One-on-One with Dr. Michael DiTolla: Interview of Dr. Dan Fischer

Dental innovator and Ultradent Products Inc. CEO Dr. Dan Fischer continues to ensure that his company’s products play a large role in the clinical techniques of many dentists. I like to check in with him once a year or so to find out what his company has been working on, and how his mission to stamp out dental caries is going. If you are ever in Utah, you owe it to yourself to visit Ultradent and take a look into the testing the company does to formulate its products. I guarantee you will come away impressed.
Dr. Michael DiTolla: I’ve always admired Ultradent and what you guys have done because you’ve brought a lot of common sense to dentistry. You’ve taken some product categories and dispensing systems that needed cleaning up and really made things easier for those of us out there practicing. One of your newer products that came across my desk the other day is UltraCem™ (Ultradent; South Jordan, Utah), your resin-reinforced glass ionomer (RRGI) cement. I’ve always felt like this was a product category that could use another product or two in it. It’s far from the sexiest product in dentistry, but it seemed like there were only two companies dominating the market. So not only did you come out with a traditional crown & bridge cement, but you put it into a dispensing system that is so novel, it could only be from Ultradent. Can you share a little bit about the development process?
Dr. Dan Fischer: Sure. Most of the credit on that syringe mixing device for the liquid and powder goes to our young team in R&D that picked up on the passion of the ease of use of a syringe. If you think about it, a syringe is one of the simplest hydraulic devices on the planet. But to be able to mix a liquid and a powder brings so much to the equation, on the logic that no paste-paste resin-modified glass ionomer (RMGI)* can be as strong as a pure liquid-powder — you just can’t get enough of the glass ionomer powder into a resin-based system.
MD: So when you guys started development of UltraCem, you already realized that, in order to have the best physical properties for this cement, you were essentially going to have to take a step back to a powder-liquid and move away from the paste-based systems?
DF: Yep. In fact, if you look at what was the strongest RMGI out there prior to UltraCem, it was GC’s FujiCEM™, and that is a liquid-powder mix in a capsule. And it’s the same with 3M™ ESPE™ RelyX™ Luting Cement; their strongest RMGI is still a liquid-powder mix in a capsule. As soon as you have to go to paste-paste, you lose the opportunity to get the amount of the glass ionomer silica in there that you’d like to have for creating a very strong cement.
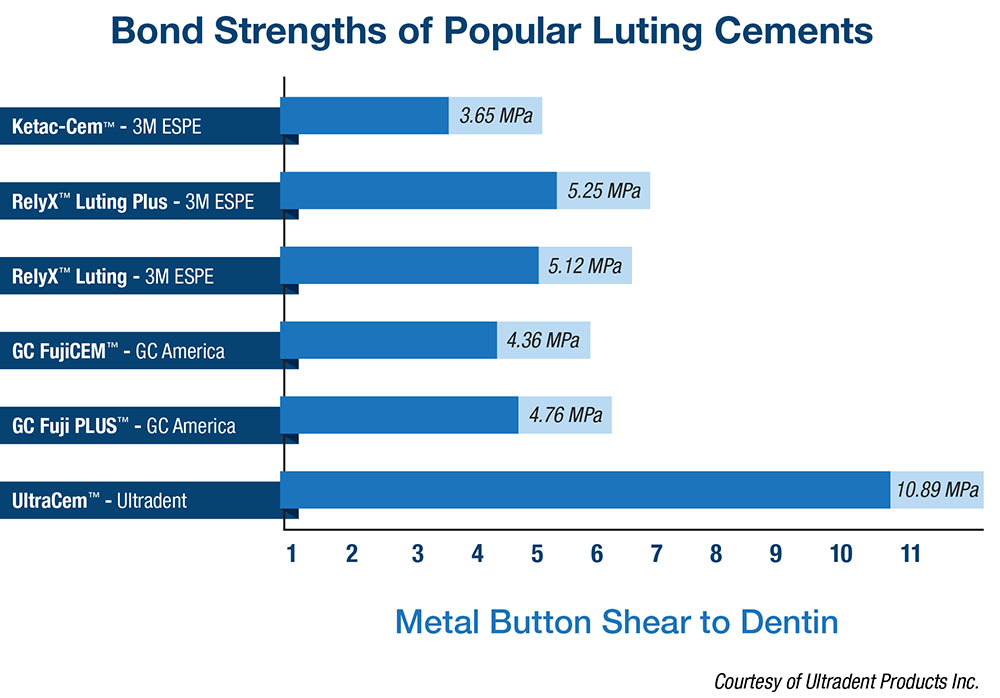
There was something else we realized, which we feel puts this product into its own distinctive category, Mike, and that is: RMGI is so fabulous for bonding to metal, and it is wonderful for bonding to zirconia, especially with the zirconia primer. But to really bond well to dentin and enamel, you need to have a minimal dwell time of the polyacrylic against the dentin to be able to etch it. That’s why UltraCem comes only in a regular set. If we were to bring it out in a fast set, it wouldn’t have that dwell time. But by having that dwell time, you have the first self-etching, resin-modified glass ionomer, which gives us a bond strength that more than doubles GC Fuji’s, which was the strongest heretofore (Fig. 1).
