Photo Essay: The Pursuit of BruxZir® Anterior Esthetics

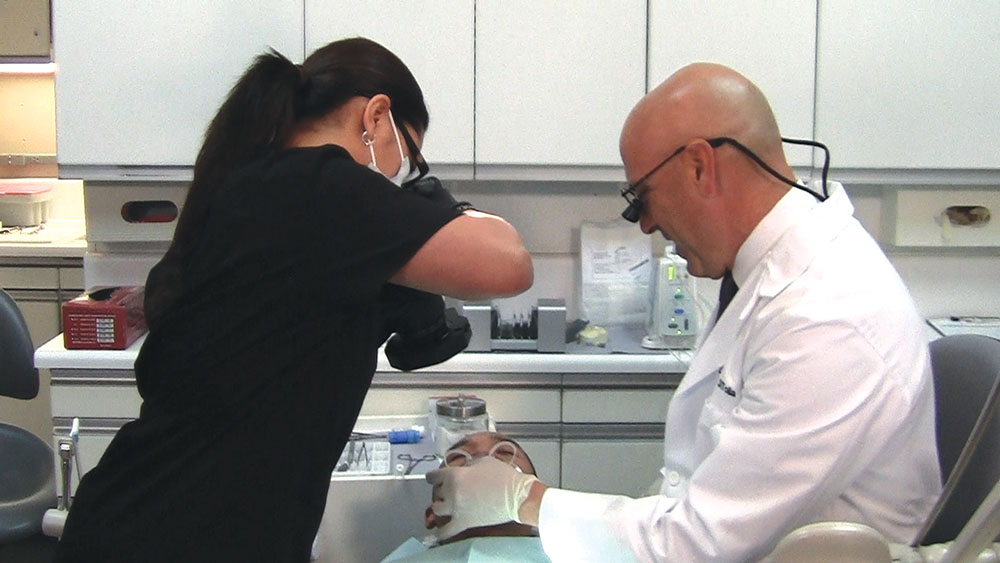
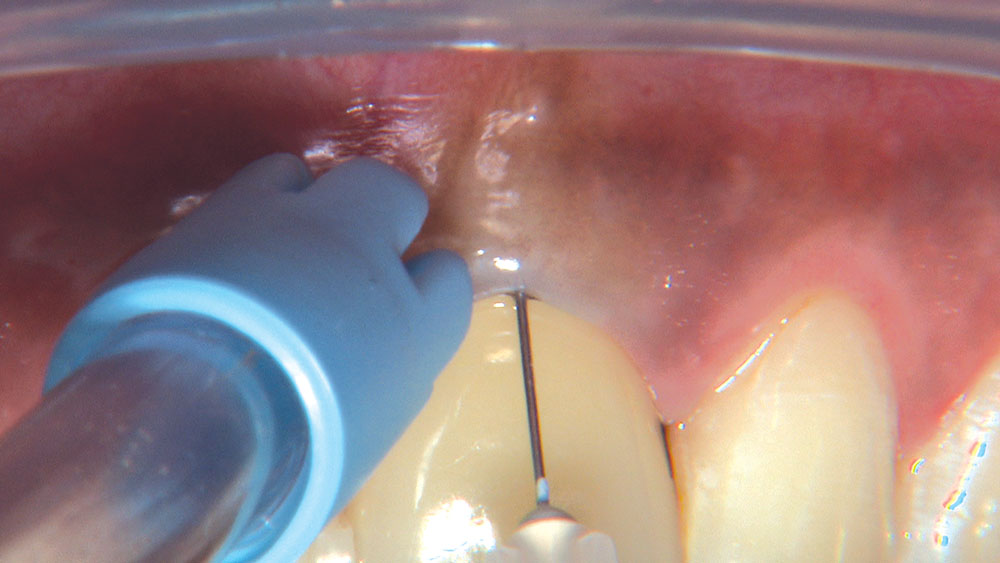
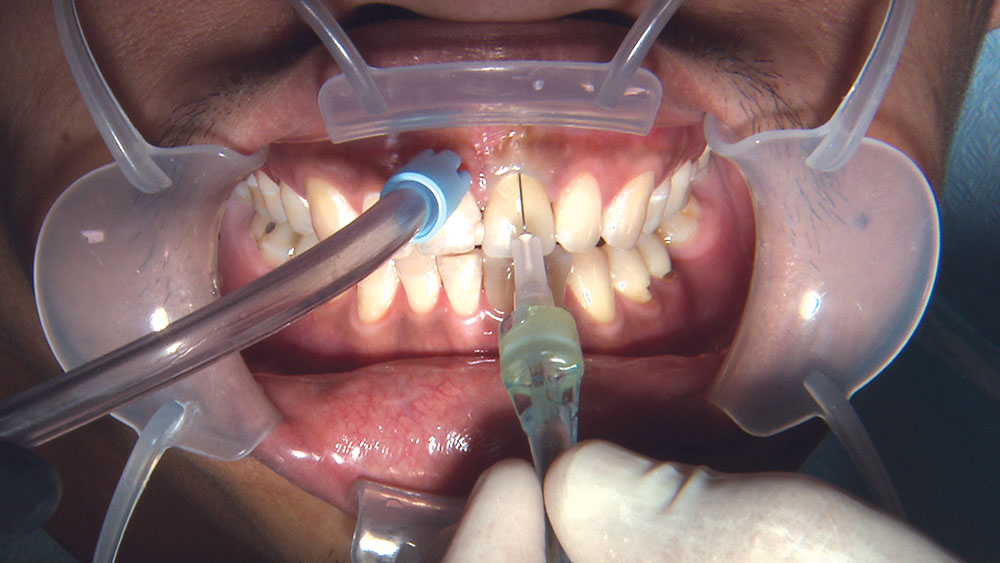
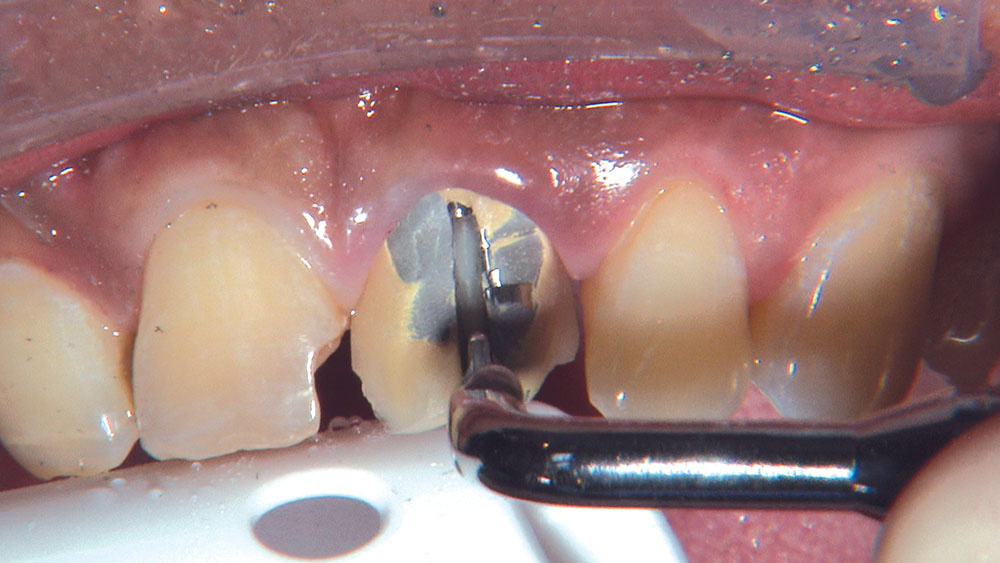
