The Zirconia-Based Porcelain Veneer

Dentistry is both an art and a science requiring today’s practitioner to be versatile and ready to adapt. Not every patient fits into the same treatment box, calling for an identical approach. A comprehensive examination is needed to discover and establish a list of each patient’s requirements.
Generally, most patients’ dental treatments call for conventional and time-tested procedures. However, at times we are faced with challenges that require us to be able to think and operate “outside the box,” relying on our ingenuity and creativity. As practitioners gain experience, they gather their own personal “bag of tricks” to turn to. New procedures and innovations in dental materials provide us with increasing options.
Case Report
Diagnosis and Treatment Planning
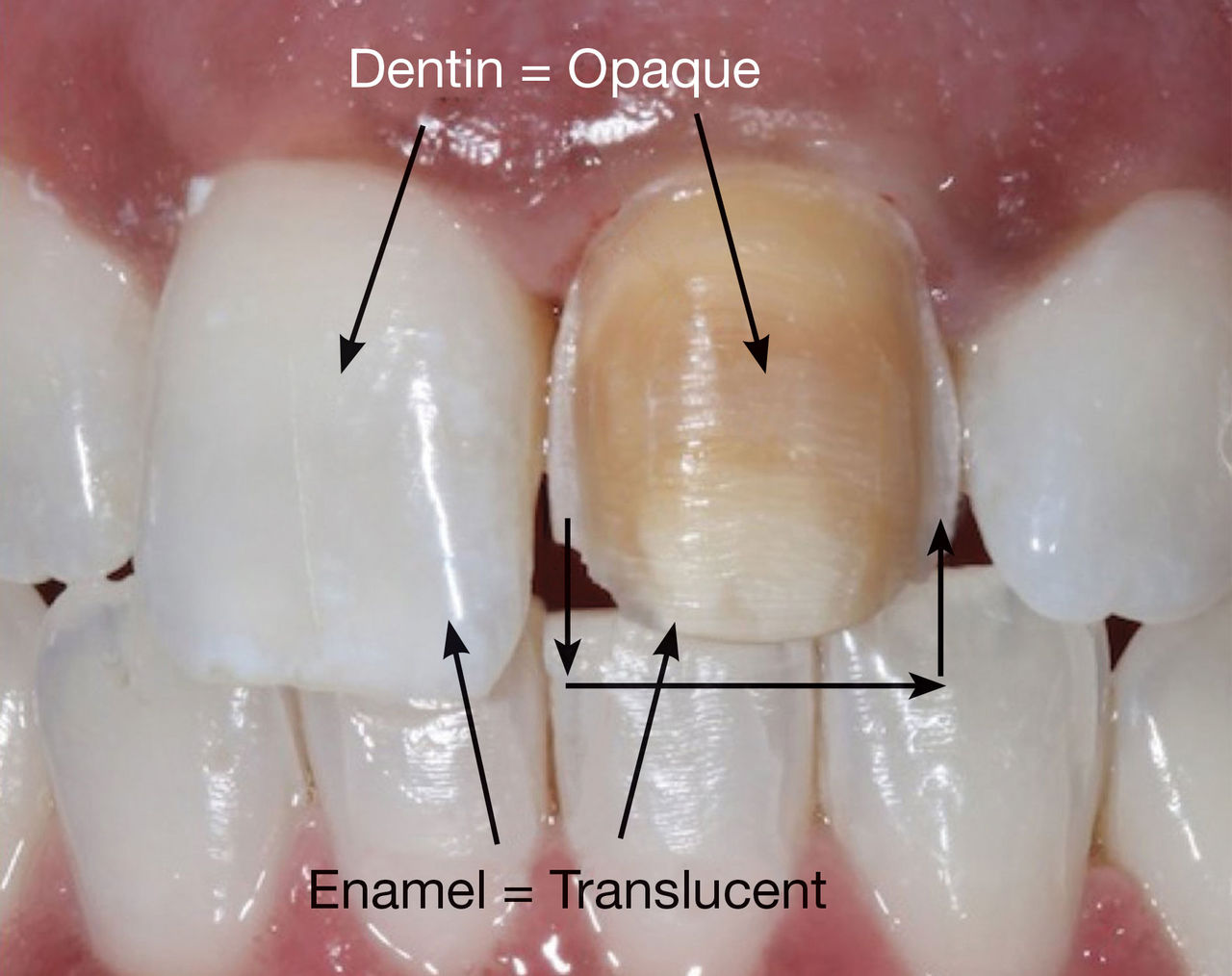
Our patient presented with a discolored upper left central incisor (Fig. 1). His dental history noted that trauma occurred to the tooth in his youth. His tooth tested vital and had never been restored. Although the dark tooth bothered the patient, he had always been reluctant to compromise its integrity. Full-coverage crowns, pressed-ceramic veneers and bonded-composite restorations had been previously proposed as possible esthetic solutions. However, these restorations called for significant tooth reduction in order to mask the dark underlying dentin. Because his tooth was healthy and asymptomatic, he had been seeking a more conservative option.