MD: You said a couple things there that I want to touch on. So the paste-paste delivery system, which has kind of become the norm — I think it’s probably the biggest seller in the category — it sounds like that was designed more for the dentist’s convenience than for the quality of the cement that comes from that mix. Is that right?
DF: Absolutely. It’s been the same name of the game for 90% of the bonding agents out there: they have been designed more for the dentist’s convenience. Tragically, in that process, we’ve had some great fourth- and fifth-generation bonding agents that have kind of been pushed aside, with the dentist running to the single bottles and the like, many of which, Mike, give one-fourth to one-half the bond strength of what a non-compromising adhesive can provide. So you take something like Clearfil™ SE (Kuraray America Inc.; New York, N.Y.) or OptiBond® (Kerr Corporation; Orange, Calif.) or our Peak® (Ultradent) — these are a handful of what I call “non-compromising adhesives” — and these can give an adhesion to dentin at around 65% to 75% of the actual strength of the dentin. Yet so many adhesives designed in the sense of speed can give you one-fourth to one-half that, and it’s really a lost opportunity. It prevents the dentist from being able to place larger, direct-bonded restorations.
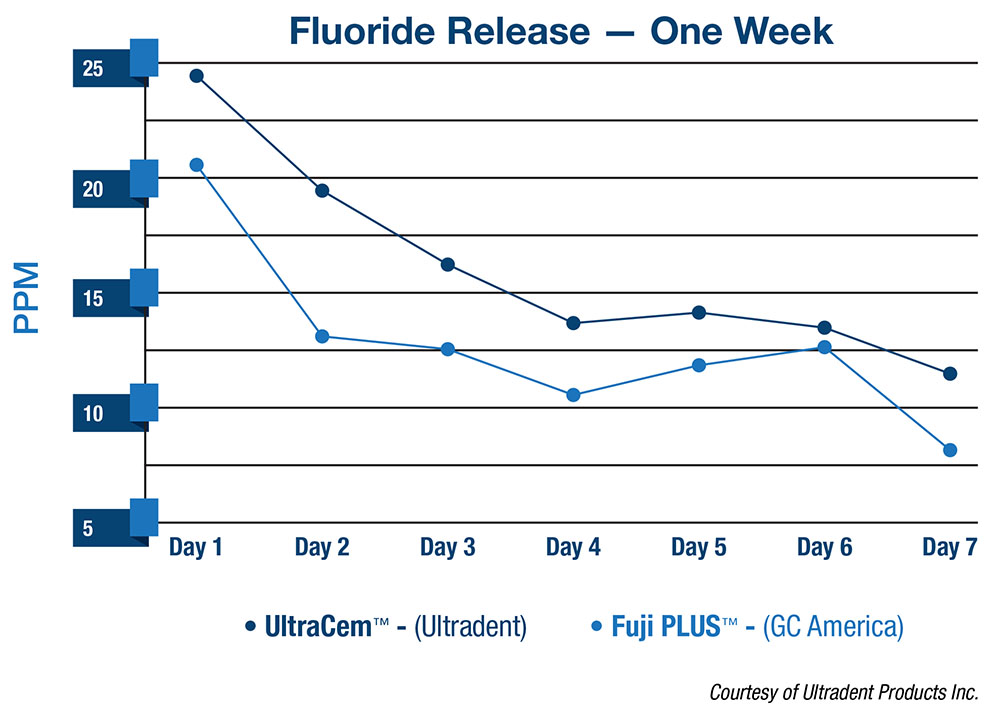
For the RMGI, it’s succumbed to the same gig: put it in a double-barrel type device and run it through a static mixer. When you’re doing that, you’re leaning more toward a resin cement with a minimal amount of resin-modified glass ionomer. Doing this was kind of a stepping stone to our resin cement. The best resin cement today can’t perform as well as UltraCem RRGI. Additionally, they don’t get the fluoride release like a RMGI can get (Fig. 2). So, all in all, to push the level of the RMGI to a higher level, you’re getting a great, strong cement to metal with the self-etching feature, over twice the bond strength to dentin as what you’d get with the best out there heretofore, and you’re getting the fluoride release. You also get a great film thickness that’s around 25 microns. So we’re kind of passionate about that. Furthermore, to eliminate the need for that plier that’s required to break the capsule before you can put it into the Wig-L-Bug® (Dentsply Rinn; Elgin, Ill.) to mix it, and to eliminate the Wig-L-Bug mixing and then to eliminate the little mix device, it brings about a lot of simplicity in our own office. Our guys have fallen in love with it because it’s so simplistic. Schools love it, too. You can probably remember when you had one Wig-L-Bug mixer between maybe 20 to 40 students, and you had to leave the patient and travel some distance to get your little capsule mixed, and then you headed back hoping you would be able to get everything in place before it set.
MD: Not only that, but I remember mixing about 10 crowns’ worth of cement for every actual dose of cement that I needed to cement one crown. So, I’m sure that for the schools it’s also going to eliminate a lot of waste, in addition to streamlining the cementation appointment. That really is amazing that you’ve been able to have UltraCem be self-etching and take advantage of those higher bond strengths, yet still have the fluoride release and not have to kowtow to going down the paste-paste route.
