Fixing a Flawed Path of Insertion for a BruxZir Bridge Case of the Week: Episode 58
Our weekly web series “Chairside Live,” which highlights a case recently received at the lab in each episode, continues to be a great way for me to share useful clinical tips and discuss potential pitfalls with our dentist viewers. If you have yet to tune in, episodes can be viewed on-demand at chairsidelive.com, or on YouTube and iTunes.
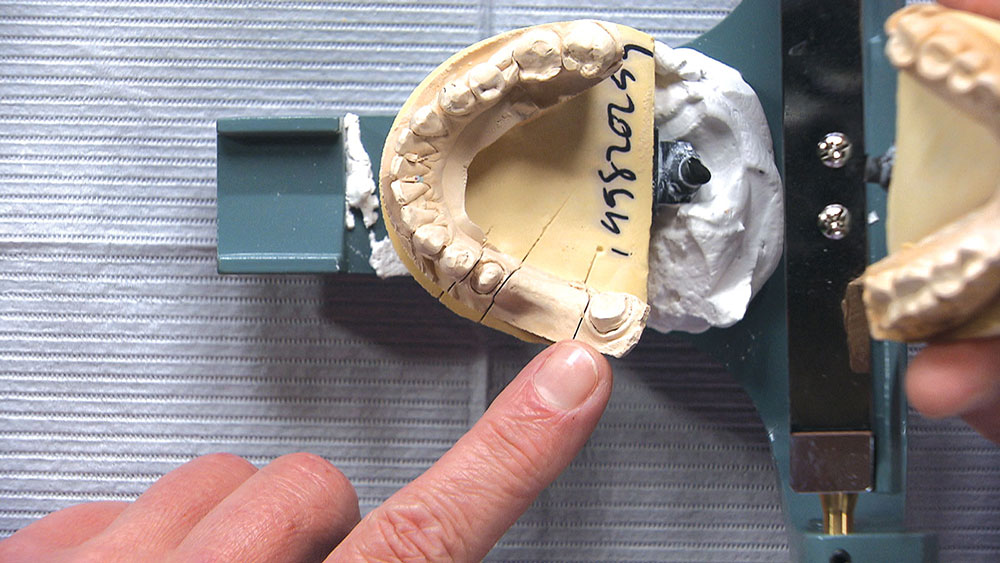
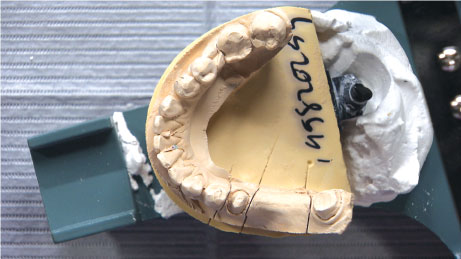
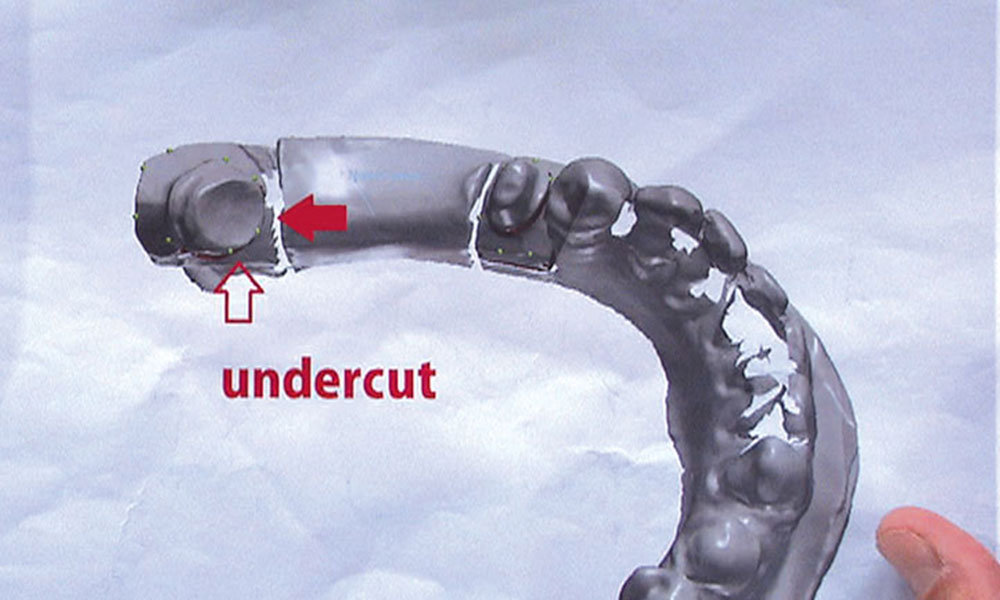
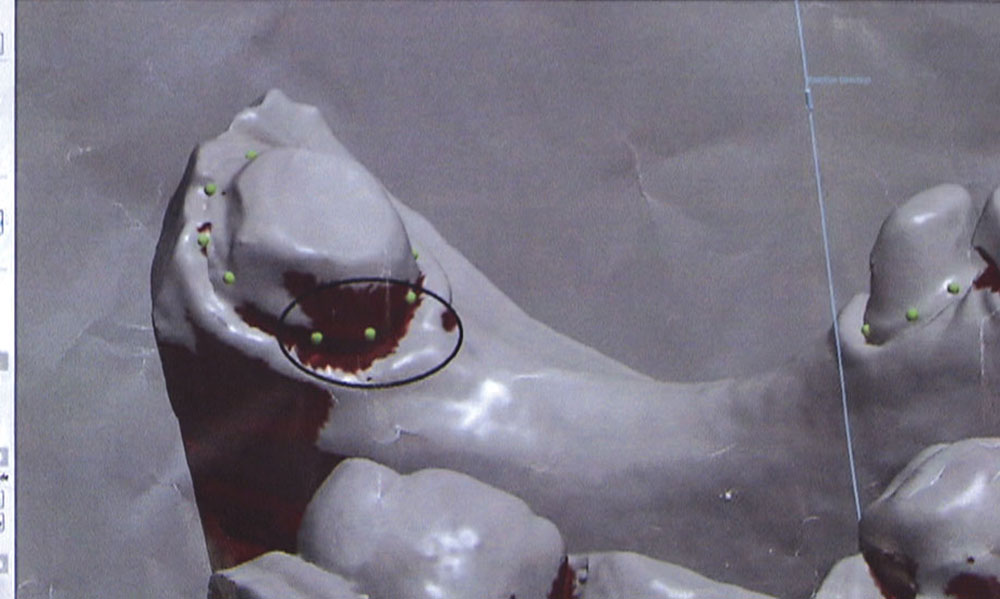
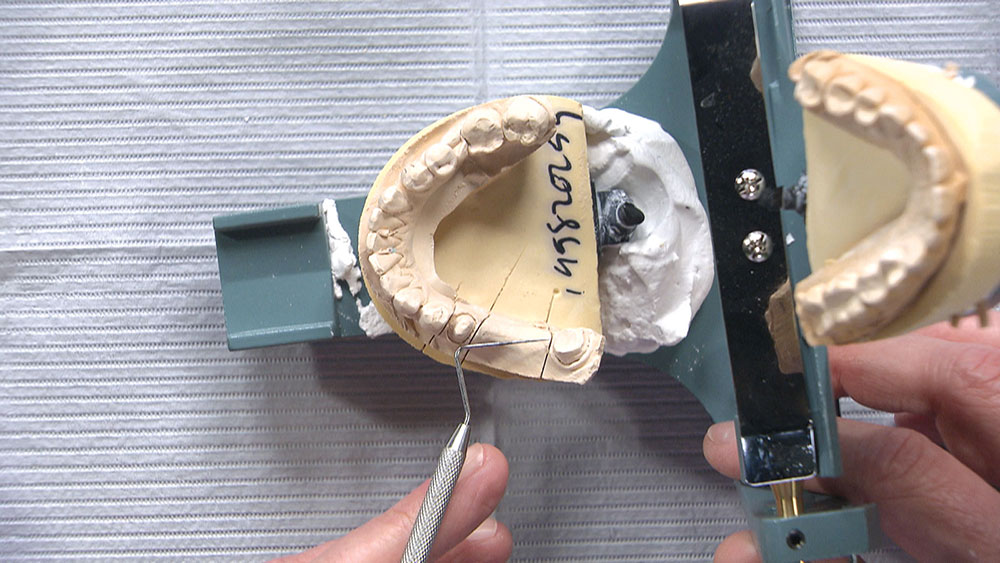
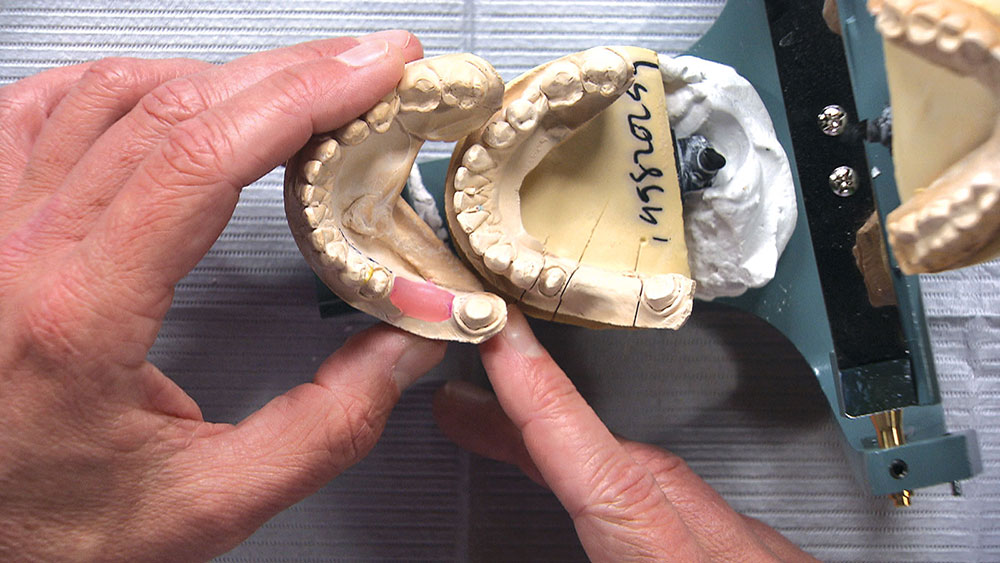
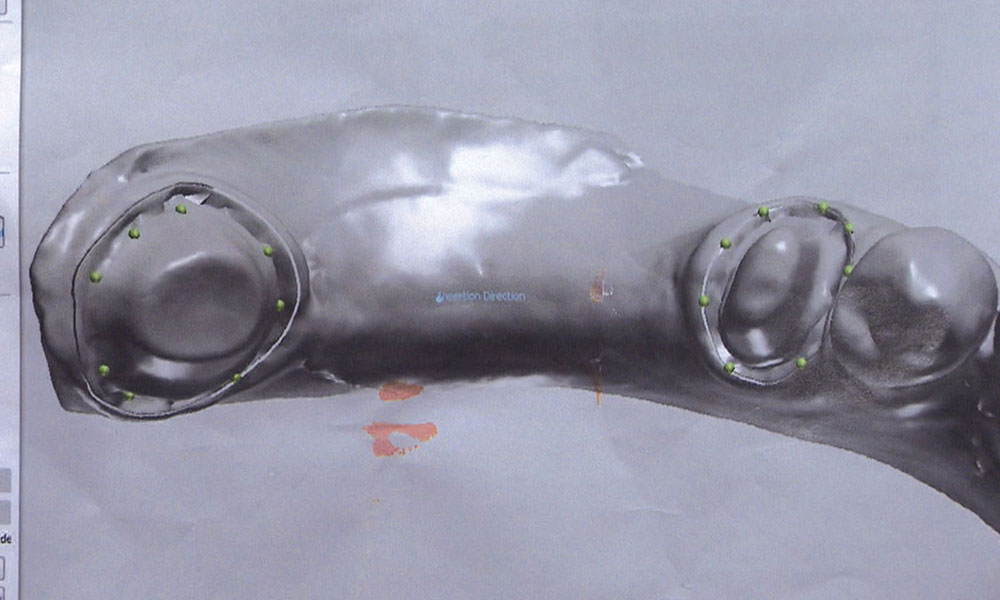
In this issue’s featured Case of the Week from Episode 58, I look at a case prepared by a dentist for a posterior BruxZir® bridge (Glidewell Laboratories; Newport Beach, Calif.). Even though the preps look really good, the path of insertion for the bridge is not ideal; in fact, one of the preps will require modification if the bridge has any chance of seating properly. The good news is we have a novel way at the lab of helping dentists accomplish a case like this. Let’s take a look at the case.
