Photo Essay: BruxZir® Solid Zirconia Anterior Esthetic Challenge

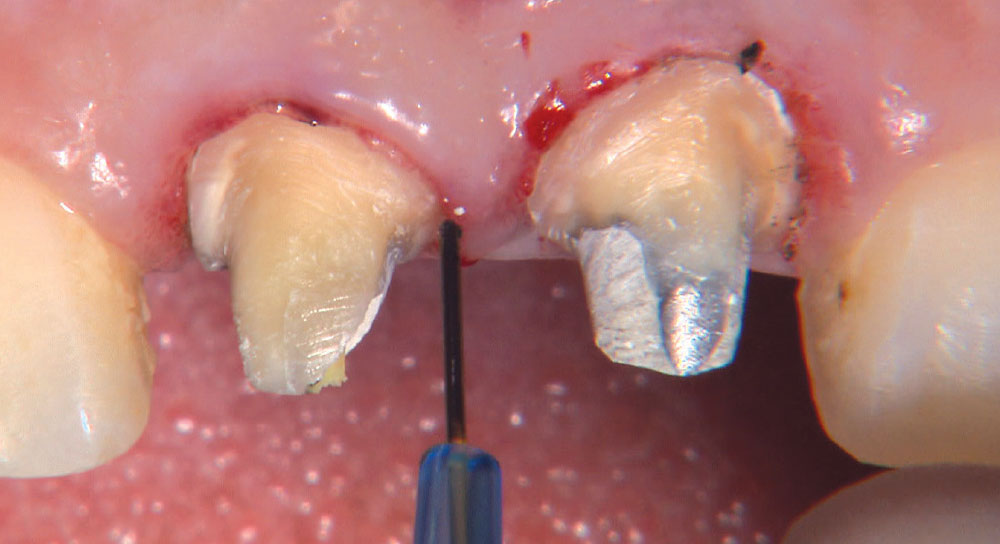
This photo essay illustrates our laboratory’s recent advancements in improving the esthetic properties of BruxZir® Solid Zirconia. Since the launch of the crown & bridge material in 2009, we have talked about BruxZir Solid Zirconia being “More Brawn Than Beauty.” As our R&D department refines our processes, improving the material’s translucency, the esthetics have continued to improve dramatically. What better esthetic challenge could there be for a