Now you mentioned the bonding agents. I think dentists are probably a little confused. I think sometimes they see products that appear too good to be true. One company releases a product like this and then the bigger companies, like the 3Ms, figure it’s selling so well that they need to release their own one-bottle system or their own paste-paste cement to keep up with the Joneses. I guess when the reputable companies release a product, the dentist tends to think: this product must be OK.
DF: Yeah, it’s frustrating. And with your dentist hat on, it’s doubly frustrating because it’s the patient that loses in the process. The patient is totally ignorant as to what’s going on. When you consider that there is somewhere around 100 brands of bonding agents out there now, and you’ve only got a small handful that are really non-compromising ones, that’s disconcerting.
Every time I’ve lectured over the last year, I share with dentists that there are two products that have a greater influence on the quality of your resin restorations than any other two products, simply based on what you choose to purchase. One of those is your bonding agent, and the second is your curing light. There are a number of quality composites out there, and there are a number of different matrix systems and the like, but, everything else being equal, the two factors that have the greatest impact on the quality of your restorations is the quality of your adhesive and the quality of your curing light. For posterior composites, you’ve got to have a curing light that will deliver around 15 to 16 joules entirely into the floor of your Class II box. You get on a first or second molar with one of these light guides that has the bend it in, and you just can’t direct that light directly down into those Class II boxes. So when I’m lecturing to dentists, I share with them that if you are using a compromising adhesive down on the gingival floor of that Class II box, or if you are using a light that just can’t illuminate the gingival floor of a Class II box, then, yes, there is a much higher potential for recurrent decay in the next two to three years under that area. It’s sad to say that our patients, when we notify them of such, just look up at us and say, “Well, doc, don’t worry, I just have soft teeth.” It just underscores the importance of us really thinking about the things we don’t think about more. If you envision a metal matrix wrapping a first or second molar, and you imagine a mesial-proximal box, with a light guide, the area that is behind that metal matrix down in the gingival box is in the shadows to a substantial degree. So, it’s a big deal to not only have adequate power, but to have a design that can illuminate the posterior preparations, or restorations, if you will. These light guides, they work fine for front teeth, but they sure are not predictable and appropriate for illuminating in proximal boxes on molars. You take those big light guides into a child’s mouth and it’s a joke!