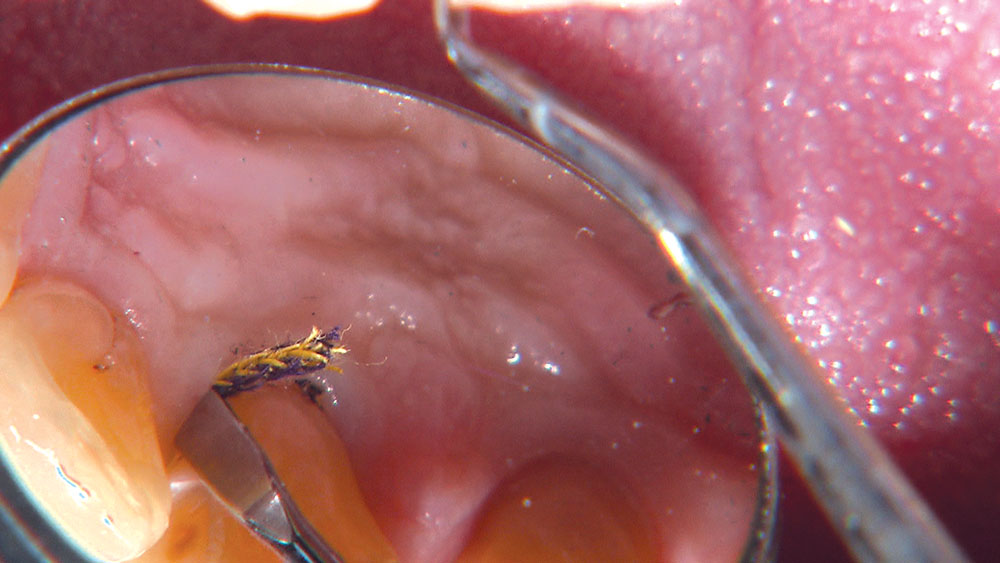
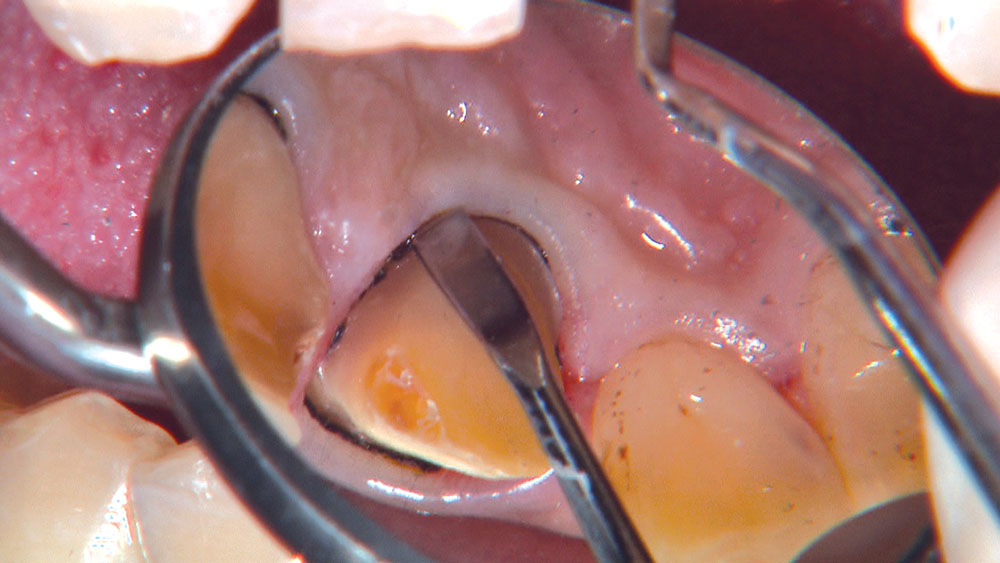
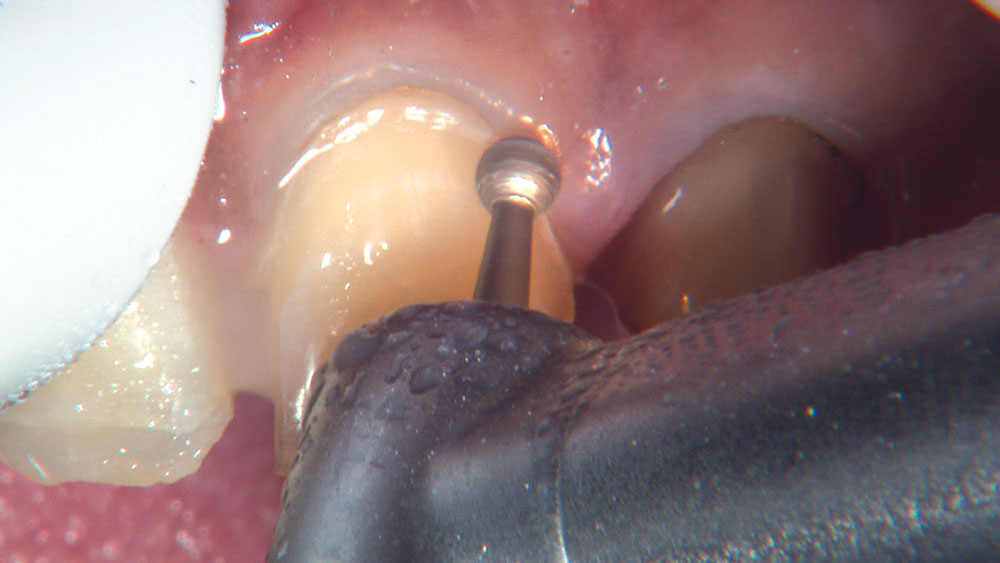
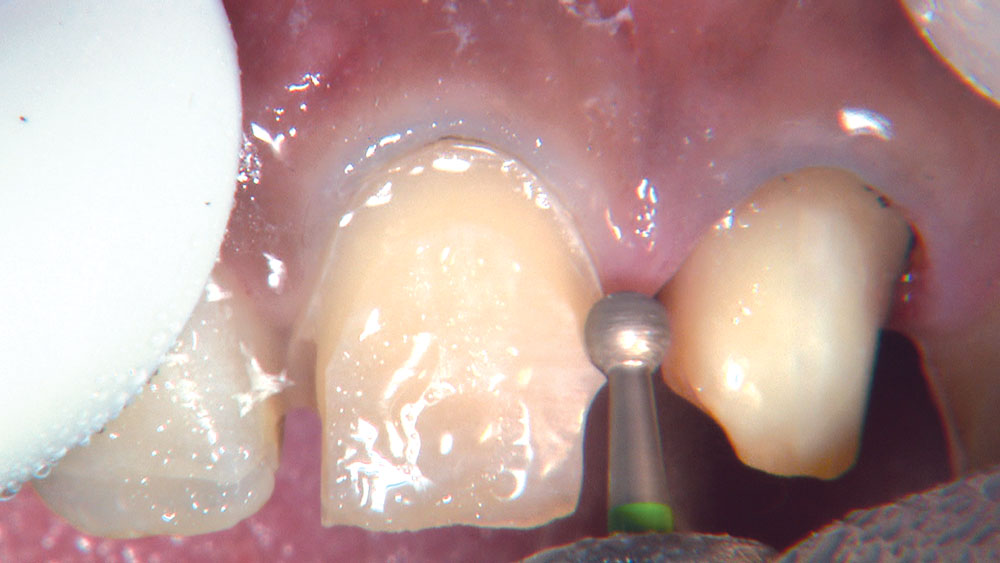
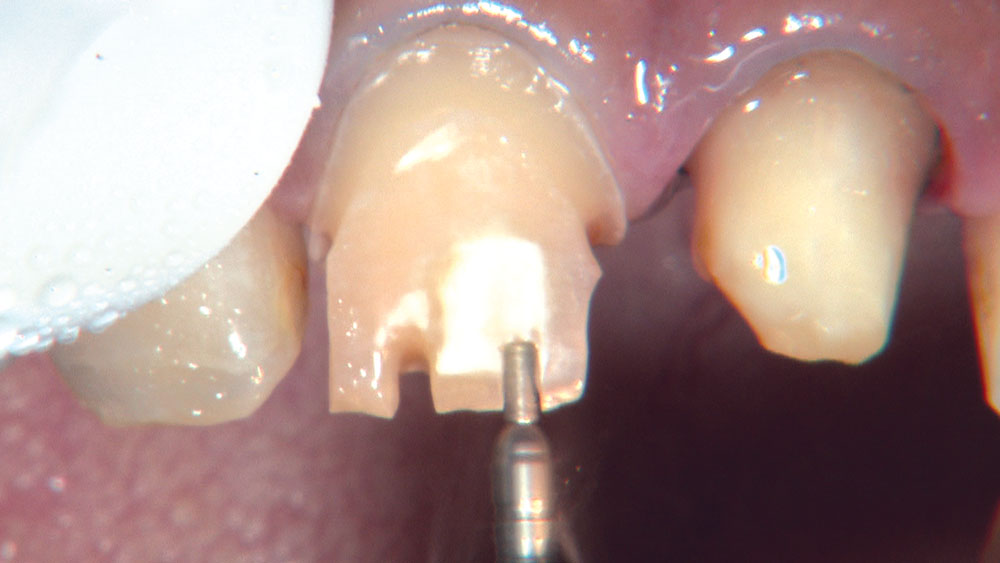
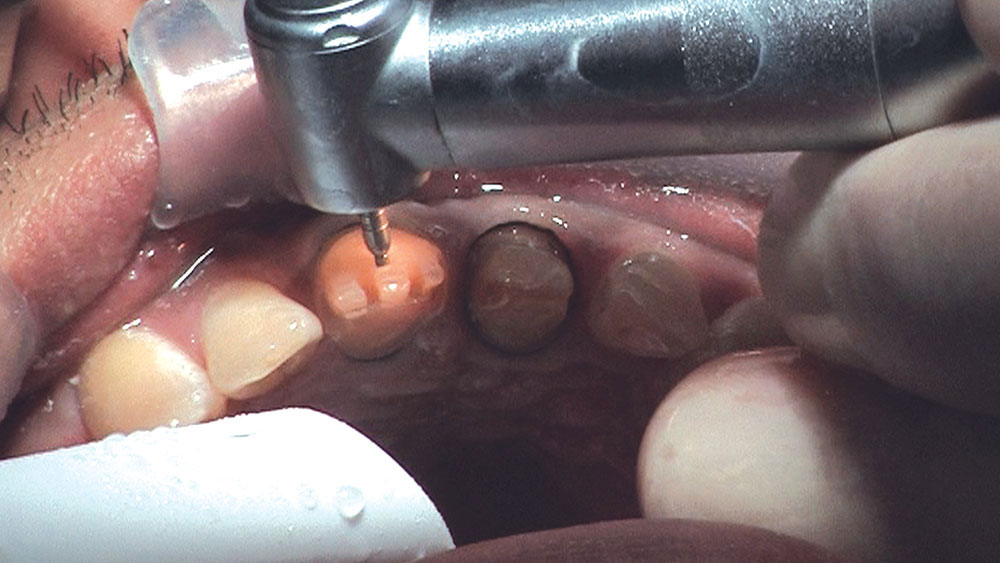