Presented with the desires of the patient, we studied his restorative choices and considered the currently available dental materials. An ultra-thin zirconia core veneered with porcelain was acceptable to him.
Zirconia has recently become a popular dental material because it has high strength, is resistant to fracture and, being opaque, has the ability to mask discolored underlying tooth structure.1 Its flexural strength of 900 to 1,100 MPa and fracture toughness of 8 to 10 MPa make it a suitable material to create both conservative esthetic restorations and pontic spans for bridge work. It can be milled to a 0.2 mm thickness and then layered with a compatible porcelain to yield a restoration of less than 0.6 mm in total thickness. A restoration of this nature would be minimally invasive, with the ability to alter the color of the dark tooth to approximate that of the other central incisor. However, in order to achieve a restoration of this description, we require the necessary chemistry to create adhesion between the zirconia and the tooth.
To understand the challenges of the required chemistry, we must realize that enamel and dentin are living tissue requiring primers and adhesives that infiltrate into created microretention on the surface. Zirconia is a nonliving, oxide-based substrate requiring a primer with phosphate comonomers to covalently bond to the oxide. In order to fuse the zirconia to the tooth, we require a cement interface that cohesively re-creates the dentoenamel junction among the living enamel, dentin and the inert zirconia oxide-based substrate. The resin cement chosen should be hydrophobic and dual-curing (light- and self-curing), as zirconia is opaque and may not allow light to totally pass through it to fully cure the resin.2,3,4
Until recently, the zirconia-to-tooth bonded interface was not possible, as hydrophobic cements do not adhere to oxides. New products, however, such as Z-PRIME™ (Bisco Inc.; Schaumburg, Ill.), have been developed. These are primers that utilize a combined phosphate and carboxylic monomer to create a cohesive interface, allowing the hydrophobic resin cement to create a linked, cohesive hydrophilic seal between the tooth and the indirect zirconia restoration. New universal primers (such as Monobond® Plus [Ivoclar Vivadent; Amherst, N.Y.]) have also been developed to accomplish this task with zirconium oxide, metals, porcelain glass and lithium disilicate.
Understanding the properties of our restorative materials and their limitations allows us to work creatively within the parameters that we are given.
Clinical Treatment
An initial reference shade was taken and photographed before any preparation to the tooth occurred. The other incisors matched a VITA® (Vident; Brea, Calif.) A1 shade (Fig. 2).
An impression of the unprepared tooth was then taken using a clear plastic tray in order to have a matrix ready for subsequent bis-acryl temporary fabrication. This clear silicone impression material, Affinity™ Crystal (CLINICIAN’S CHOICE; New Milford, Conn.), allows the dentist to visualize the underlying teeth as a reference, making it easy to reposition in the patient’s mouth when filled with the provisional material (Fig. 3).
