Photo Essay: Another Use for Anterior BruxZir® Solid Zirconia Restorations
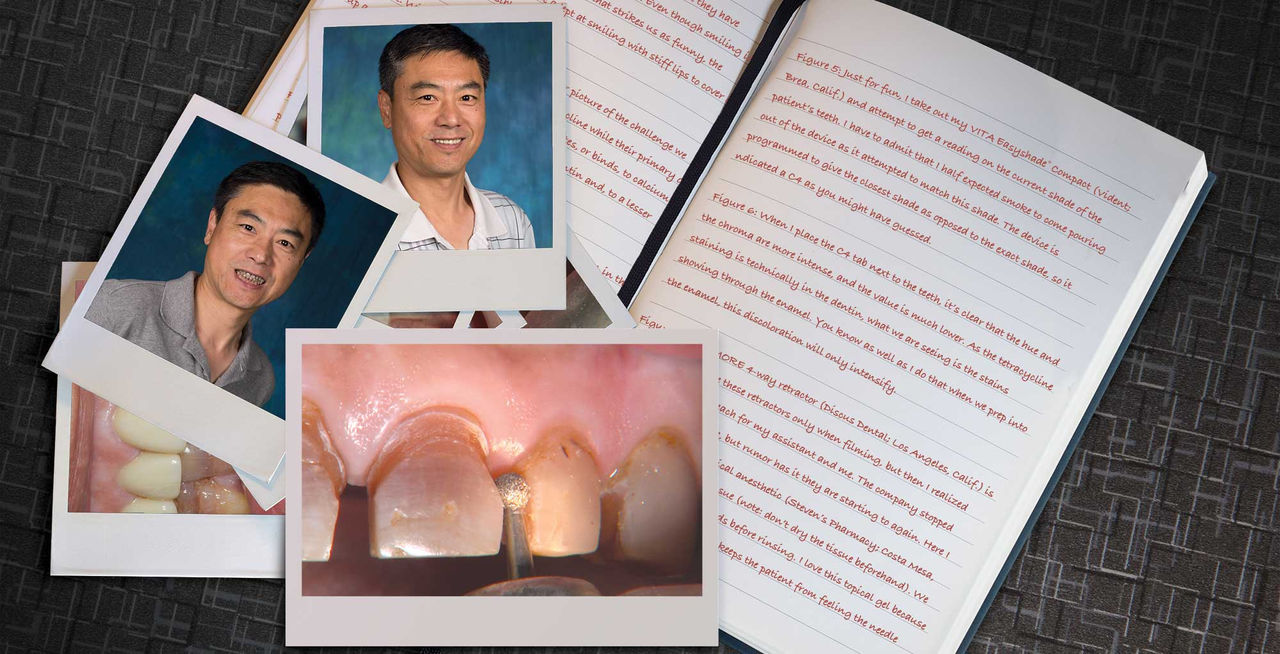
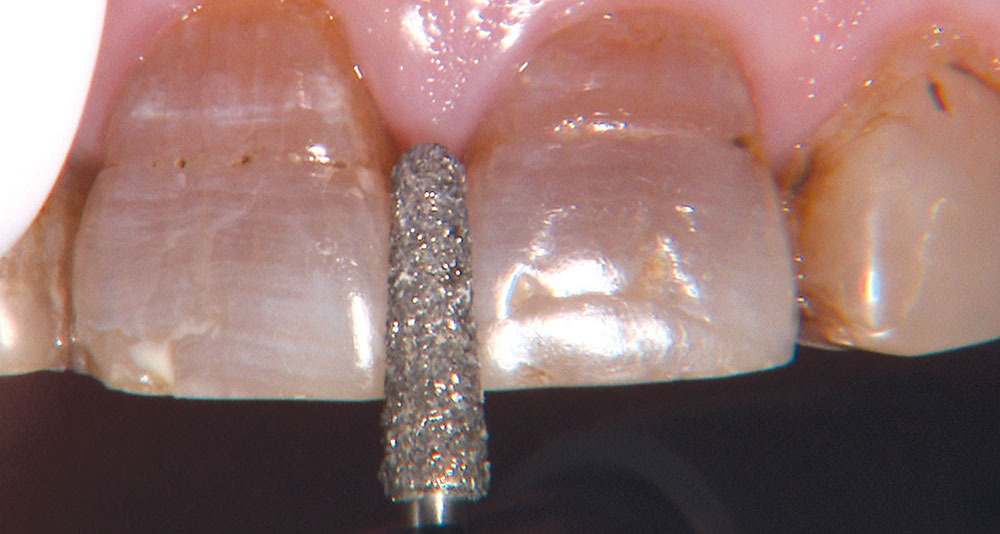
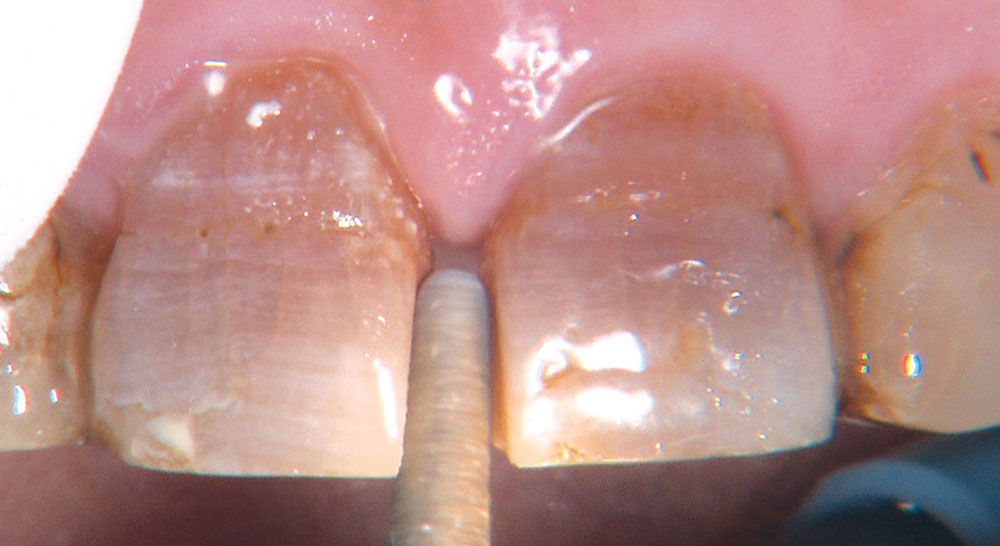
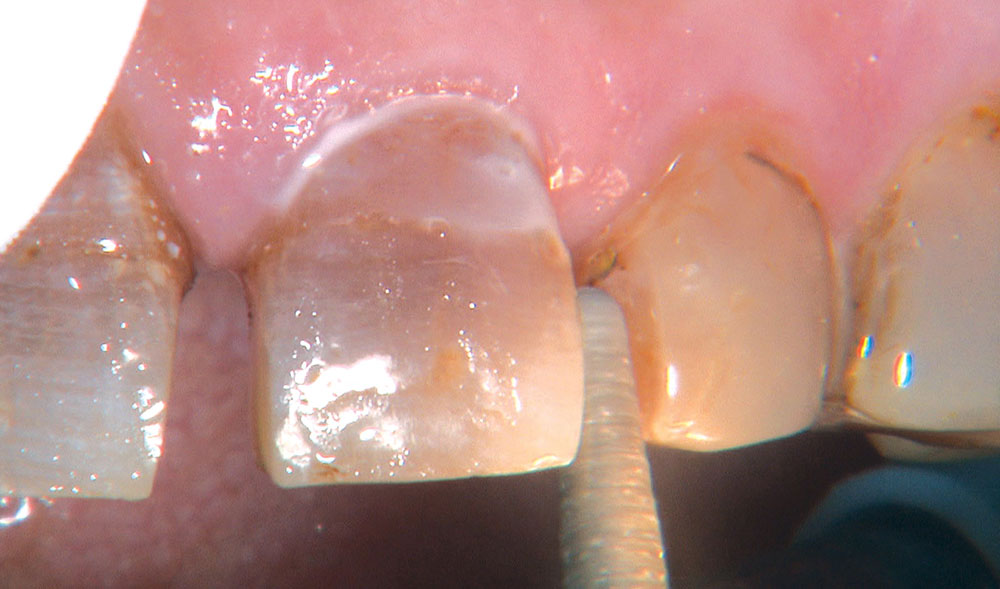
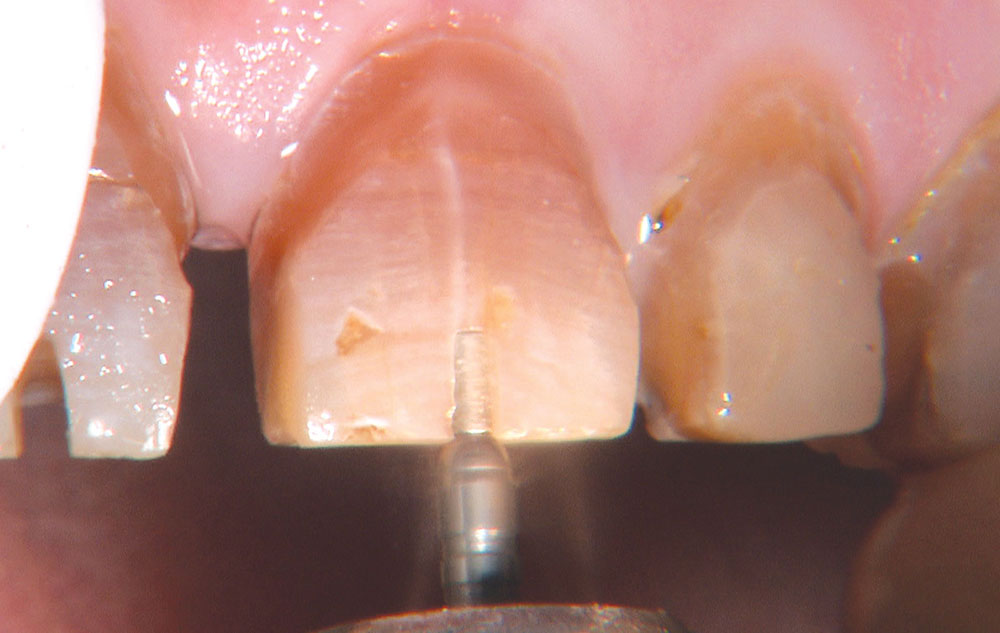
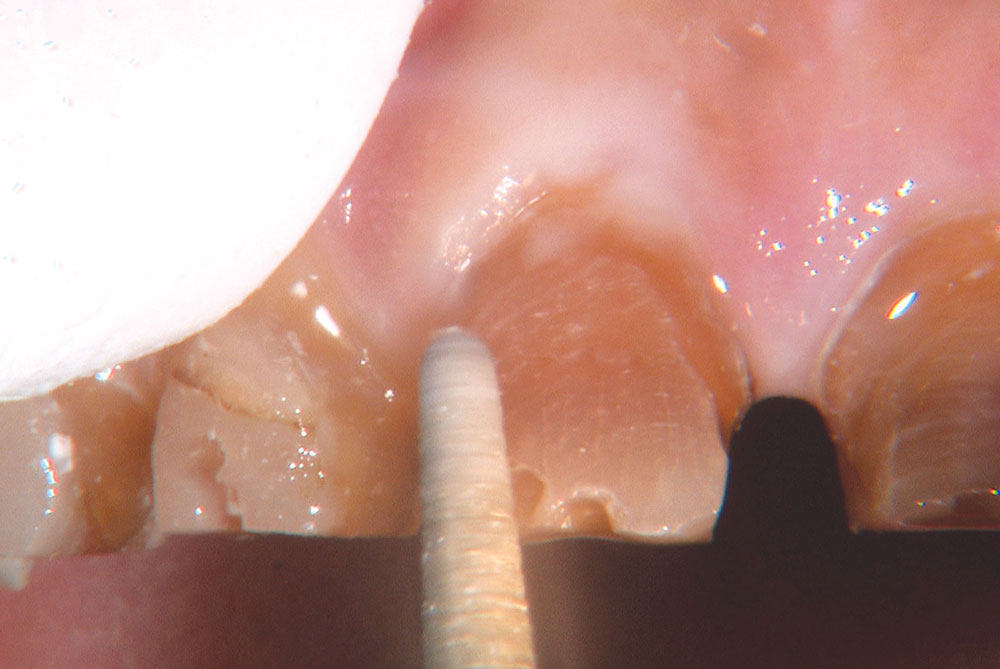
One of the most difficult clinical situations restorative dentists face