Biologic Shaping from a Restorative Perspective
In today’s world of advanced dental procedures and technology, traditional or classic dental principles can easily be lost. This may especially be true with the decision-making process of saving teeth. Implants are wonderful options when appropriate, but they should not be selected when a tooth can be saved using a predictable perio or restorative protocol that yields excellent long-term prognoses. Too often today, good teeth are being removed in favor of implant placement that is occurring in a clinical environment of inadequate bone and soft tissue, as well as biomechanical compromise. Biologic shaping and soft tissue grafting offer a classic, proven methodology for treating teeth with absolute predictability.
Often our restorative treatment plans lead us to subgingival margins, furcation involvement, root flutes and concavities, in addition to a multitude of complex issues. Many of the issues we face are in the subgingival environment and require periodontal corrective procedures to return the foundation to a healthy state. Traditionally, crown lengthening was indicated for deep subgingival margins, not only to facilitate impression making but also to correct biologic width infringements. Biologic shaping is a periodontal corrective procedure reported in the literature1 that may complement traditional crown lengthening, yet it differs from traditional crown lengthening in the following ways:
- Traditional crown lengthening moves the bone away from the margin. Biologic shaping moves the margin away from the bone.
- Traditional crown lengthening requires osseous surgery to re-establish the biologic width. Biologic shaping may require minor osseous surgery, but it generally avoids major osseous surgery and still re-establishes biologic width because you have the choice to locate your restorative margin coronal to the old restorative margin (0.5 mm apical to the core is the coronal extent).
- Traditional crown lengthening may open furcations and render a poor prognosis. Biologic shaping preserves the integrity of the furcation because aggressive osseous surgery was not needed.