material than using it to replace old crowns on teeth #8 and #9? BruxZir Solid Zirconia rises to the challenge in this case, but keep in mind, I have the advantage of in-house dental technicians, which always makes it easier to deliver great restorations. High-quality digital photographs can result in the same high-quality restorations almost as easily. After this case, we decided to upgrade the BruxZir Solid Zirconia motto to “More Brawn and Improving Beauty.” Continue reading to see if you agree!
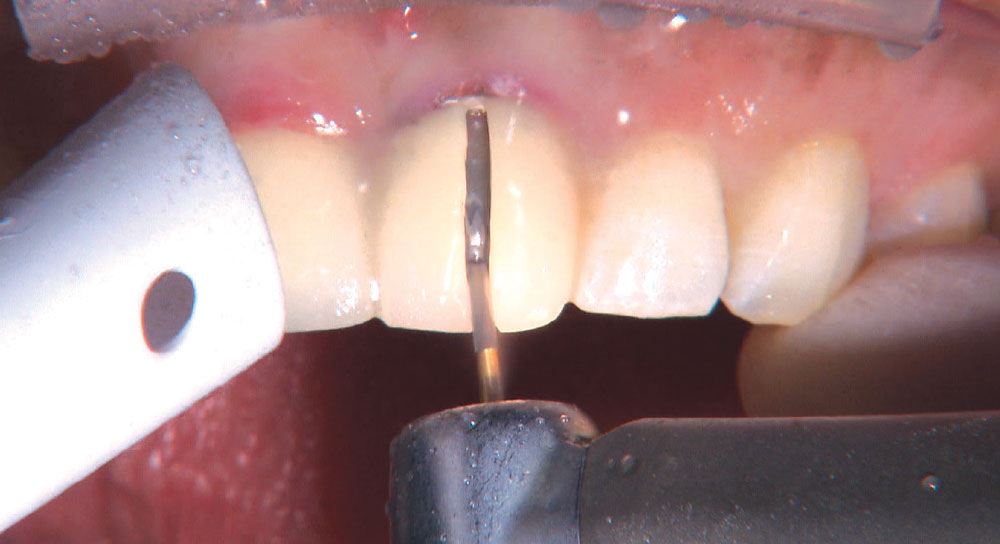