in clinical practice is treating a patient with severe tetracycline staining. I treated one of these patients a few years ago with a set of veneers that were conservative but an esthetic compromise. The tetracycline stains showing through the veneers were still visible enough to bother the patient. When we removed the veneers six months later, I prepped 0.6 mm deeper to make the veneers thicker. But at the try-in appointment, it was clear that the esthetics hadn’t improved much from the first set. We ended up using lithium disilicate crowns, which provided an improved result, but there was still some minor show-through in the gingival third.
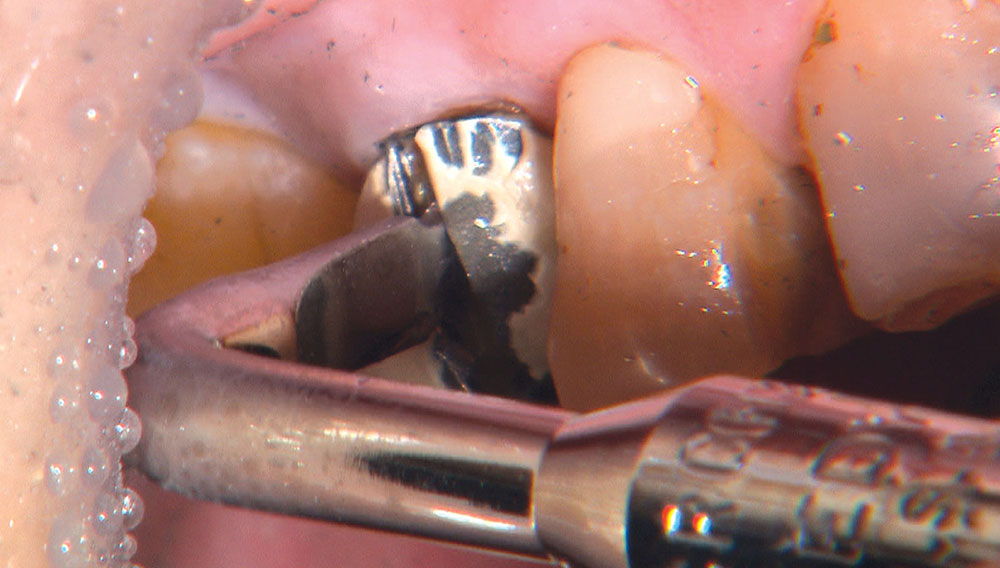
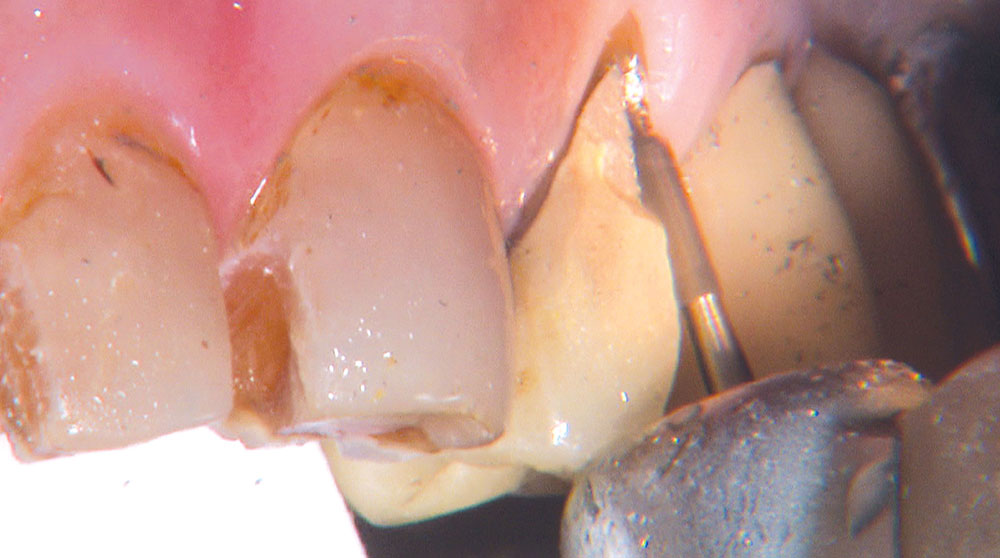
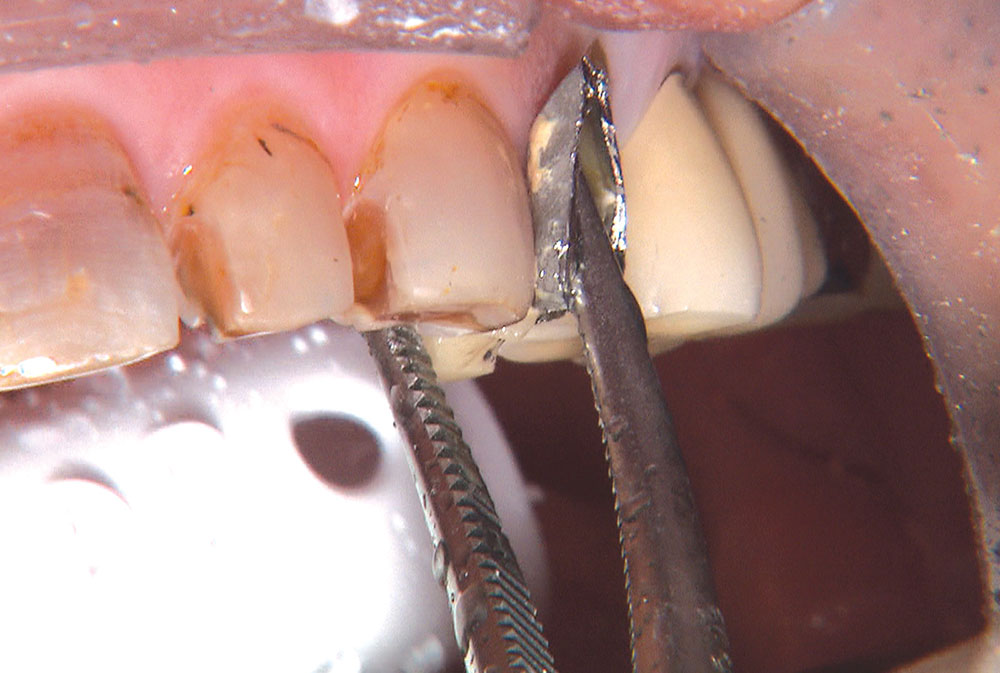
