchange for four lectures per year and advertising rights to his name. This involved millions of dollars. Koop was accused of also trying to downplay the allergy danger issue in Congress because, as he told CDC representatives, “It would cause more harm than good and frighten hospital workers out of using gloves.” Eventually Koop ended up with a failed health care website, worthless stock, angry investors and a TV ad contract to sell “first alert” medical warning devices to the elderly. It seems that science was not a part of this formula.
It is amazing that dentists, their organizations, OSHA, dental boards and America as a whole accepted the pronouncements from the CDC, an organization of questionable authority and candor, without debate. The CDC has flubbed many health initiatives, the latest being the severity and criticalness of the H1N1 flu outbreak and botched vaccine supply.
In 1976 it also went out on a limb, declaring the swine flu of that year was the 1918 variety. It was not, though useless vaccines were distributed to the nation with hundreds of deaths and thousands of hospitalizations from adverse reactions. The anti-HIV cream Noroxnol-9, promoted by the CDC, was found to enhance the spread of AIDS, not hinder it. Former Surgeon General David Satcher called the CDC labs a national disgrace. Congress criticized the CDC for changing the definition of AIDS, thus doubling case numbers in an effort to garner more funding.17 This sad episode was termed by the CDC as “the distortion.”
Strange schemes appeared in the journals, such as ads stating, “Patients love headbags” or “$20 precision, plastic individual handpieces.”
A long series of crises, scandals, reorganizations, mistakes, policy flip-flops, infighting and political interference has left the CDC with a legacy of questionable competence. Because most infection control procedures are based on this flawed organization’s recommendations, dentists would be best served to be more critical than accepting of such government edicts.
The second area of political deception lies in dental publishing. Originally, a few articles on gloves and other PPEs appeared in 1980s journals rebutted by other papers opposing their routine use. As time went on, increasingly more journals printed unsubstantiated horror stories of dentists getting AIDS from patients and other rumors. They published increasingly bizarre recommendations from so-called infection control gurus increasing the panic. This brought attention and sold issues. Advertising for disposable (e.g., glove) manufacturers went from 3% to 25% of most dental publications’ ad space with the accompanying (financial) pressure on editors to avoid infection control criticisms, which would hurt business. Strange schemes appeared in the journals, such as ads stating, “Patients love headbags (a paper isolation bag with a hole for the mouth)” or “$20 precision, plastic individual handpieces (to ensure sterility and cracked enamel).” Some major dental organizations, profiting from the increased attention, adverted in their journals and took on the lead to perpetuate the deception that dentists were in danger of AIDS. They accepted whatever the CDC handed them, because protesting or questioning had some degree of political risk. Instead, they embellished the recommendations of extremes (e.g., heat sterilization of handpieces) to the detriment of the practitioners and their patients. Few journals protested and fearful dental staff embraced the deceptions with lemming enthusiasm.
Conclusion
Gloves are imperfect. They often contribute to the breakdown of the natural skin barriers. They are poor barriers to the transmission of viruses because of numerous voids derived from manufacturing and use. Gloves are cumbersome for the dentist to wear. Gloves are costly and allergenic, contain irritants, and breed microorganisms. The wearing of gloves is beneficial at times (e.g., deep surgery) but can be hazardous at others. The wearing of gloves should not be mandated by government edict but left to the discretion of the dentist in situations where the wearing of gloves provides more benefit than liability. As costs and glove-related illnesses increase, there is no rational scientific reason to continue routine glove use. It is time for dentists to decide what is best for their patients, not bureaucrats and hucksters. It is time for re-evaluation of glove use on a case-by-case basis.
What can be done? If the contaminated/sterile glove issue becomes public, there will be extreme pressure to replace exam gloves with expensive sterile gloves. Each practice will be required to spend at least 10 times more money on glove supplies. How much will this cost you? In this time of financial difficulty, in which many practices are in economic trouble and the excesses and window dressings of the wealthier past no longer can be comfortably funded, such costs would be ruinous. Many dentists will lose their jobs. Many practices will fold. The glove problem must be tackled sooner or later.
