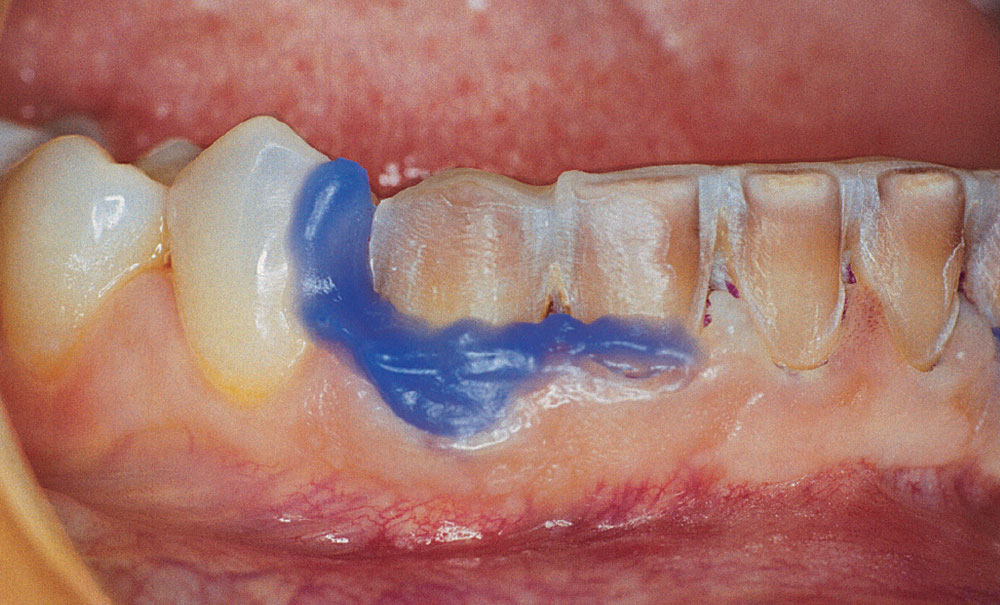
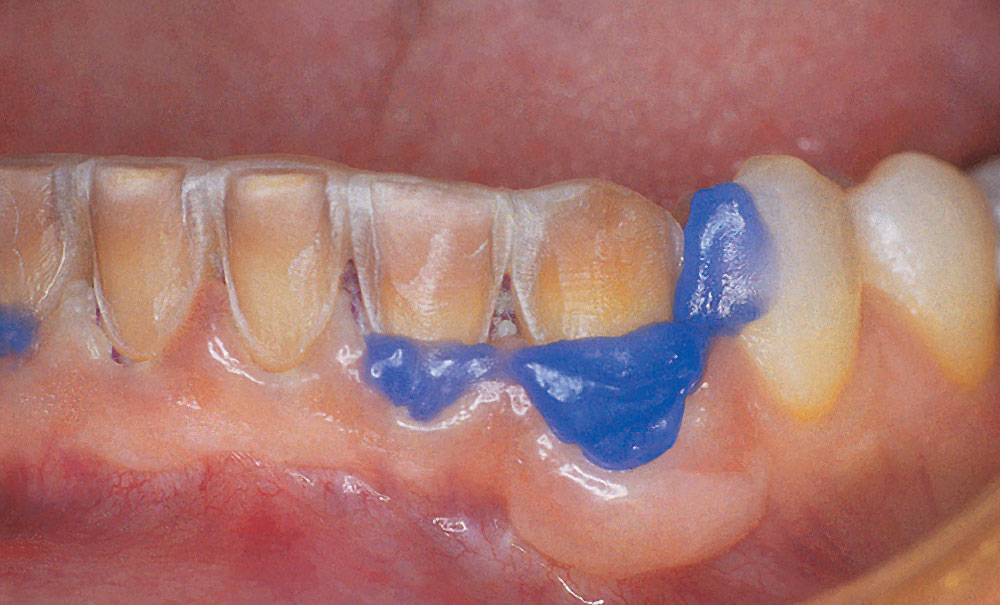
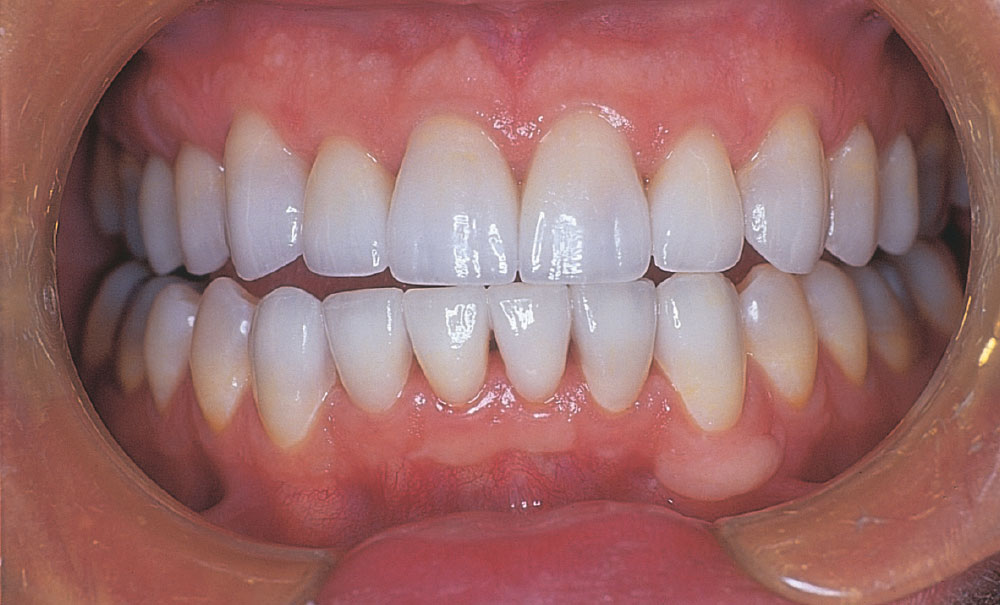
Photo Essay: Porcelain Veneers for Tetracycline Using Blockout Method

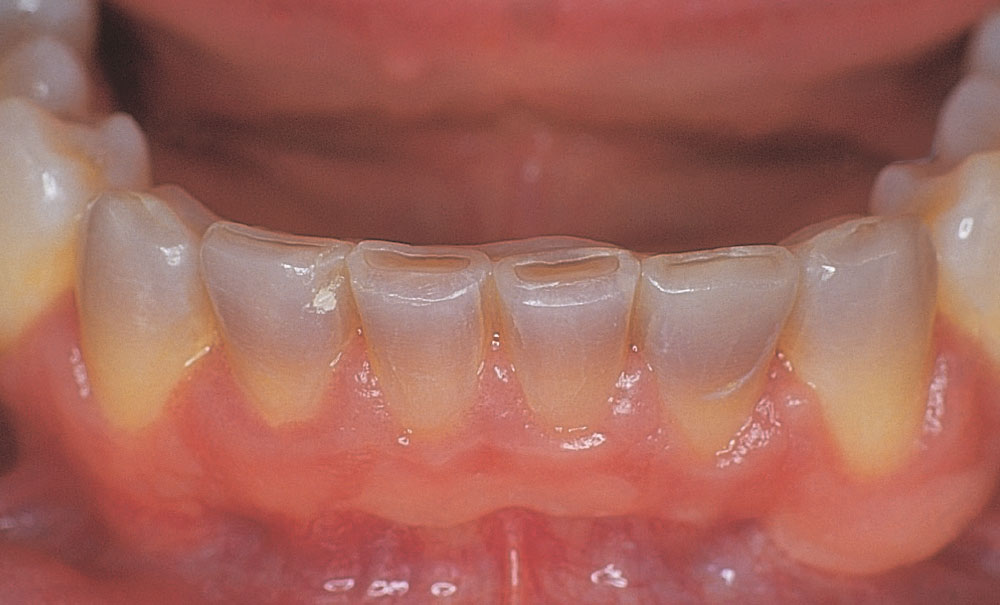
Note that the tetracycline stains are in the incisal half of each tooth, except for the central incisors, where the stains extend almost to the gingival crest. Masking stains in the more incisal portions of the teeth is much easier than when the stains are at the gingival margins. Because the stains are more incisal, the gingival color is quite normal.
Dr. Michael Miller is the co-founder, president and editor-in-chief of REALITY. He maintains a dental practice in Houston, Texas. Contact him at mm@realityesthetics.com.
Reprinted by permission of REALITY Publishing. REALITY: The Information Source for Esthetic Dentistry, The Techniques, Volume 1, 2003, REALITY Publishing Company, pp. 272–74.