MD: Right. There’s no chance of getting down there in those types of clinical situations. Do you think you face an uphill battle with this dispensing system? Just in the sense that dentists are used to and love the fact that you guys have put everything in a syringe over the years, but this is the first time that we’ve seen a permanent cement like this that needs to be mixed up in the syringe. Or do you feel like this is a product that once dentists get a chance to use it once or twice, they’re going to say it’s pretty simple to use and that they can sleep better at night knowing it’s a great cement with no compromises?
DF: The beauty of UltraCem is that the liquid and the powder are dosed in accurate ways, so you know you’re going to get a great mix. This is also the case for the capsule with the Wig-L-Bug; the syringe just eliminates the Wig-L-Bug and the other apparatus. But, certainly, if they don’t want to go that way, we offer it in a bottle and a scoop as well, because we believe in the cement standalone as a quality self-etching RMGI. But, ideally, they’ll pick up on the beauty of that syringe just like many other dentists. Many dentists have found the value of syringes and other dentists prefer just to bottle. You can’t convince all of them to go down the same path.
MD: That’s really interesting. I think 3M ESPE’s RelyX Luting Cement, which used to be Vitremer™ Luting Cement, has probably been the product category leader for a while. When it was a powder and liquid, I don’t think a lot of dentists had complaints about having to mix the cement and put it in the crown and cement it. I don’t think it was something that dentists looked at as being overly laborious or technical or a pain. So when it came out in the paste-paste form and it was from the same company, I think dentists just thought: all right, this is the upgrade. This must be version 3.0, instead of 2.0. This must be the better version of it. It’s really kind of stunning to hear you talk about the physical properties and how, clinically, in the patient’s best interest, it was kind of a step backward. I hope dentists read this and really stop to think a little more because I think sometimes marketing can lead us astray in the case of a product like this.
DF: We need marketing and marketing is important, but it’s the patient in the chair that it’s all about. We can’t afford to lose sight of that because they’re the ones who ultimately pay the price if things don’t work out, and they’re the ones who ultimately benefit if things do work out. From my point of view, this is just part of being a patient-centered dentist.
MD: I completely agree. And, obviously, as somebody who practices within a dental laboratory and talks to a lot of dentists who are cementing restorations, I’m very happy this is going to be in our magazine that goes out to 125,000 dentists across the U.S. But I’m especially happy this will go out to our customers, so they will get an opportunity to see what your research has proven.
Another thing that I’m passionate about is impressions. One of the trays I started using awhile back was the Triotray Pro™ from Triodent. They came to us as a laboratory and said they thought we’d like this tray and that our clients would be able to get better, less-distorted impressions with it. I started using it and I liked it, and we started promoting it to our customers who didn’t like the idea of a disposable tray. Then, I woke up one morning and saw that Ultradent was now distributing the tray! I thought: “Well, that’s great. Two companies that I really enjoy are getting along well together.” I’m interested in why, when you guys seem to develop a lot of things from scratch on your own and take a new approach to traditional products, you decided to join up with Triodent, rather than coming up with your own tray.
DF: There are a couple things that have been at work here — maybe more than two. Obviously, Triodent’s Dr. Simon McDonald and his R&D team have been hard at work down there in New Zealand pushing the envelope with their fabulous system. We’ve been working for years to push the envelope where we could. Both companies are driven by R&D. We’ve probably put more money into R&D for each dollar of product we sell than any other companies, and that’s where the first level of our similarity comes.
The next level of our similarity comes in that both of us are owned and managed by dentists, so we have that dentist’s need, that necessity-is-the-mother-of-convention drive to find a better way to skin the cat.
Then, it’s the words that frame the Ultradent brand as determined by a large, outside marketing entity that surveyed our customers about six years ago. The two words they found that were repeated most often by our customers were “progressive” and “trustworthy.” So when we looked at what the Triodent guys have done with this matrix — bringing the ultimate level of finesse, incorporating science and facilitating virtually 100% of the time tight contacts and nice, anatomically correct broad contacts for the direct-placed restoration — we thought, “Should we try and reinvent the wheel on this, or is it logical that we work together?”