The problem with latex gloves is simple to solve. Dentists must pressure the CDC to declare that gloves are potentially hazardous and that its recommendations on mandatory UPs (including glove wear) are optional in those cases where UPs use is more detrimental than beneficial based on the dentist’s evaluation on a case-by-case basis. In this way, glove use will be determined by the doctor, not the bureaucrat. The blood-borne pathogen concerns of a medical heart surgeon need not be extrapolated to the dentist doing a prophy on a healthy 3-year-old. OSHA’s blood borne regulations already have this glove option, to a limited degree, in place (Federal Register 12-6-91. 56:235 p.64129d3ii). Once the CDC publicizes this change, dentists can once again take command of their practices. It’s your future and your patients’ health, and now is the time to act.
Dr. Ellis Neiburger is a general practitioner in Waukegan, Illinois. Contact him at 847-244-0292 or drneiburger.com.
References
- ^CDC. Guidelines for prevention of transmission of human immunodeficiency virus and hepatitis B virus to health-care and public-safety workers. MMWR. 1989 Jun 23;38(6):1-37.
- ^OSHA joint advisory notice: Protection against occupational exposure to HBV and HIV. October 19, 1987.
- ^Editorial: Practitioners surveyed report dramatic increase in glove usage. Dental Products Report. 1987;12:1.
- ^Holub W. et al. AIDS, A new disease? American Clinical Products Review. 1988;5:28-37.
- ^Fein S. A bad case of one upmanship. Dental Economics. 1988;5:23.
- ^Most dentists wear gloves, survey says. ADA News. 1989;20(3):1-2, 4.
- ^Coburn S. AIDS Update. Illinois Dental Journal. 1988;3:128-9.
- ^Solovan D, Uldricks J, Caccamo P, Beck F. Evaluation of oral procedures performed with gloves: a pilot study. Dental Hygiene. 1984;3:122-4.
- ^Reingold AL, Kane MA, Hightower AW. Failure of gloves and other protective devices to prevent transmission of hepatitis B virus to oral surgeons. JAMA. 1988 May 6;259(17):2558-60.
- ^Dentists guard patients, selves against HB virus. ADA News. 1989;20(3):3.
- ^Badner V, et al. Dentists and risk of HIV. N Engl J Med. 1988;319(2):113.
- ^CDC. HIV/AIDS Surveillance Report. 2007;19:20.
- ^CDC. Update: acquired immunodeficiency syndrome and human immunodeficiency virus infection among health-care workers. MMWR. 1988 Apr 22;37(15):229-34, 239.
- ^GAO, CDC’s Investigation of HIV Transmission by a Dentist. Sept. 1992. p.2-47.
- ^Klein RS, Phelan JA, Freeman K, et al. Low occupational risk of human immunodeficiency virus infection among dental professionals. N Engl J Med. 1988 Jan 14;318(2):86-90.
- ^Wormser GP, Rabkin CS, Joline C. Frequency of nosocomial transmission of HIV infection among heath care workers. New England Journal of Medicine. 1988 Aug 4;319(5):307-8.
- ^Neiburger EJ. Dentists do not get occupational AIDS. J Am Assoc Forensic Dentists. 2004;26:1-3. Available at: http://www.dentaleditors.org/Article%20Library/Neiburger%20 art1.htm.
- ^Neiburger EJ. Gloves and manual dexterity. J Am Assoc Forensic Dentists. 1990;13:1-4.
- ^Shapter D. AIDS, what dentists are doing about it. Dental Management. 1988;3:32-6.
- ^Bonner P. Report D.D.S. alert. 1987;7:19:2-3.
- ^Tanchyk AP. Precautions in protection. J Am Dent Assoc. 1987 Dec;115(6):824.
- ^Hardison JD, et al. Gloved and ungloved: performance time for two dental procedures. J Am Dent Assoc. 1988 May;116(6):691-4.
- ^Klein RC, Party E, Gershey EL. Safety in the laboratory. Nature. 1989 Sep 28;341(6240):288.