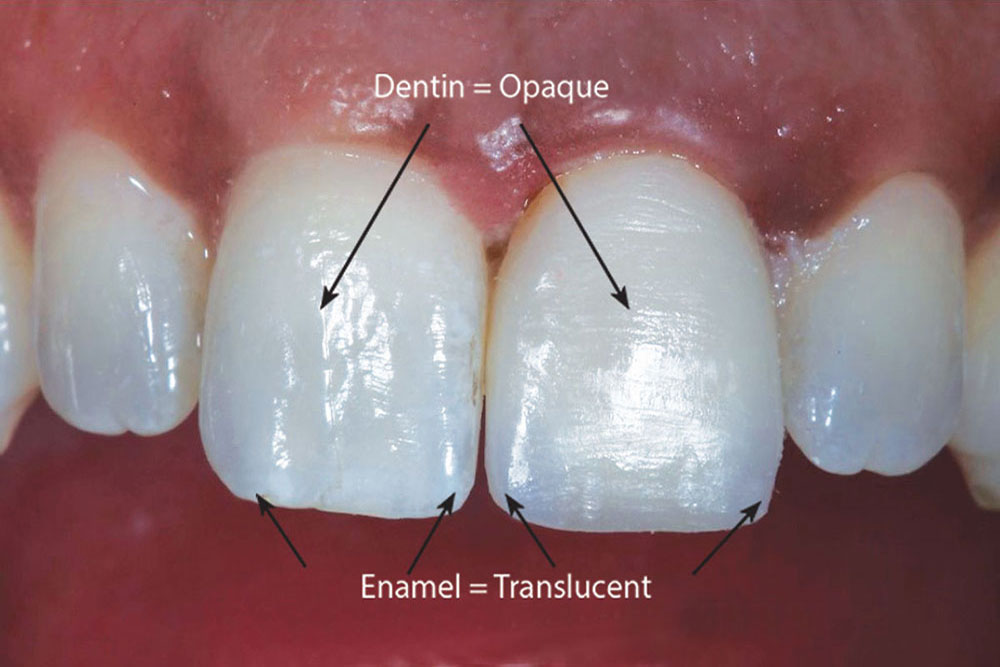
After labial reduction of 0.6 mm, we had removed the outer layers of translucent enamel, thus exposing the darker underlying hue of the dentin that creates the tooth’s color. Zirconia oxide is typically a very opaque material that does not provide for natural translucency and light reflection. It should be noted that several translucent zirconia-based materials have been recently introduced into the marketplace to address certain esthetic concerns (such as inCoris™ TZI [Sirona Dental Systems; Charlotte, N.C.], Zenotec CAD/CAM [Wieland Dental Systems; Danbury, Conn.] and BruxZir® Solid Zirconia [Glidewell Laboratories; Newport Beach, Calif.]).
Understanding the properties of our restorative materials and their limitations allows us to work creatively within the parameters that we are given. Incisal reduction of 1.0 mm was created so that the incisal edge of the veneer could be fabricated in pure feldspathic porcelain. This design would allow our ceramist to create transparencies and internal coloration similar to that of the adjacent natural tooth. In addition, deeper preparation on the mesial and distal line angles would enable the ceramist to develop a translucent effect in these areas (Fig. 4). The areas of discolored dentin would be masked out with the opaque zirconia.
Next, the shade of the underlying prepared tooth was selected and photographed (Fig. 5). This was done in order for the ceramist to create a corresponding die as a color reference.
Understanding the properties of our restorative materials and their limitations allows us to work creatively within the parameters that we are given.
Before taking the final impression of the prepared tooth, our procedure protocol is to fabricate a preliminary provisional restoration using a bis-acryl provisional material (such as Luxatemp® Ultra [DMG America; Eaglewood, N.J.], Protemp™ Plus [3M™ ESPE™; St. Paul, Minn.] or Integrity® [DENTSPLY Caulk; Milford, Del.]). This initial provisional serves both as a preparation check, allowing the clinician to assess if enough tooth structure was removed to accommodate the desired restoration, and to also verify that the correct shade of bis-acryl provisional material was chosen. Our office protocol calls for the dental assistants to use an operatory timer that is set to reflect the setting time as noted in the manufacturer’s instructions for the material being used. The timer was set for two minutes (as required for the Luxatemp Ultra used in this case) (Fig. 6a), and then the bis-acryl material was injected into the previously obtained clear silicone matrix impression (Fig. 6b) and positioned over the prepared tooth. The provisional material was allowed to set on the tooth, so that we could check to see if we had achieved an adequate and uniform preparation to accommodate the required thickness of the restorative material selected for this case (Fig. 7). Any modification needed can be done to the preparation by directly cutting through the bis-acryl, which serves as our reference. In this case, we needed to reduce the tooth a bit more on the labial surface (Fig. 8).5 After the preparation was completed, a final provisional restoration was fabricated and set aside to harden.
It is important to emphasize that, by using the bis-acryl provisional as a preview, we eliminated the need for our dental laboratory team to inform us of underpreparation/insufficient room; this also obviated the need for the patient to return to our office to modify the tooth and to take a new impression. Having to reanesthetize, retemporize, reprepare and reimpress (the author refers to this as “redo-a-dontics”) is not fun for either the patient or the dentist!