Now I bring about the fourth leg of this discussion, and that is, we decided a couple years ago that even if we applied ourselves darn hard, it’s still not logical to think that we can invent everything that a dentist needs and have it be the absolute best product out there. We pride ourselves on having progressive, trustworthy products. We pride ourselves on bringing out what is among the best. But to do that on every front, to be the best at everything, that gets to be a challenge. And, if you’re not careful, it can even be a little bit arrogant. So when they approached us about distributing their matrix system, we studied it and thought: “You know, this company is aligning pretty good with our culture. They’re aligning well with our vision to improve oral health globally. They’re aligning on so many fronts, so let’s take the leap and for the first time market and sell another company’s brand of product.” We’re glad we did that, and I think they’re glad we did it. Certainly, our sales team focuses not on 20 or 30 different brands of thousands of different products like the large distributors do; they focus on a narrower range. We believe if we can keep that range narrow, even extending beyond our own brand if an appropriate opportunity presents itself, that we really can serve the dentist and their needs in much more knowledgeable, educated, quality, caring ways.
MD: I think you’re right. I think there is a lot of hubris if you start to go down the road of, “We can do everything better than everybody else.” I think, at some point, you do need to realize that there are a lot of smart people in this industry, and at least this one team has spent all their time looking at this one thing. When you sit and look at that impression tray, there are so many desirable aspects about it: how it’s taller in the anterior to help you get the impression of the cuspid, and the way the material locks into it, and how it has the little seal on the back to keep the extra impression material from running out the posterior part of the tray. It’s very stiff; it’s hard to squeeze it laterally and have it bend at all. So, it really is well thought out.
When you look at our laboratory statistics, 75% of the impressions we get here are for single-unit crowns, but almost 75% of those are still in plastic disposable impression trays. When you take these disposable trays and you squeeze them, they distort very easily. We know polyvinyl siloxane materials already shrink on their own as they cure. Frankly, it’s amazing that crowns fit as often as they do. Have you done any research into disposable impression trays? Or do you just kind of have a feel for how much better these Triotrays work?
DF: We basically believe the same concepts you do. In fact, my initial passion out of dental school in Loma Linda in the mid-’70s was full-mouth reconstruction. I ate, drank and slept that type of dentistry for some time. What you said is so true: The research that extends for decades shows the importance of a tray that’s not deformed, that’s rigid, that holds its shape and supports that impression material to the best of its ability. And, certainly, when you compound that with moldable units beyond one unit — boy! With just a tiny bit of inaccuracy extended out over the length of a multi-unit bridge, that problem escalates virtually algorithmically. So, it just made a whole lot of sense to embrace a quality impression tray such as what Simon and his team had developed. And I concur with you, when you look at the finesse, when you look at the details that you described — higher in the front for cuspids and the like — you can tell that a lot of thought has gone into it from entities who are knowledgeable on dental anatomy and dentists’ needs and patients’ capabilities in the chair and the rest. It all comes together.
MD: Even the disposable mesh that goes in the tray, when I first looked at it I thought there was a mistake in the factory because the mesh was so loose in the front. But, of course, it was intentional so that a patient with a deep overbite could get into maximum intercuspation without tearing the mesh. So even that little mesh insert has had a lot of thought that’s gone into it. It’s like you locked seven people in a room and gave them some quadrant impression trays and told them they could come out in a year. It looks like that’s the kind of time that was spent, and it’s pretty ingenious.