- ^Arnold SG, Whitman JE Jr, Fox CH, Cottier-Fox MH. Latex gloves not enough to exclude viruses. Nature. 1988 Sep 1;335(6185):19.
- ^Young F (FDA Commissioner) Report. Dental Economics. 1989;1:9.
- ^Editorial. AIDS found to pass through latex glove undetected. Dentistry Today. 1988;12:12.
- ^Katz JN, et al. Fluorescein dye evaluation of glove integrity. J Am Dent Assoc. 1989;118(3):327-31.
- ^Otis LL, Cottone JA. Prevalence of perforations in disposable latex gloves during routine dental treatment. J Am Dent Assoc. 1989 Mar;118(3):321-4.
- ^Tortora GJ, Funke BR, Case CL. Microbiology: an introduction. 3rd ed. New York: Benjamin/Cummings Publishing Co.; 1989. p. 327.
- ^Boguszewski D. Third national forum on AIDS and HBV. Dental Products Report. 1989;1:6.
- ^Baker RF, Sherwin RP, Bernstein GS, Nakamura RM, et al. Precautions when lighting strikes during the monsoon: the effect of ozone on condoms. JAMA. 1988 Sep 9;260(10):1404-5.
- ^Brough SJ, Hunt TM, Barrie WW. Surgical glove perforations. Br J Surg. 1988 Apr;75(4):317.
- ^Gonzalez E, Naleway C. Assessment of the effectiveness of glove use as a barrier technique in the dental operatory. J Am Dent Assoc. 1988 Sep;117(3):467-9.
- ^Hadler SC, Sorley DL, Acree KH. An outbreak of hepatitis B in a dental practice. Ann Intern Med. 1981 Aug;95(2):133-8.
- ^Neiburger EJ. Are we spreading AIDS by wearing gloves. New York State Dental Journal. 1988;3:6-7.
- ^Fisher A. Contact dermatitis. 3rd ed. Philadelphia: Lea & Febiger; 1986. p. 224-79 and 630-1.
- ^Reitz CD, Clark NP. The setting of vinyl polysiloxane and condensation silicon putties when mixed with gloved hands. J Am Dent Assoc. 1988 Mar;116(3):371-5.
- ^Antó JM, Sunyer J, Rodriguez-Roisin R, et al. Community outbreaks of asthma associated with inhalation of soybean dust. N Engl J Med. 1989 Apr 27;320(17):1097-102.
- ^van der Meeren HL. Life-threatening contact urticaria due to glove powder. Ned. Tijdschr Geneeskd. 1988 May 21;132(21):968-70.
- ^Slater JE. Rubber anaphylaxis. N Engl J Med. 1989 Apr 27;320(17):1126-30.
- ^Dooms-Goossens A. Contact urticaria caused by rubber gloves. J Am Acad Dermatol. 1988 Jun;18(6):1360-1.
- ^Yoder K. Patients’ attitudes toward the routine use of surgical gloves in a dental office. Journal of Indiana Dental Association. 1985;64(6):25-7.
- ^Brantley CF, et al. The effect of gloves on psychomotor skills acquisition among dental students. J Dent Educ. 1986 Oct;50(10):611-3.
- ^U.S. revenue forecast of the disposable gloves market. Dentist. 1989;4:9.
- ^Bender IB, Landau MA, Fonsecca S, Trowbridge HO. The optimum placement-site of the electrode in electric pulp testing of the 12 anterior teeth. J Am Dent Assoc. 1989 Mar;118(3):305-10.
- ^Christensen GJ. Operating gloves. The good and the bad. J Am Dent Assoc. 2001 Oct;132(10):1455-7.
- ^Assennato G, et al. Type I allergy to natural rubber latex and type IV allergy to rubber chemicals in health care workers with glove-related skin symptoms. Clin Exp Allergy. 2002 Mar;32(3):441-7.
Written by Ellis Neiburger, DDS, for Chairside® magazine. Copyright ©2010 Ellis Neiburger. All rights reserved.