The patient’s bite was taken using a rigid bis-acryl bite registration material (LuxaBite® Ultra [DMG America]) placed in the anterior region from canine to canine (Figs. 9a, 9b). This is a thixotropic material that offers minimal resistance to closure; and once set, it has a D-69 Shore scale hardness that prevents any flexure/distortion, allowing the accurate transfer of the patient’s bite to the articulator. Unlike many silicone bite registration materials, it is a bis-acryl material designed to yield precise mounting and orientation of the plaster models.6 Again, the assistant set the operatory timer to a setting time of two minutes, according to the manufacturer’s instructions. There was no reason to extend the registration beyond the canines because the posterior bite was extremely stable; in this way, it was easily visually verified that the patient was biting in maximum intercuspation.
The final upper impression was taken using an extremely firm vinyl polysiloxane (VPS) impression material (Honigum® Putty [DMG America]). The Honigum Putty, which was dispensed from an automatic mixer (MixStar® eMotion [DMG America]), has a setting time of five minutes. It easily displaced the very viscous KOPY Single Crown Light Body (Dental Savings Club; Montreal, Quebec, Canada) into the subgingival sulcus, yielding a sharp and accurate impression. The author has found that this impression material is pleasant tasting and is easily removed from the mouth. The opposing lower model was taken with a VPS alginate substitute (StatusBlue® [DMG America]). Totally rigid and inflexible metal impression trays (Rim-Lock® Metal Trays [DENTSPLY Caulk]) were used for both impressions, thus minimizing distortions and inaccuracies.
Next, the patient’s tooth was cleaned and treated with a desensitizing agent (Gluma® [Heraeus Kulzer; South Bend, Ind.]). The provisional restoration was then cemented with a translucent, dual-cured, eugenol-free resin temporary cement (Temp-Bond® Clear [Kerr Corp.; Orange, Calif.]).
Brief Synopsis of the Dental Laboratory Protocol
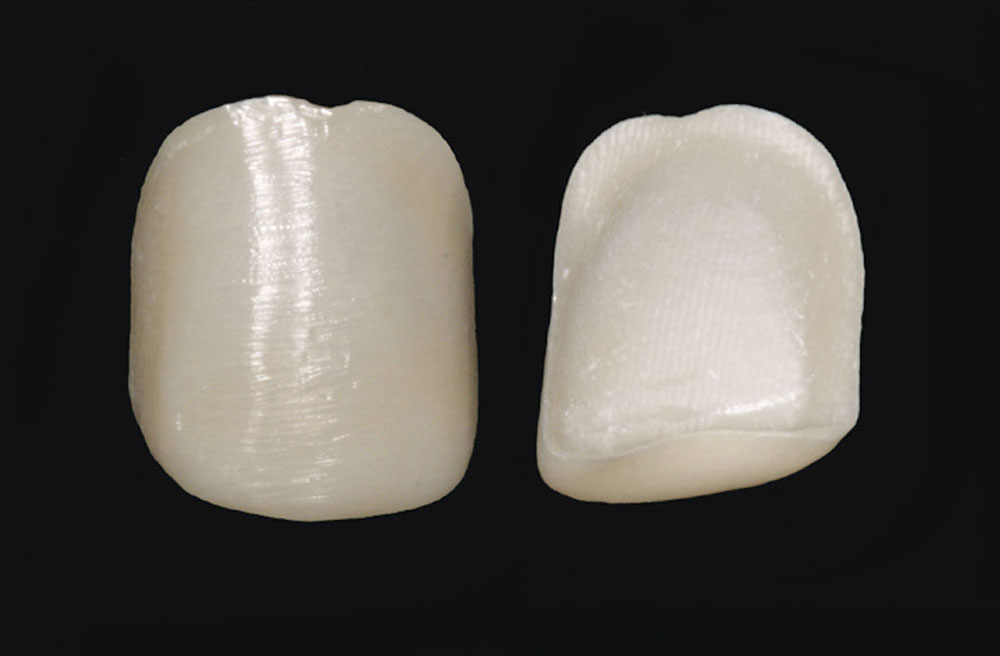
At the dental lab, a sintered zirconia core (keyed to the desired A1 shade) was milled using the Zenotec T1 7-axis CAD/CAM milling system to a thickness of 0.2 mm (Fig. 10). A feldspathic porcelain (Cerabien™ ZR [Kuraray America; New York, N.Y.]) was used to create a 0.4 mm porcelain buildup (laminate) over the zirconia substructure, yielding a total restoration thickness of 0.6 mm. The Noritake feldspathic porcelain has a coefficient of thermal expansion carefully matched to the zirconia, permitting the ceramist to create lifelike esthetics that display internal detailing and transparencies. The finished zirconia veneer offers precise marginal fit, excellent esthetics and high strength.