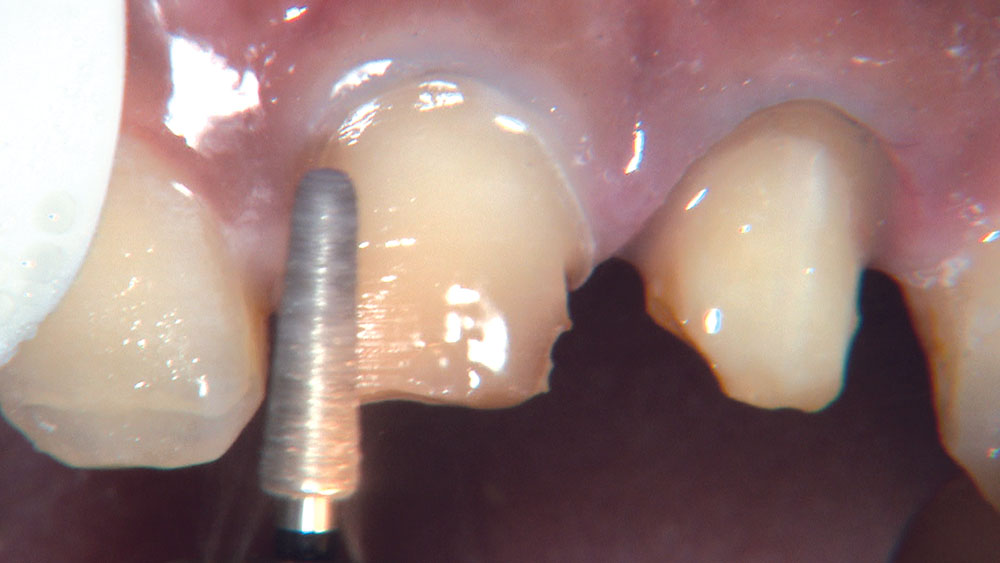
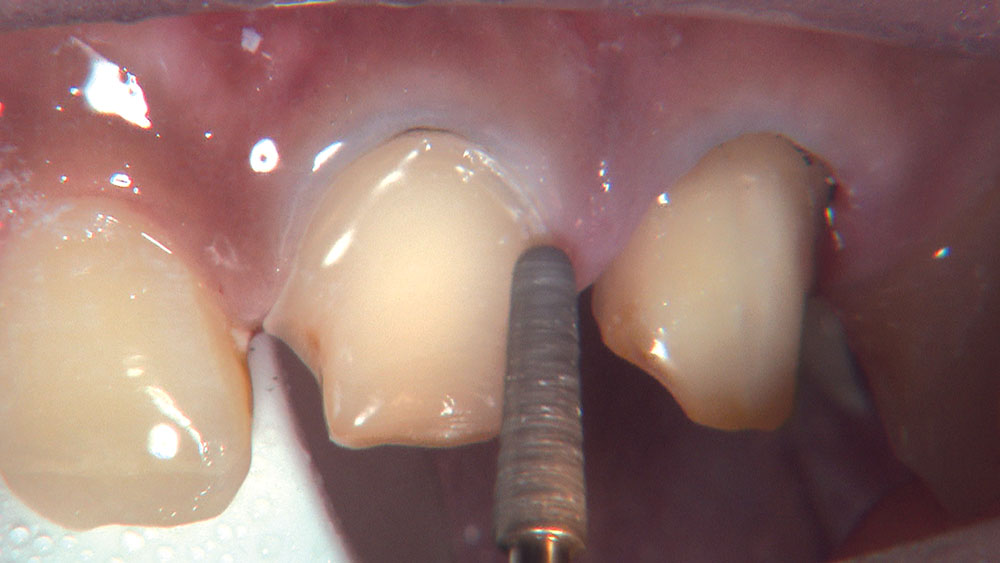
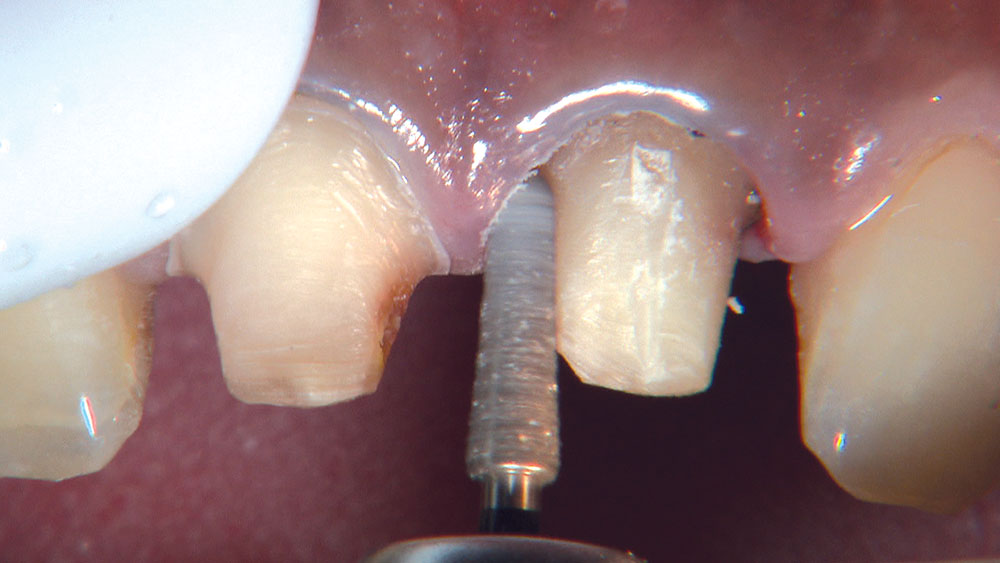
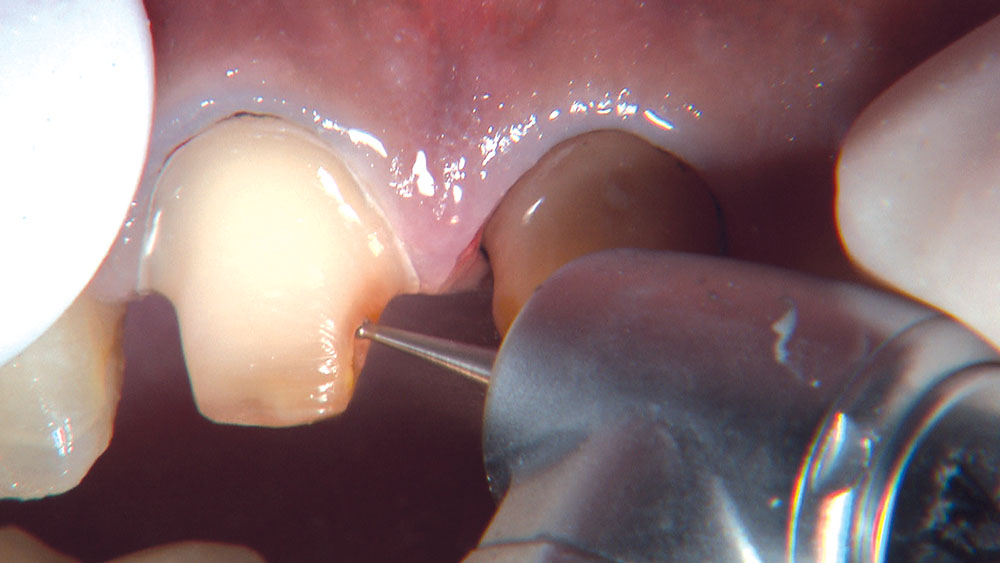
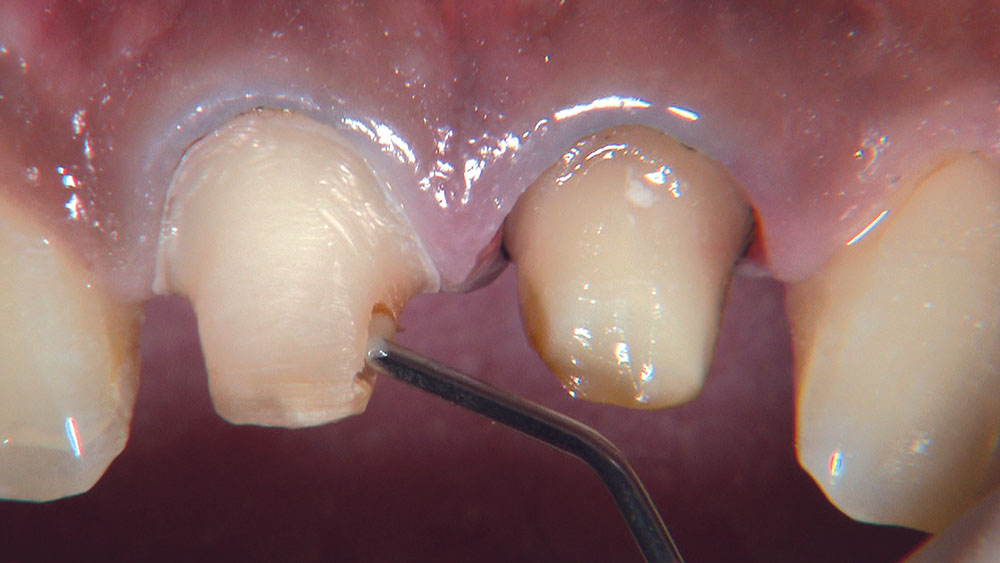