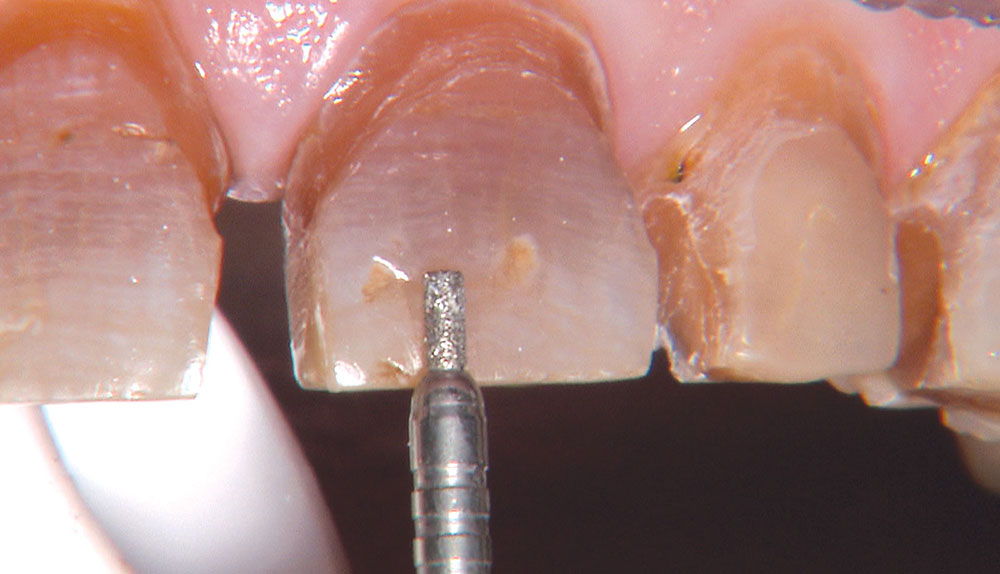
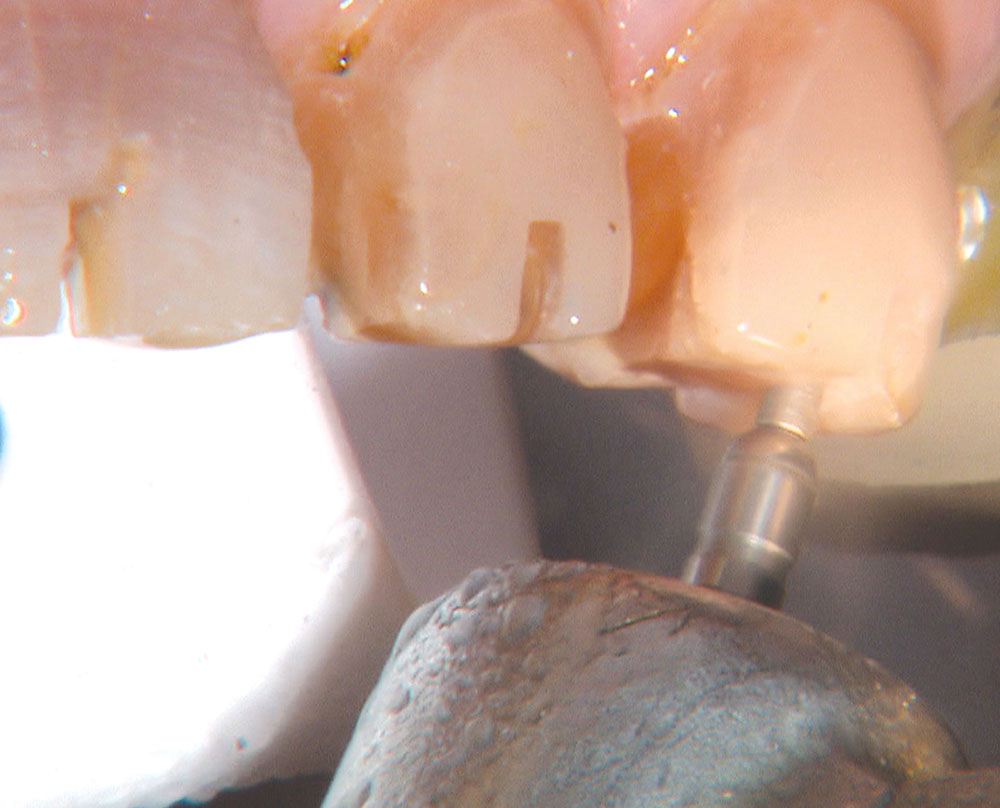
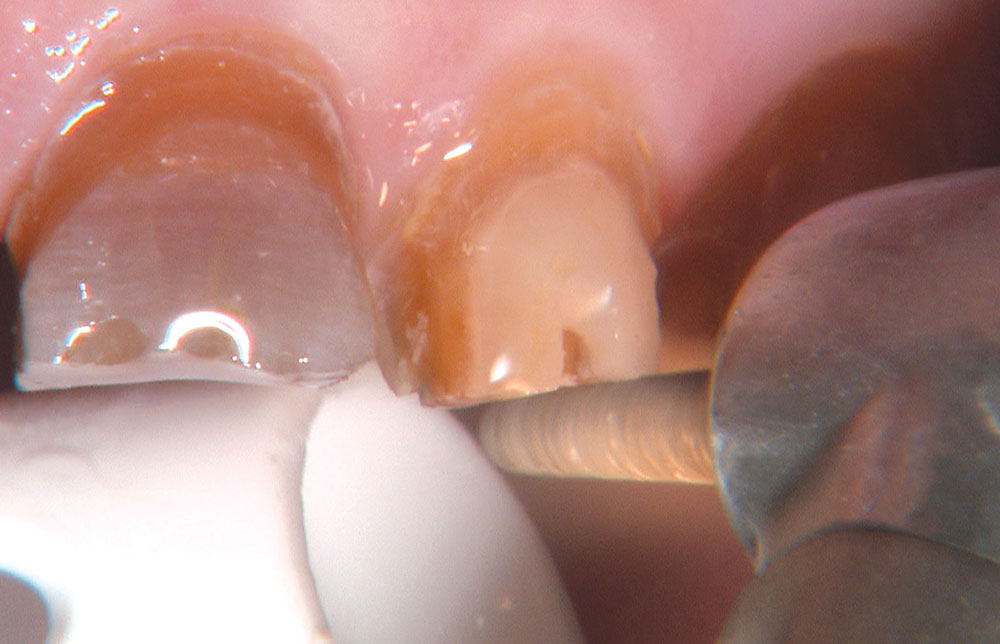
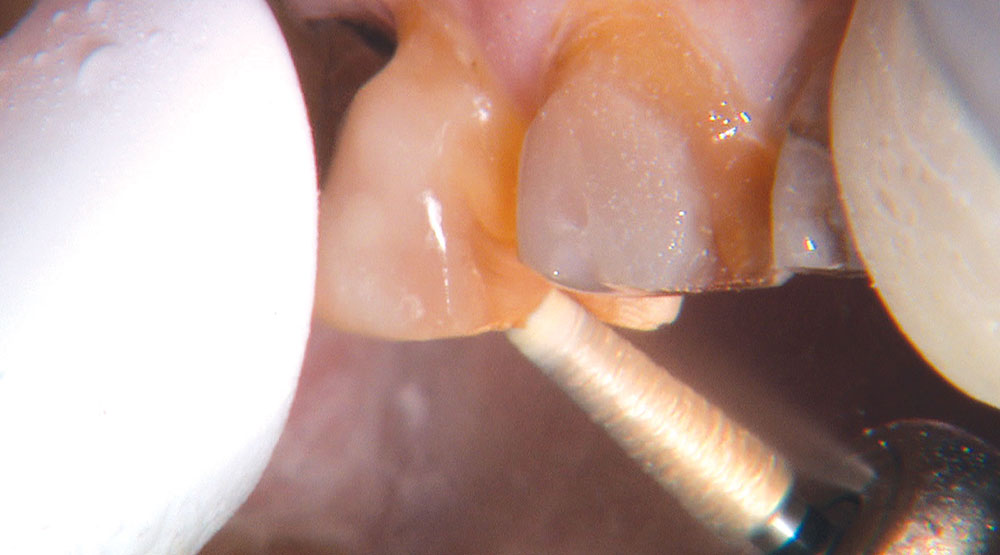
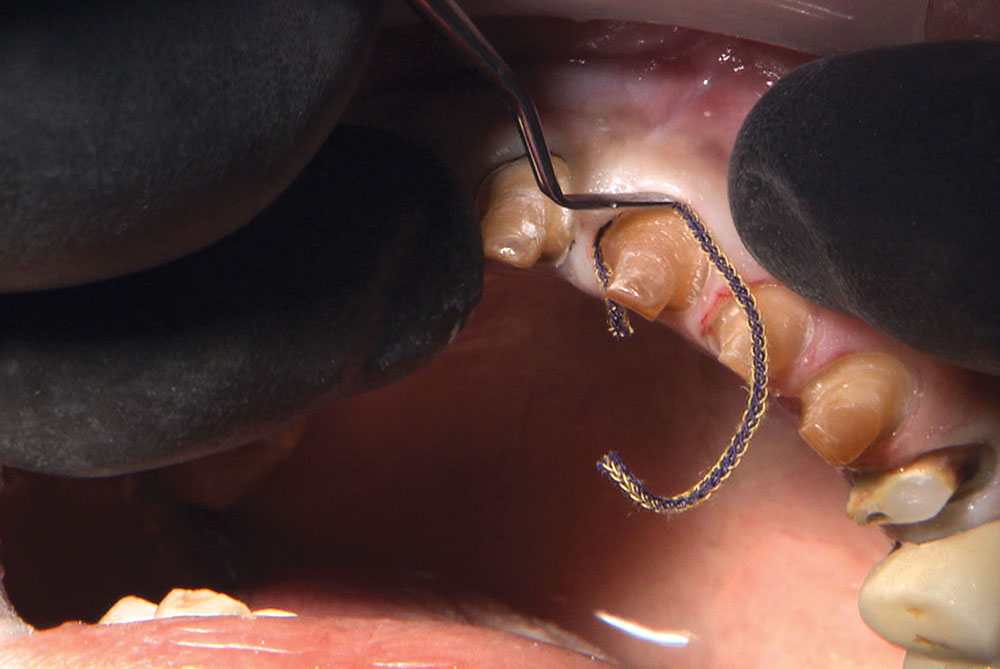
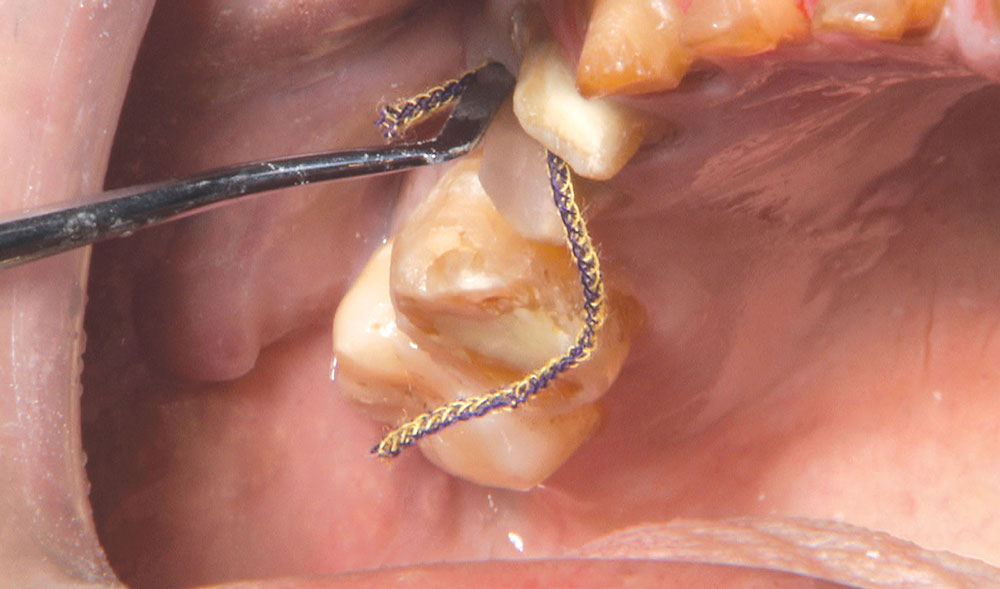
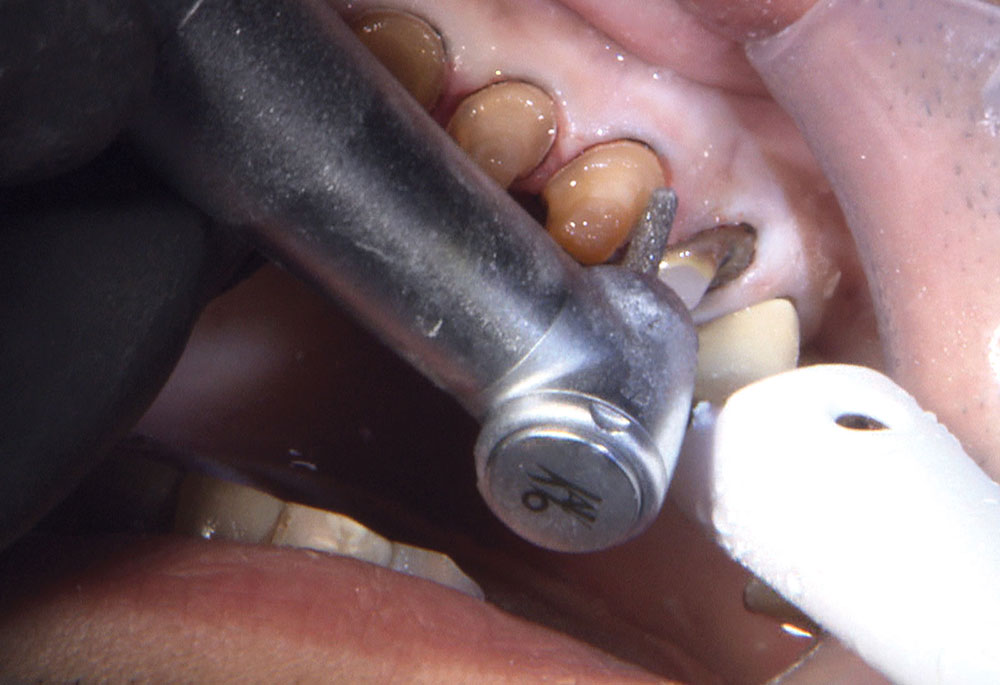
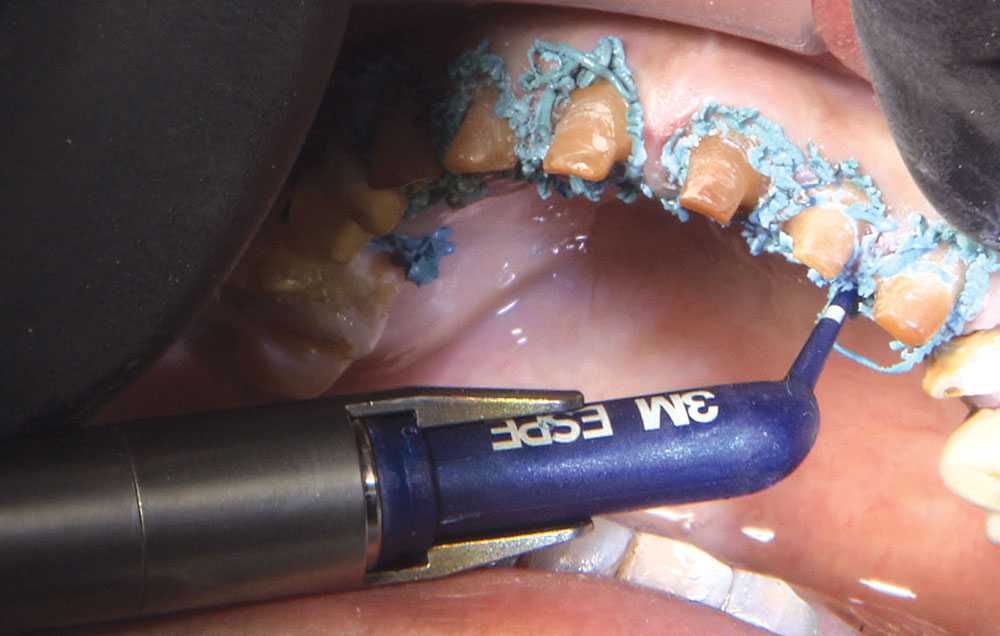
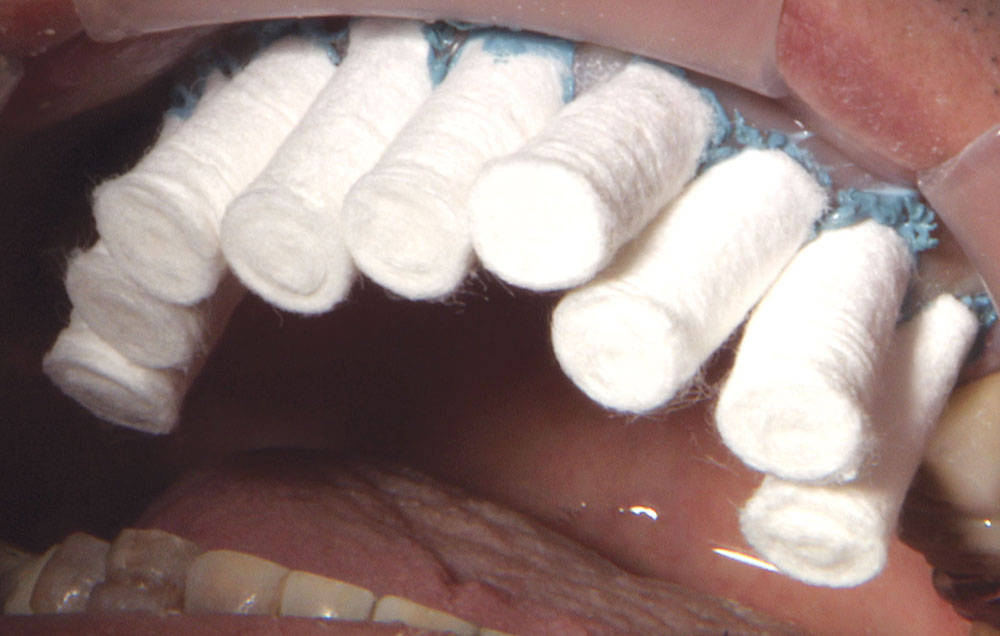
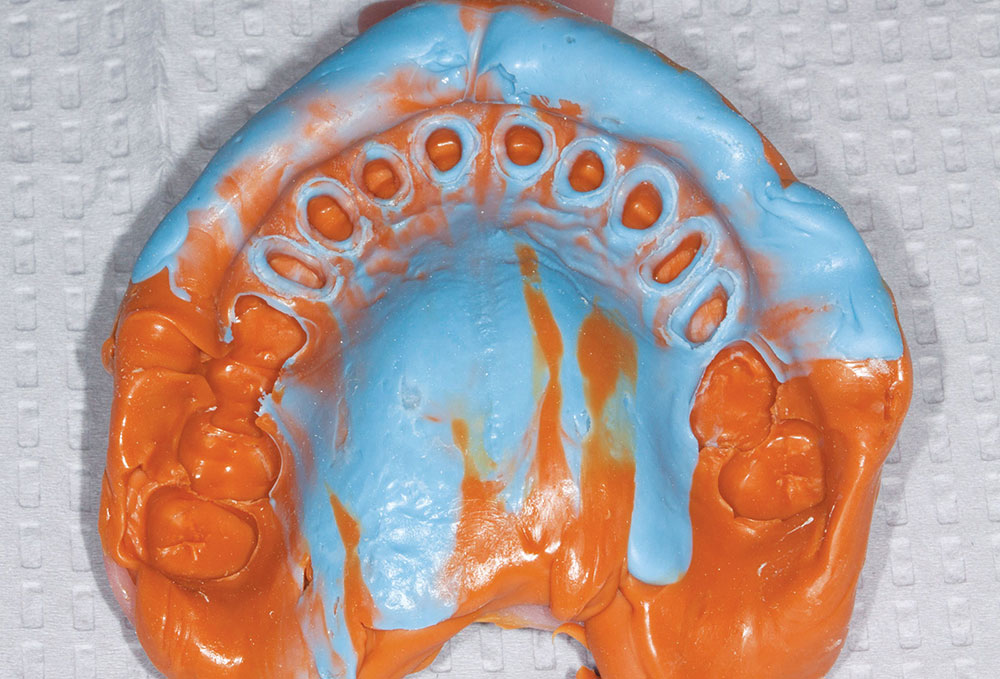