Delivery of the Final Restoration
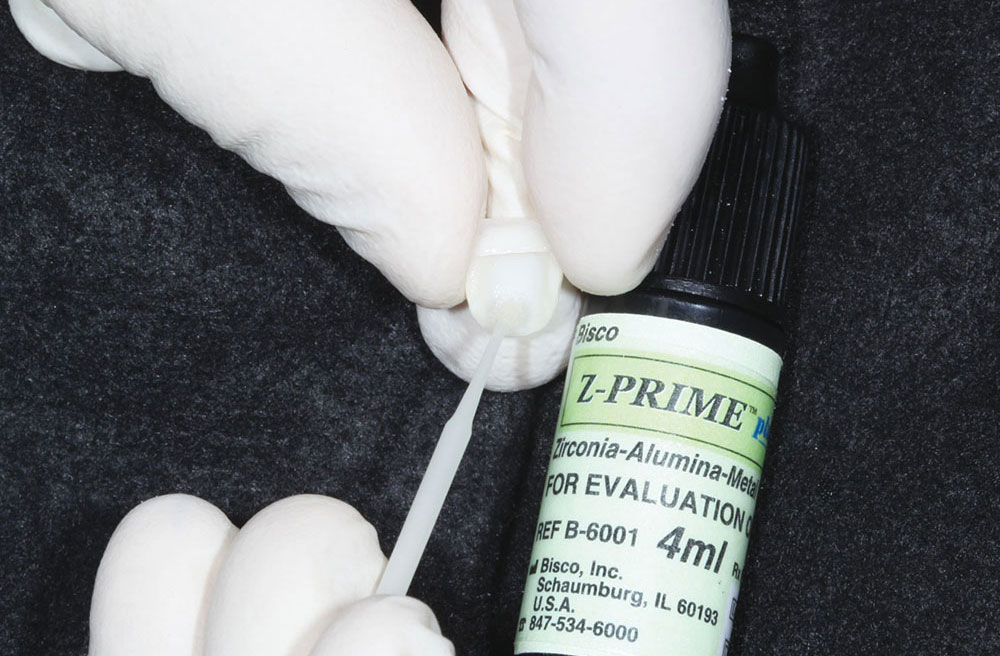
Upon receiving the restoration from the laboratory, its fit was verified on the laboratory work model to ascertain that it met our expectations. We then telephoned the patient to schedule an appointment. (In our office protocol, delivery appointments are not prescheduled according to the lab return dates, as we always want to have the flexibility of being able to return the case to the dental laboratory team if obvious corrections are needed.) In this case, the restoration was acceptable as received from the laboratory, so the internal surfaces were treated with a zirconia primer (Z-PRIME) (Fig. 11). The phosphate monomer in this special primer interacts with the oxide surface of the zirconia to form a covalent bond, thus optimizing the bond strength between the resin cement and the zirconia surface.
With the patient in the chair, and before removing the provisional, we first assessed the esthetics of the restoration next to the natural teeth to see if they looked the same (Fig. 12). If they had not, we would have returned the case to the dental ceramist with photos and a description of the changes required.