I heard you say something that I didn’t know about you. You started off early in your career doing a lot of full-mouth reconstruction? I’m surprised because I know you hate crowns now. (laughs)
DF: Quite frankly, Mike, I don’t hate crowns. In fact, just this morning I prepared a crown on a patient. What I say is: I place fewer crowns than I used to in my younger years. I don’t plead with my colleagues not to place crowns anymore, but rather to try and push that more invasive procedure back in a patient’s life. Not committing them to the invasive procedure of a full-crown prep in their 20s, 30s and 40s, but to try and buy time with less-invasive procedures — giving the pulp chamber a chance to become smaller, giving the dentinal tubules a chance to become smaller, and saving that more invasive procedure for their later years. When you do so, you minimize the number of root canal treatments that are required later, you minimize the amount of replacements that have to occur with crowns and the like. We will always, within my lifetime, I believe, have the need for full-coverage crowns. I’ve got one that my daughter put in my mouth just four years ago. It was an upper second molar that was a virgin tooth, but it succumbed finally to the “dental student syndrome.” Namely, when I was a junior, a senior student had to take out impacted wisdom teeth in order to graduate, and I became the volunteer. The student wasn’t the sharpest knife in the drawer and took out some of the buccal plate over my second molar, and I’m sure he leaned that elevator on that root. Later, bacteria got in that crack and it was discovered, much later, probably about eight years ago, when the tooth abscessed and became a sinus infection and all the rest. If you’ve got a tooth like that, or you’ve got a molar that’s taking a heavy load, or a tooth that’s had root canal treatment — you’ve got to put crowns on those kinds of things.
MD: Of course! And I know you don’t hate crowns. I know that what you don’t like is the overuse of full crowns as the easy way out, or kowtowing to what the patient’s insurance might pay. Did you go with cast gold on that crown?
DF: It’s solid cast gold on this upper second molar.
MD: Good choice! We like to see that. That’s becoming an endangered species in the laboratory today. I guess part of that is gold hitting $1,700 an ounce. It’s also patients giving some pushback about having gold in their mouth — even on a second molar — which is kind of crazy, especially after we tell them it’s the best material we’ve ever had in dentistry.
DF: Well, when you said, “Good choice, that’s what we like to see,” the truth is at the end of the day, you can’t even see it, Mike! (I’m teasing you a little based on the meaning here.) But, yes, it’s true: if nobody is going to see it, you can’t beat it. That being said, I am impressed with how zirconia continues to improve. In fact, boy, with the cost of metals and the like, thank goodness we’ve got materials like zirconia that are evolving to where they are.
MD: Right. Let me share some numbers with you. In 2007, 66% of the crowns that we fabricated here were PFM crowns and 23% were all-ceramic crowns. If you look at 2011 and the first half of 2012, PFMs have gone from 66% to 20%, and all-ceramics have risen from 22% to 68% of the restorations, and it’s because of zirconia and lithium disilicate. It’s shocking to me, and even to us as a laboratory, to see how quickly dentists have changed their allegiance and have been willing to kind of drop the PFM. It has been an amazing transformation largely pushed on by zirconia and dentists being somewhat satisfied with the material because they continue to order it.
Let me ask you about one other thing I find fascinating about you: your drive to find a cure for dental caries. I don’t think there could be a higher mission on the planet, and least in the dental world, than to tackle something like this, and I don’t hear anybody else really talking about this. In fact, I saw in a recent article that the city of Phoenix is thinking about not fluoridating their public water supply. Can you tell me how your drive to find a cure for dental caries is going?
DF: The progress has been slow. Not because of the technology, but because of regulatory constraints that we’re up against with the FDA. We have a technology that we feel can go a significant distance on this. We’re being very active on it, and we feel like we’re making some good inroads relative to explaining the technology to the FDA. It’s a little device that in the first human studies — four kids in a lower social economic group for which oral hygiene is pretty low — was shown to decrease caries 76%. If we can reduce caries 76%, we can reduce the incidence of the abscessed tooth 95%, which is exciting to me. But, yes, we’re still battling that.
That being said, and I don’t know if I told you this last time or not, Mike, but if we could bring about a cure to caries today, we’d still need more dentists. I mean, when you consider that in our country before the recession, one-third of our fellow Americans couldn’t afford to go to the dentist except for emergency treatment. When you consider that teeth are like tires — they’re good for so many miles, and then the treads wear out, the sidewalls give out. When you consider the jobs of the Western world, there’s hardly one job I can think of in Western countries that makes it easy for a patient with a missing central or dark, disfigured teeth to get a job. It’s a different world than it used to be. If we can bring about a cure for caries today, we’d still need more dentists.