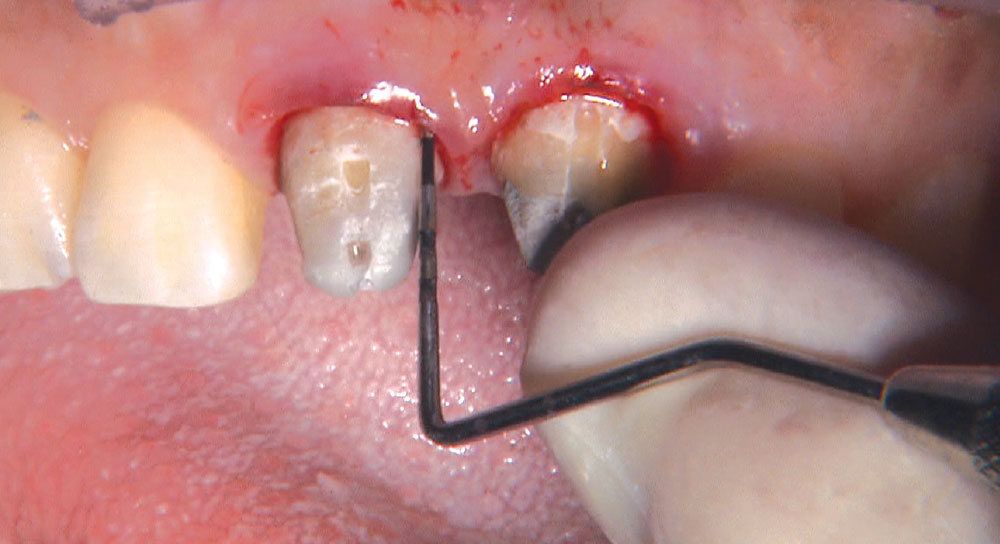
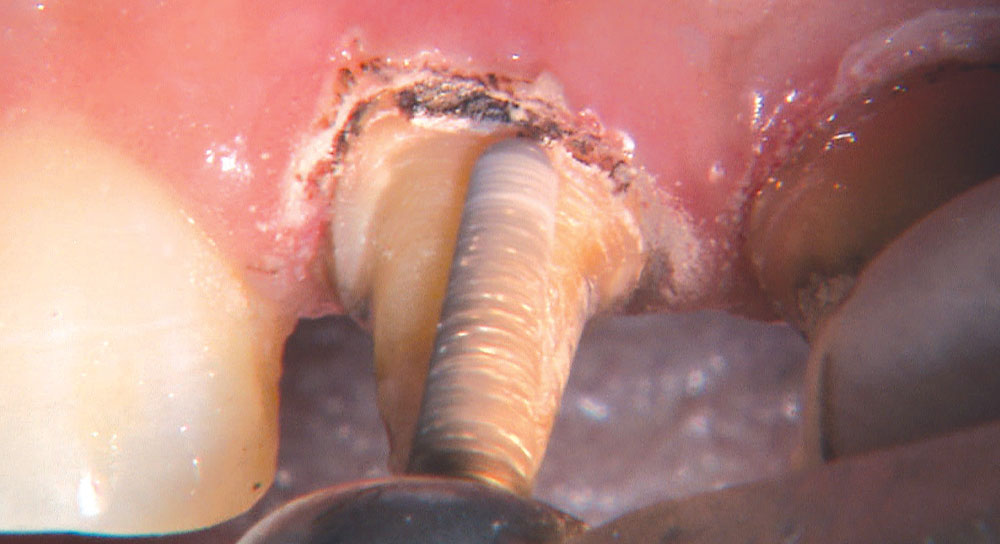
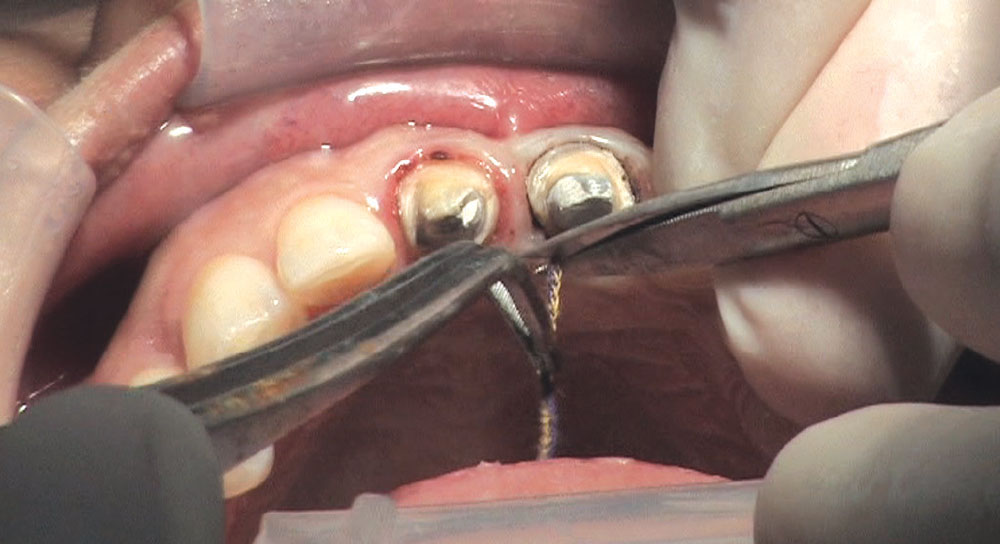
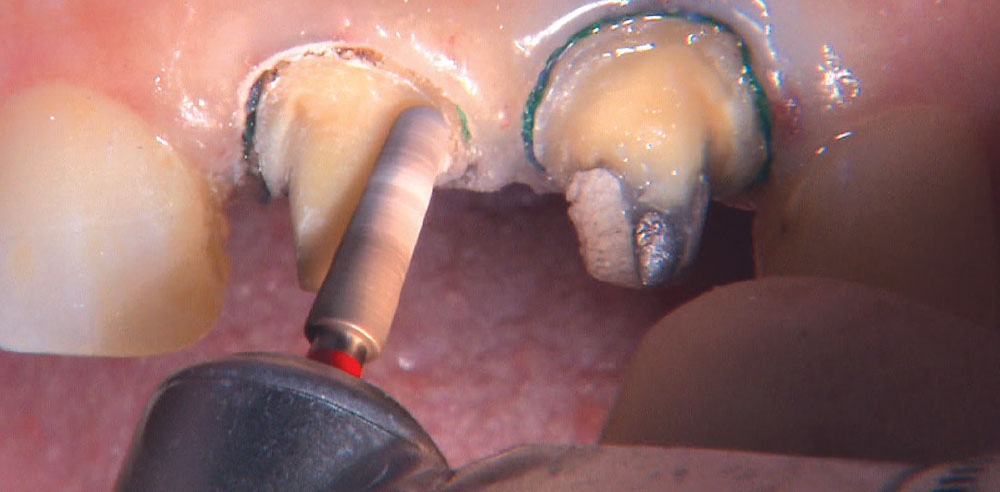
With the margins now clearly exposed, I use an 856-025 bur (Axis Dental) with the water off and my KaVo ELECTROtorque handpiece set to 4000 rpm to slowly drop the margins to the new gingival level.
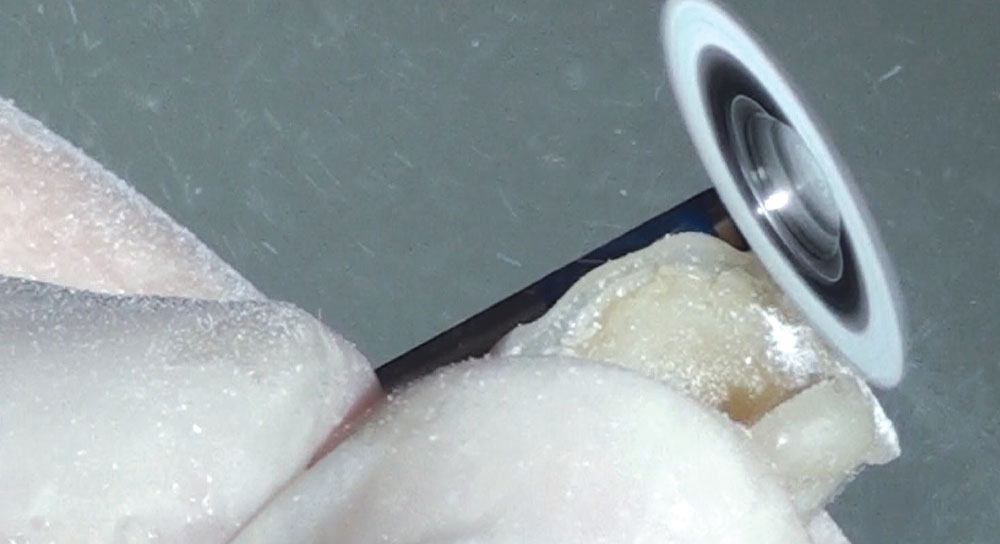
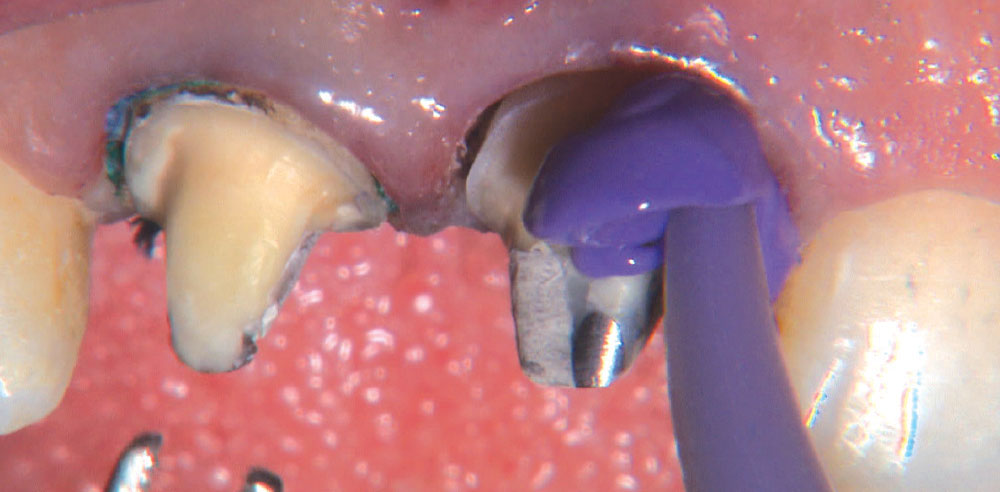
I use a Warm Air Tooth Dryer (A-dec; Newberg, Ore.) for 10 seconds after applying both coats of the G5. Meanwhile, my assistant places