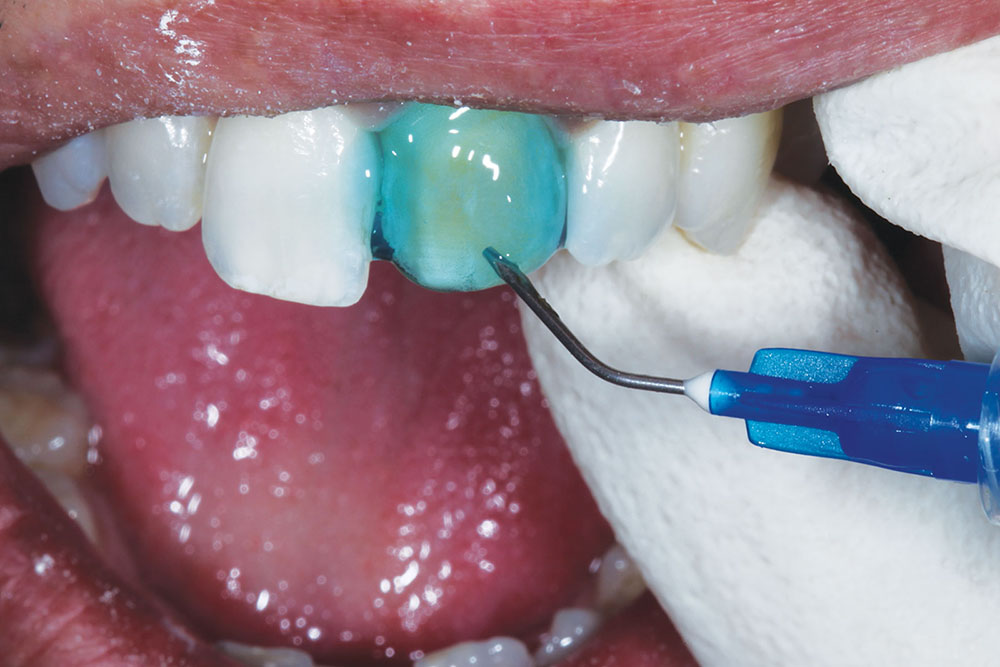
Once approved, the provisional was removed by first placing a slit in the labial surface using a flame-shaped diamond (KUT 3205 C [Dental Savings Club]). It was then separated and removed using an EB134 instrument (Brasseler USA; Savannah, Ga.) (Figs. 13a–13c). The underlying prepared tooth was cleaned with pumice, and then treated with a 32% phosphoric acid gel (UNI-ETCH® [Bisco Inc.]) containing benzalkonium chloride, an antimicrobial agent (Fig. 14). A universal adhesive (ALL-BOND UNIVERSAL™ [Bisco Inc.]) with low film thickness was then brushed on the tooth structure (Fig. 15).
Next, a resin cement (DUO-LINK™ SE Kit [Bisco Inc.]) was applied to the internal surface of the veneer (Fig. 16), and then it was placed on the tooth and light-cured (VALO® LED Curing Light (Ultradent Products Inc.; South Jordan, Utah) (Fig. 17). The VALO LED light produces a high degree of polymerization.7,8 Furthermore, its curing tip can be easily placed at a 90-degree angle to the labial surface of the tooth, allowing optimum light penetration.
Designing the tooth preparation specifically to accommodate the application of the ceramic materials chosen in this case was very important. This thoughtful protocol resulted in areas of translucency, transparency and internal detailing, providing a definitive restoration with lifelike esthetics that satisfied our patient’s esthetic goals (Fig. 18).
Closing Comments
No single restorative material can satisfy every esthetic need. By having current knowledge of procedures and materials available, the practitioner is better able to adapt and satisfy the patient’s desires. Porcelain-layered zirconia veneers can be a useful addition to our dental “bag of tricks.”
Dr. Elliot Mechanic practices esthetic dentistry in Montreal, Canada. He is the esthetic editor of Canada’s Oral Health dental journal and is on the editorial board of Dentistry Today. Contact him via email at info@drmechanic.com.
Acknowledgment
The author would like to thank Adrian Jurim, CDT, MDT, for inspiration and the exquisite technical fabrication of this zirconia-based layered veneer (Zeneer™ [Jurim Dental Studio Inc.; Great Neck, N.Y.]).
References
- ^ Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008 Mar;24(3):299-307.
- ^ Tanaka R, Fujishima A, Shibata Y, Manabe A, Miyazaki T. Cooperation of phosphate monomer and silica modification on zirconia. J Dent Res. 2008 Jul;87(7):666-70.
- ^ Yoshida K, Tsuo Y, Atsuta M. Bonding of dual-cured resin cement to zirconia ceramic using phosphate acid ester monomer and zirconate coupler. J Biomed Mater Res B Appl Biomater. 2006 Apr;77(1):28-33.
- ^ Dérand P, Dérand T. Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont. 2000 Mar-Apr;13(2):131-5.
- ^ Gürel G. Predictable, precise, and repeatable tooth preparation for porcelain laminate veneers. Pract Proced Aesthet Dent. 2003 Jan-Feb;15(1):17-24.
- ^ Chan CA. Bite-management considerations for the restorative dentist. Dent Today. 2008 Jan;27(1):108, 110-3.
- ^ Price RB, Felix CA, Andreou P. Third-generation vs a second-generation LED curing light: effect on Knoop microhardness. Compend Contin Educ Dent. 2006 Sep;27(9):490-6.
- ^ Boksman L, Santos GC Jr. Principles of light-curing. Inside Dentistry. 2012 Mar;8(3):94-7.
Disclosure: Dr. Mechanic reports no disclosures.
Reprinted by permission of Dentistry Today, © 2012 Dentistry Today.