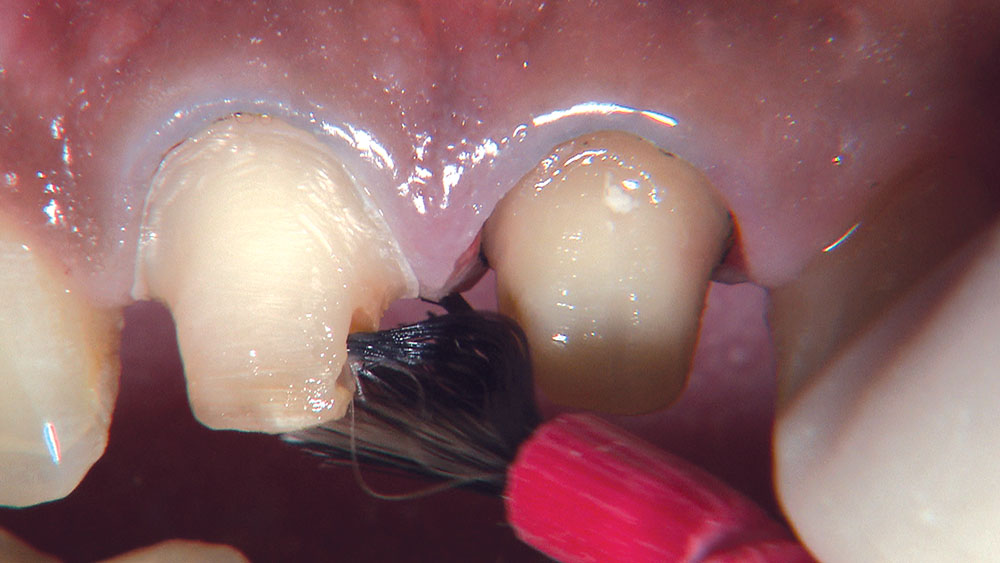
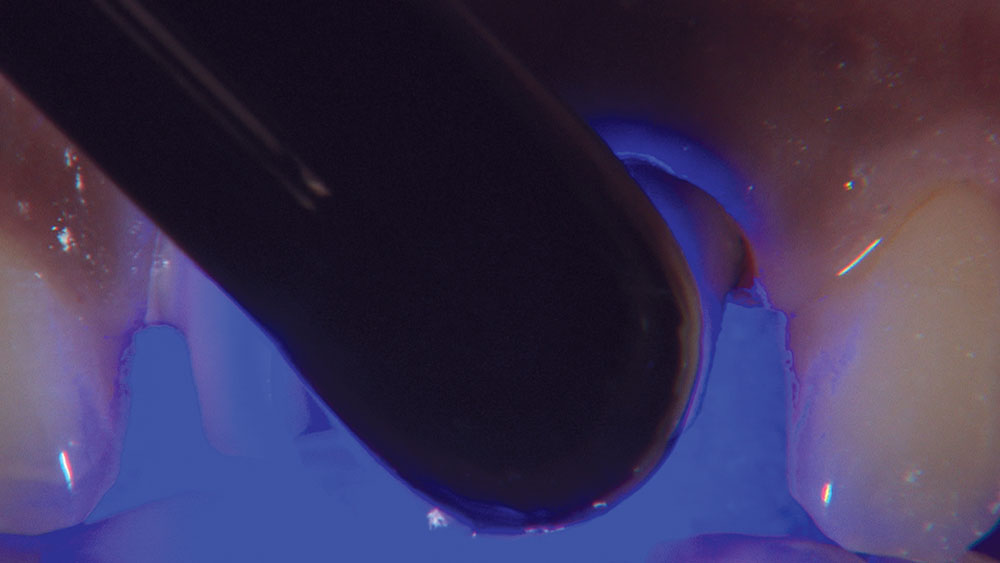
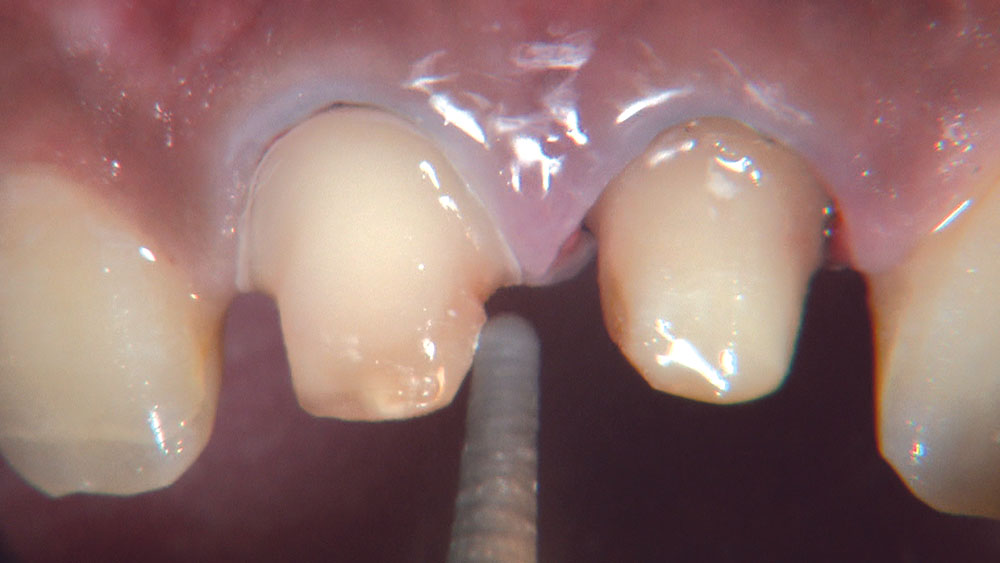
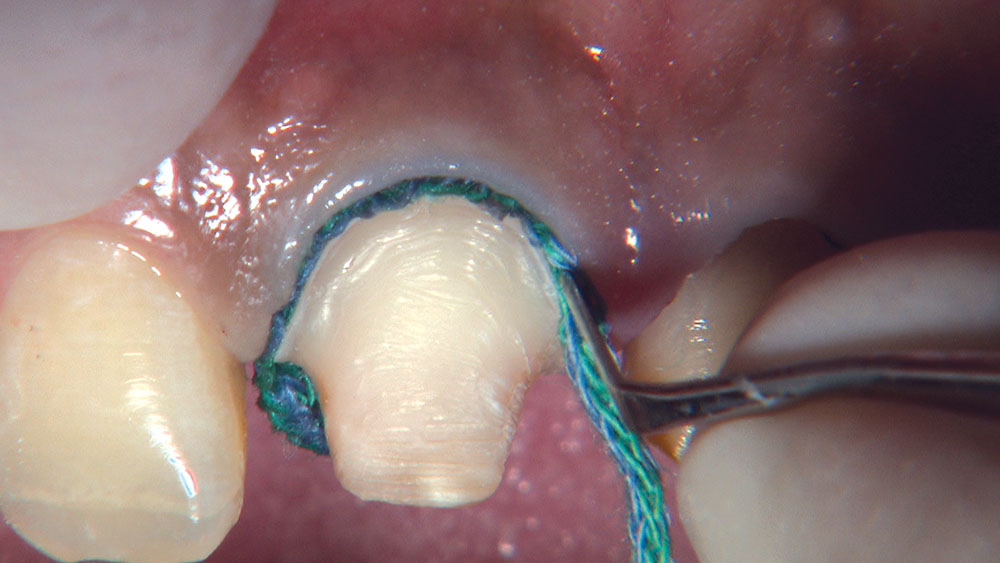
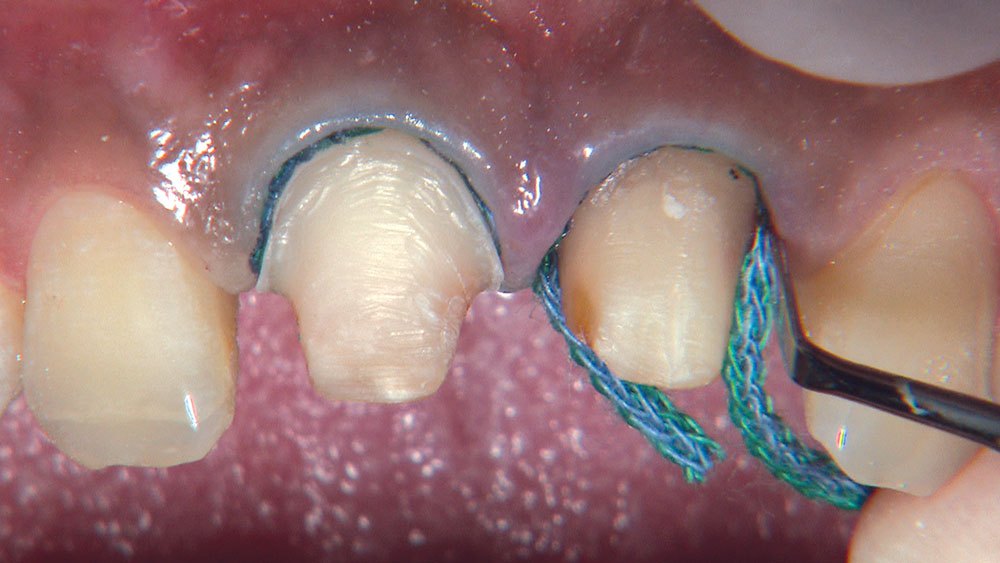
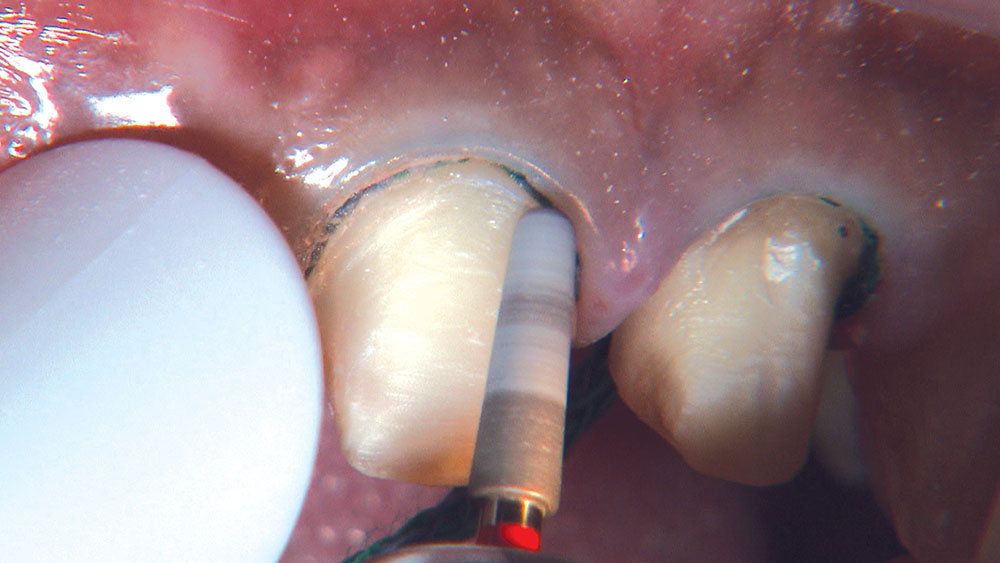