Z-PRIME™ Plus (Bisco; Schaumburg, Ill.) inside the BruxZir crowns, and then we air-thin that for 10 seconds. Z-PRIME Plus is a zirconia adhesive that helps strengthen the bond of the cement to the crown.
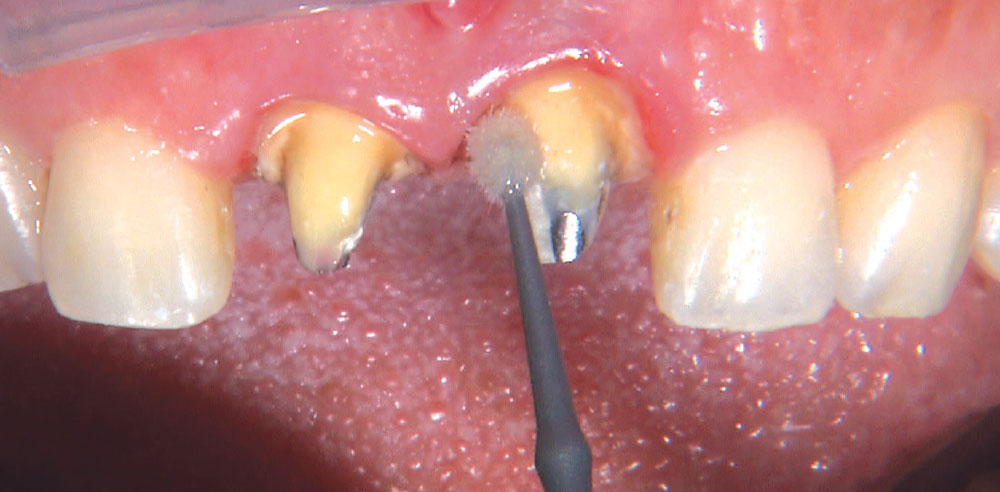
The other amazing thing I notice is the facial anatomy that you see on the crowns in the lateral views. That flat facial profile in three planes is what makes a tooth look real. Because that anatomy is built into the CAD/CAM database, we are able to deliver it every time — provided the doctor gives us enough reduction.