The most exciting news to me would be the amount of suffering we could stop for those who can’t afford Western dentists. Whereas one-third of our fellow Americans can’t afford treatment, two-thirds of the world doesn’t even have access to dentists. You’ve got humans who would jump off a cliff to escape the pain of an abscessed tooth. You’ve got humans who are known to pick up a boulder and mash it into the side of their head trying to escape the pain of an abscessed tooth. In so many parts of the world, including America, there are 12-, 13-, 14-year-old kids who are totally edentulous! The magnitude of this infectious disease is so devastating, when humans don’t have access to or can’t afford access to our Western-trained dentists. I believe it’s something we have to be serious about, just out of humanitarian reasons beyond mastication, chewing and the like.
MD: I thought it was kind of self-evident that we’d still need dentists, even if we found a cure for caries. Can you clarify what you mean by that?
DF: What I meant to say is, for sure we’ll need dentists. But I believe, even if we bring about a cure for caries, we’ll need more dentists.
MD: Right. But are you saying there’s some pushback from the dental industry when you talk about curing dental caries?
DF: I say that, quite frankly, just to let the dental industry know it shouldn’t be afraid of any source that is going to bring about a cure to caries because, whether it be us, whether it be NIH, whether it be JNJ, whether it be any company that comes out with a cure for caries, we’ll still need more dentists. So in a proactive way I’m saying: dentists shouldn’t be afraid of that, dental companies shouldn’t be afraid of that. Teeth being like tires, look at the challenges to the dentition with people living longer and keeping their teeth longer. We’d have a shifting demographic. We’d have less need to be addressing severe, early childhood caries. We would be working more on older people. But that would be a good problem, Mike.
MD: I actually think that sounds like a great practice! In fact, most of the dentists I know who work on adult populations refer the kids out anyway. They don’t enjoy treating childhood caries. They prefer doing restorative dentistry on older patients. For dentists who say they want to do more esthetic dentistry, if you get rid of caries, a large part of it will be esthetic dentistry. So that sounds like a very modern, desirable way to practice. I like your vision of the future.
DF: And if more families, even in lower socioeconomic groups, didn’t have to spend as much money addressing caries, they could potentially have more there, including the insurance companies they align with to help them get orthodontics for their kids. So you’d have more pediatric dentists doing more orthodontics, taking more ortho courses. There’s always going to be the need for it all, we just will be shifting to somewhat different demographics. But we’ll still need more dentists, Mike.
MD: I think that’s such a noble effort that you’re putting forth toward doing that, especially for somebody from a restorative company — although, as you point out, it’s really not going to put anybody in dentistry out of business. Business will boom. It will just be a slightly different treatment modality than we practice today.
It’s been fascinating hearing about UltraCem, especially because when I first looked at the product, honestly, without a bunch of the literature, I just thought that you had reinvented the dispensing system. But I really appreciate you informing me on the difference between the powder-liquid and the paste-paste cement. It’s nice to hear that you guys decided to go with the product that was the best clinical product available and not just chase the easier money and high convenience. You chose something that’s going to stand the test of time and ultimately benefit the patient.
DF: That’s right. I think it’s important that the dentist sees it’s not just a fancy, fun mixer, but that it’s actually a superior cement.
One other quick note on this: You know how frustrating it is if, say, there’s not adequate retention on a preparation and the crown comes off, but I’m sure you also know the most challenging of all cases when that occurs is when you have compromised retention on one abutment and good retention on the other and one side of the bridge comes loose. For dentists who are cementing crowns in which they have less-than-ideal vertical wall retention capabilities or any concern over one side of a bridge coming off, they can take that bond strength — which is a little more than double GC Fuji’s — and double it again simply by putting a little of our Peak on the preparation before they cement.
MD: Interesting. That’s certainly an easy way to double the bond strength. And with the UltraCem, they get all the fluoride release as well, so they don’t have to make that compromise.
DF: Yes, you are still getting the fluoride release, and you go from twice the bond strength of a GC Fuji to four times the bond strength. And the GC Fuji and UltraCem are higher in bond strength than the self-etching resin cements that are out there today.
*RRGI and RMGI are used interchangeably in this interview.
For more information on Ultradent, visit ultradent.com or call 888-230-1420.