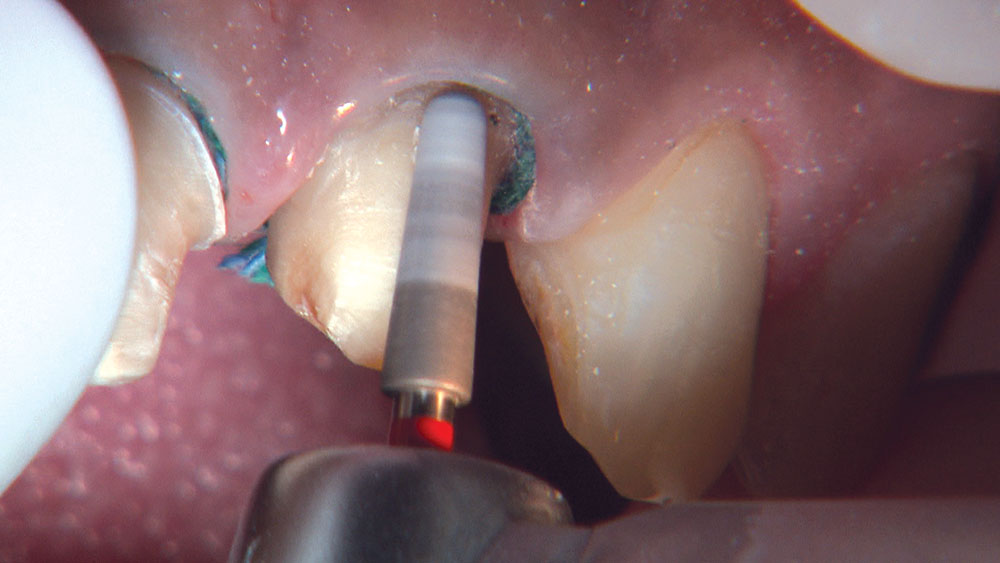
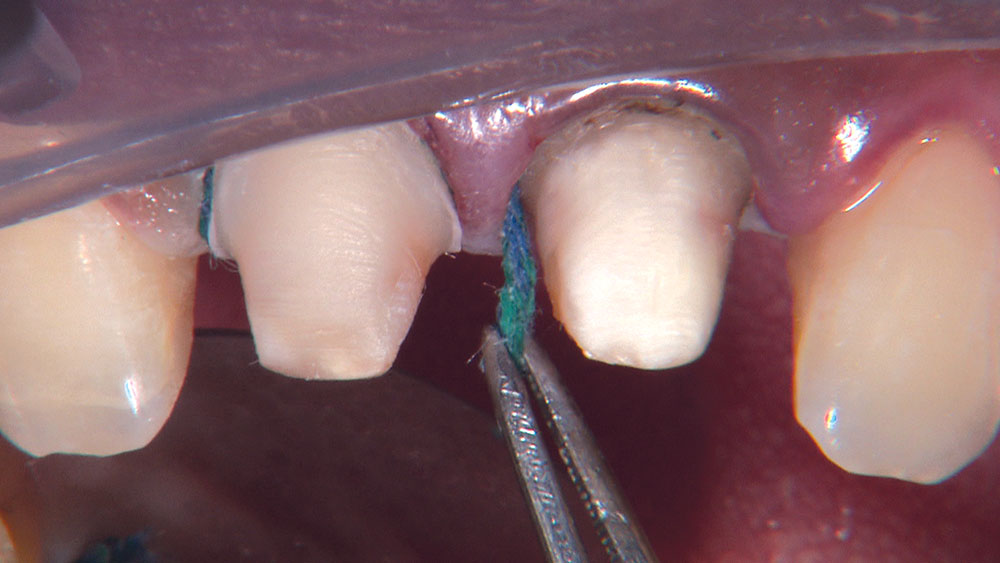
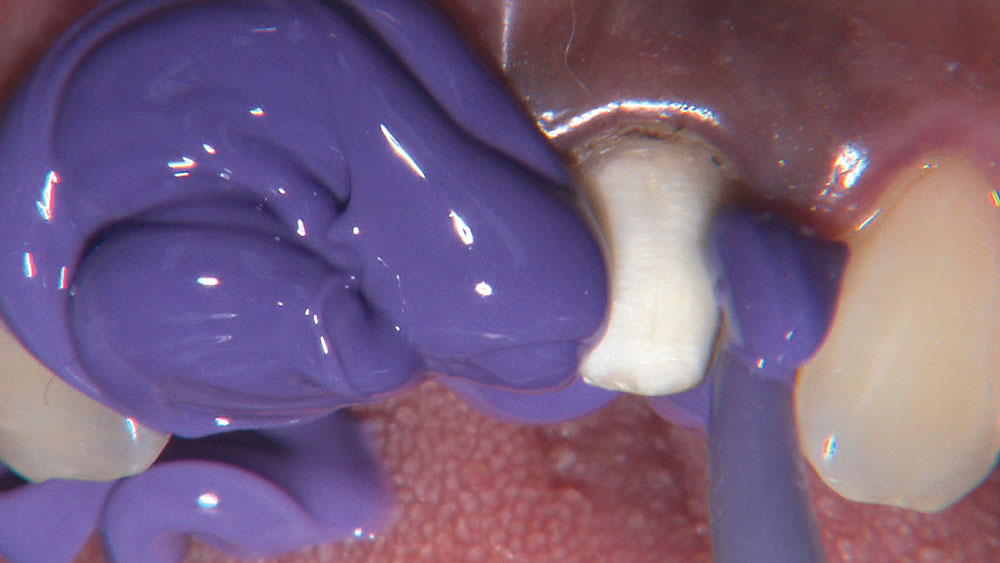
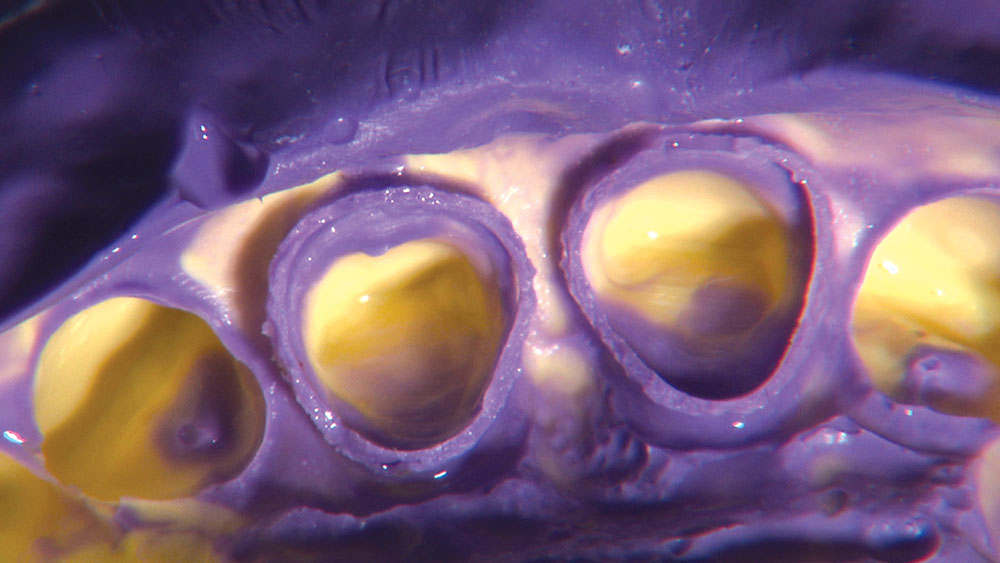
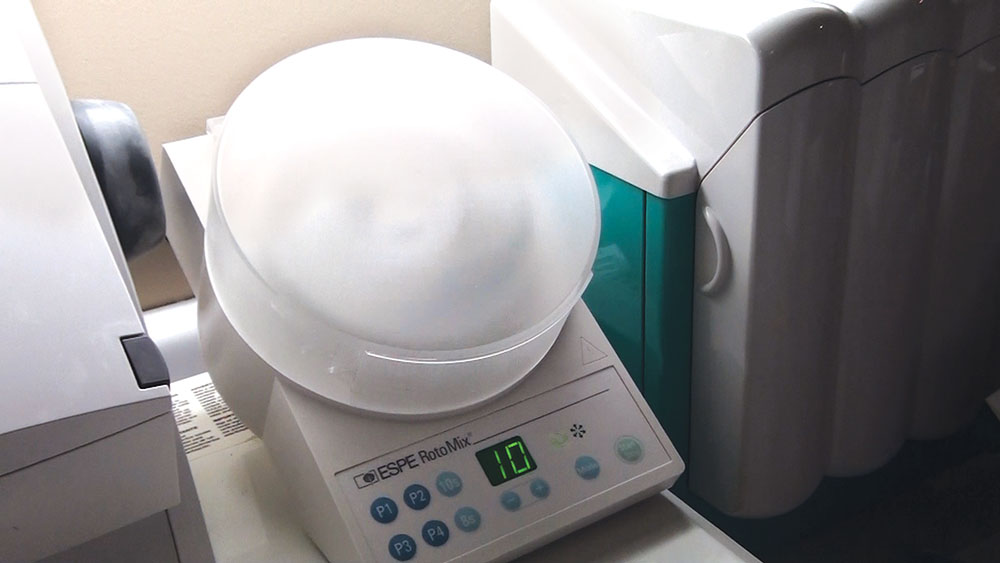
Glidewell Laboratories continues to test what the lab can do with BruxZir® Solid Zirconia crowns & bridges as it works to improve the esthetic nature of this zirconia material. BruxZir crowns now account for 15% of the anterior crowns fabricated at the lab, and as this number will likely continue to rise, the lab is committed to increasing the material’s ability to be predictably prescribed in anterior situations. This photo essay illustrates a case where we are prepping teeth #8 and #9 for BruxZir crowns. Tooth #8 is a natural tooth that has been endodontically treated, and tooth #9 has an existing PFM that needs to be replaced. To view a live video of the case, visit our Video Gallery.