- Traditional crown lengthening does not eliminate flutes, concavities or root clefts, leaving the postoperative lengthened crown at risk for disease recurrence due to increased susceptibility for plaque, calculus and caries formation. Biologic shaping leaves the subgingival area as smooth as glass; there are no areas for plaque, calculus or caries to hide.
- Traditional crown lengthening worsens crown-to-root ratio. Biologic shaping maintains crown-to-root ratio.
- Traditional perio is about pockets and probing. Biologic shaping is about preserving bone, smoothing out the rough spots, and making restorative dentistry predictable and a joy to perform.
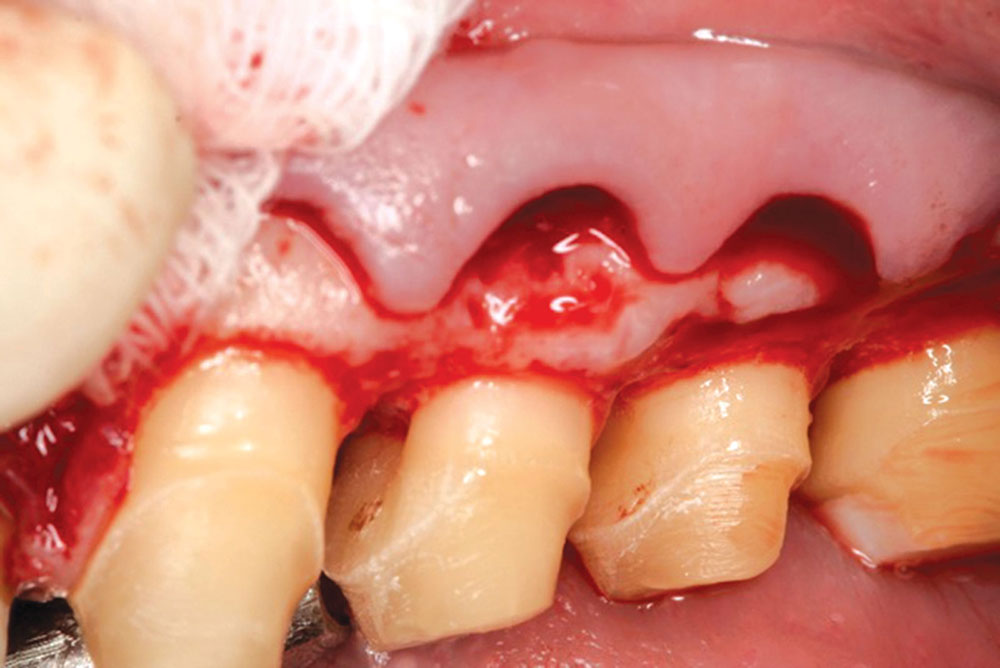
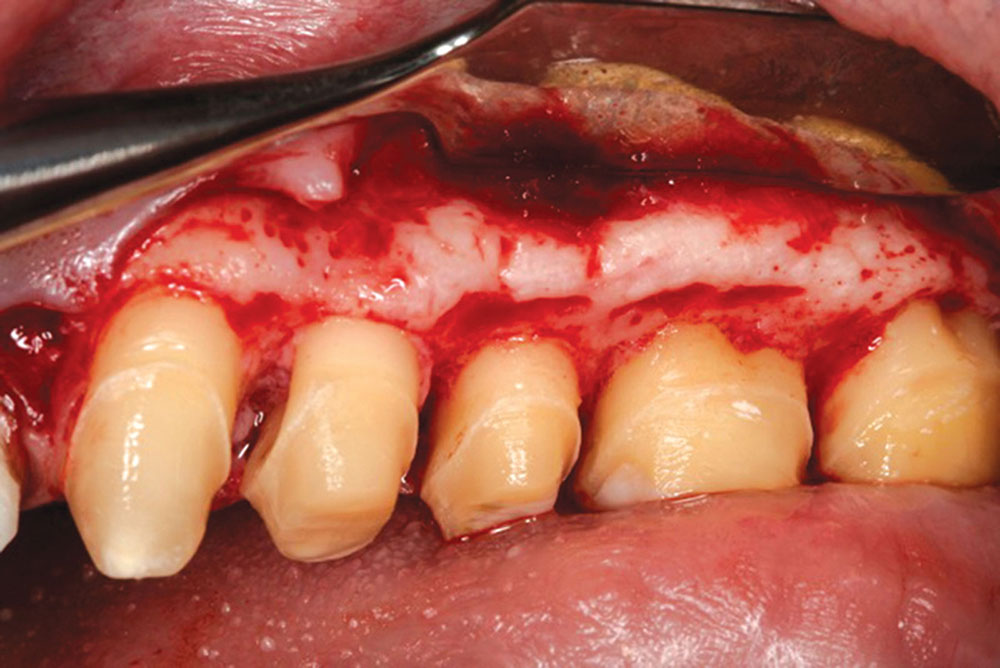
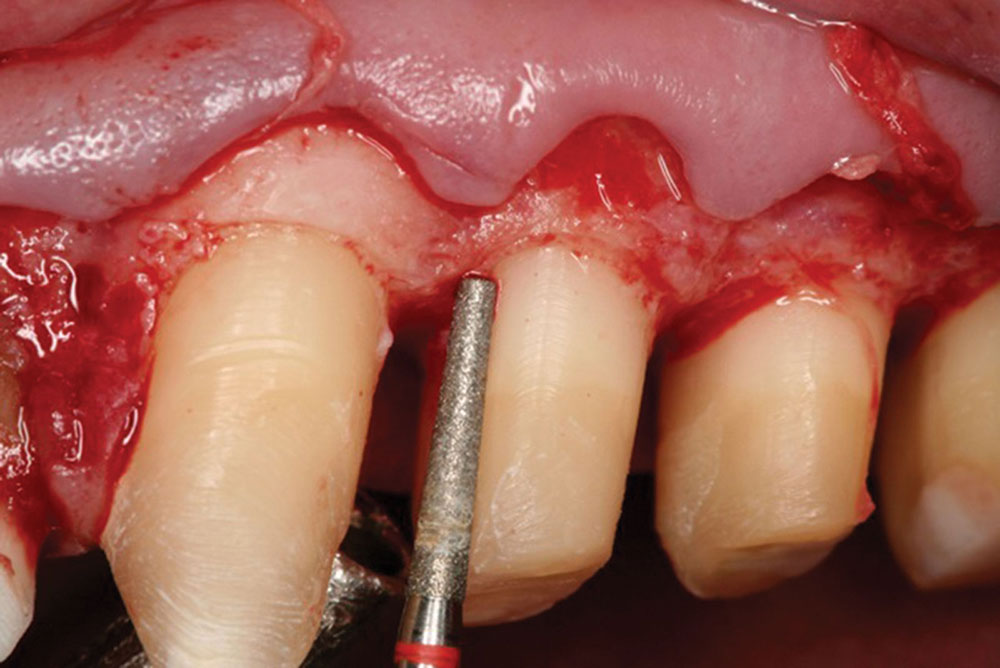
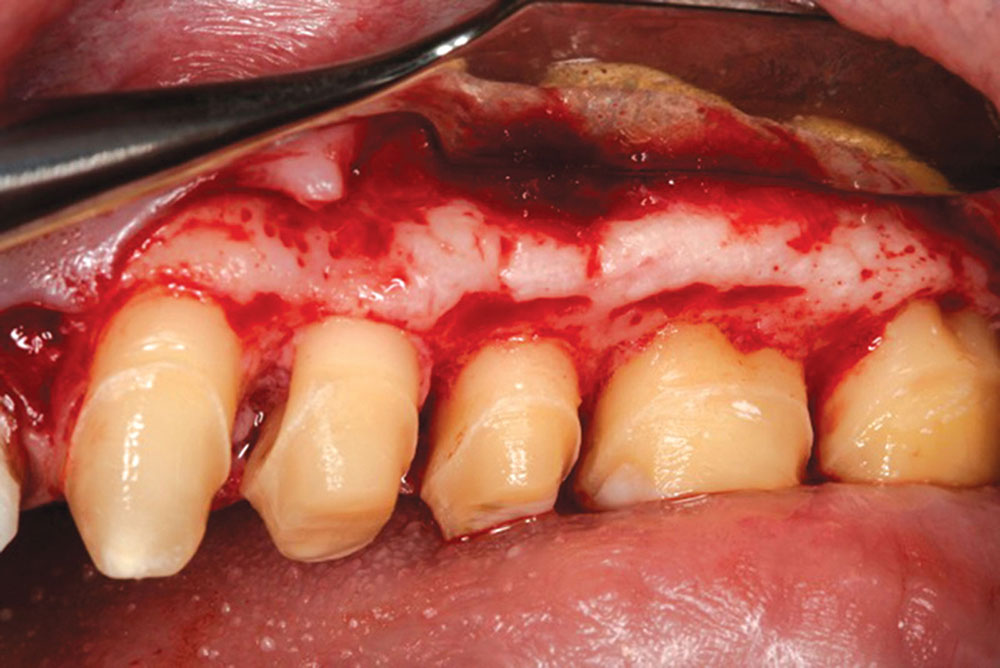
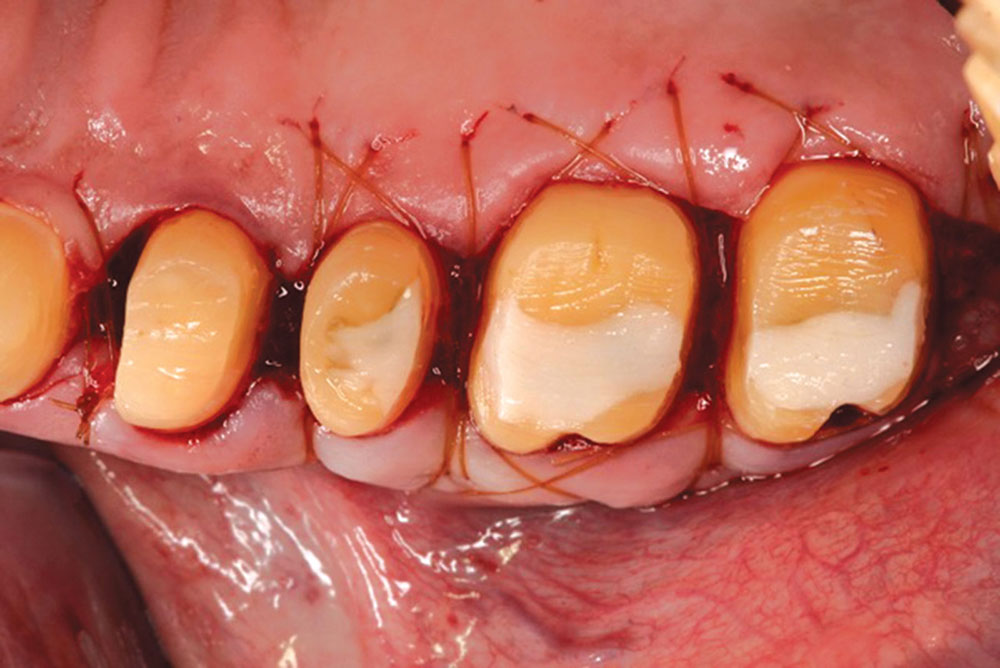
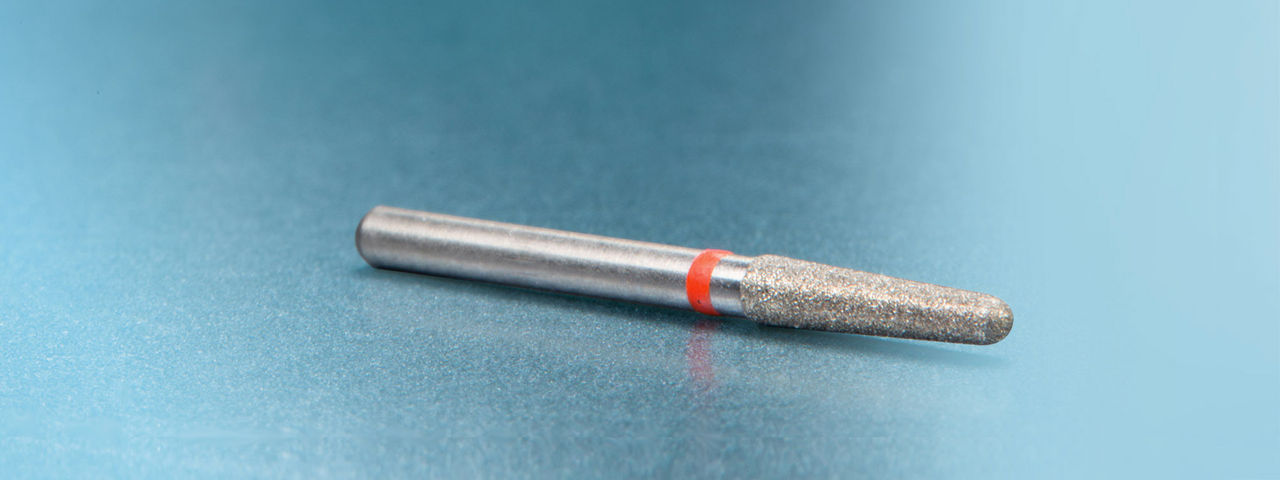
The concept of biologic shaping is presented in the case that follows. The procedure stresses a 360-degree removal of tooth surface irregularities as well as all cementoenamel junctions (CEJs) and existing margins. An important aspect of the procedure is to remove any concavities or furcation involvements. Once the root surfaces are perfectly smooth, the flap is placed just coronal to the osseous surface and sutured in place. After 12 to 14 weeks of healing, the restorative dentist simply places a new margin just coronal to the gingival collar, which allows for a perfect impression to be taken. This case also features the specific correction of a mesial concavity on an upper first bicuspid.
Case Presentation
Biologic shaping and soft tissue grafting offer a classic, proven methodology for treating teeth with absolute predictability.
Biologic shaping is about preserving bone, smoothing out the rough spots, and making restorative dentistry predictable and a joy to perform.
The procedure stresses a 360-degree removal of tooth surface irregularities … all CEJs and existing margins.
Dr. Daniel Melker is in private practice in Clearwater, Florida, and lectures nationwide on periodontics and prosthodontics. Contact him at 727-725-0100.