Not long ago, the patient’s brother came to see me. He was already prepared to do crowns, so I wanted to see if BruxZir® Solid Zirconia crowns (Glidewell Laboratories) could block out the prep shade. While not as esthetic as lithium disilicate crowns, I hoped to get a more esthetic overall result by entirely blocking out the stump shade. Unlike his sister, this patient had fractured nearly every PFM in his mouth, and the wear in his mouth and his edge-to-edge bite clearly revealed a severe bruxing habit. Taking this into consideration, I knew BruxZir Solid Zirconia was the only ceramic material that would stand a chance of surviving in this hostile oral environment.
References
- Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011 Jan;27(1):83-96.
- Holt LR, Boksman L. Monolithic zirconia: minimizing adjustments. Dent Today. 2012 Dec;31(12):78, 80-1.
- Janyavula S, Lawson N, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013 Jan;109(1):22-9.
- Rinke S, Schäfer S, Lange K, Gersdorff N, Roediger M. Practice-based clinical evaluation of metal-ceramic and zirconia molar crowns: 3-year results. J Oral Rehabil. 2013 Mar;40(3):228-37.
- Shahin R, Kern M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent Mater. 2010 Sep;26(9):922-8.
- Kern M, Swift EJ Jr. Bonding to zirconia. J Esthet Restor Dent. 2011 Apr;23(2):71-2.
- Sasse M, Eschbach S, Kern M. Randomized clinical trial on single retainer all-ceramic resin-bonded fixed partial dentures: Influence of the bonding system after up to 55 months. J Dent. 2012 Sep;40(9):783-6.