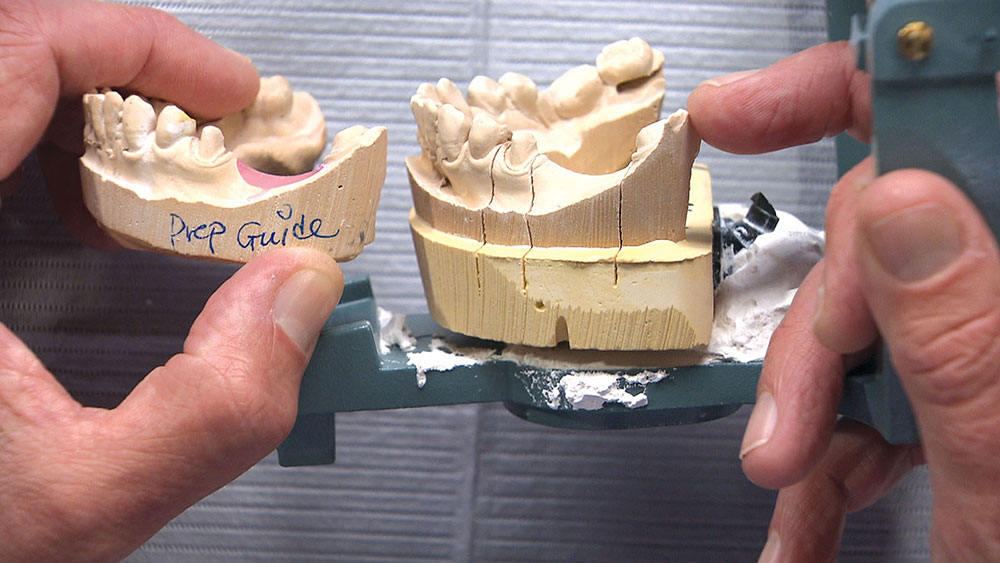
You’d be surprised how often we send doctors reduction copings and, for whatever reason, the necessary reduction is not done. I’m not sure if this is due to a lack of understanding about how to use a reduction coping, or if dentists think it’s only a suggestion.
Conclusion
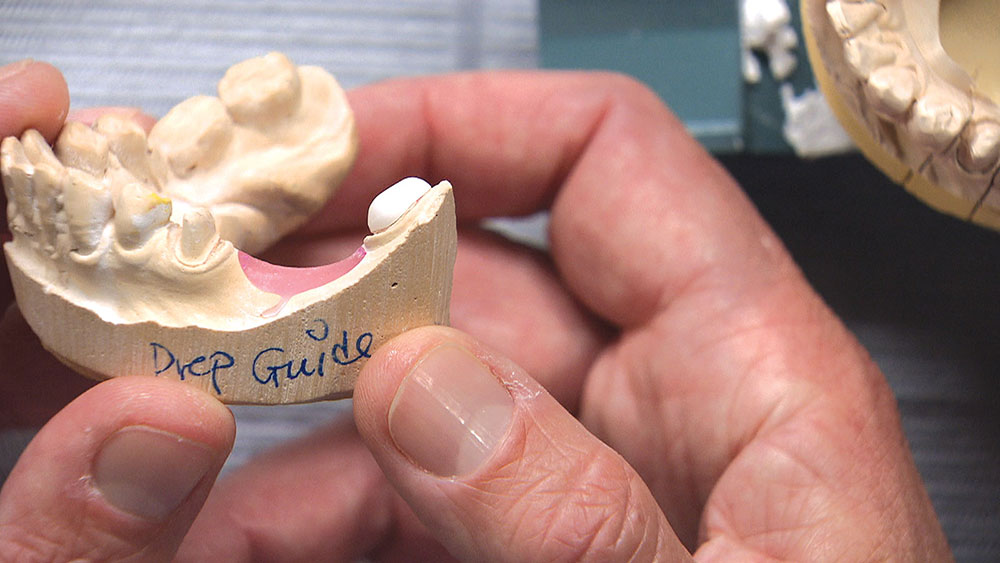
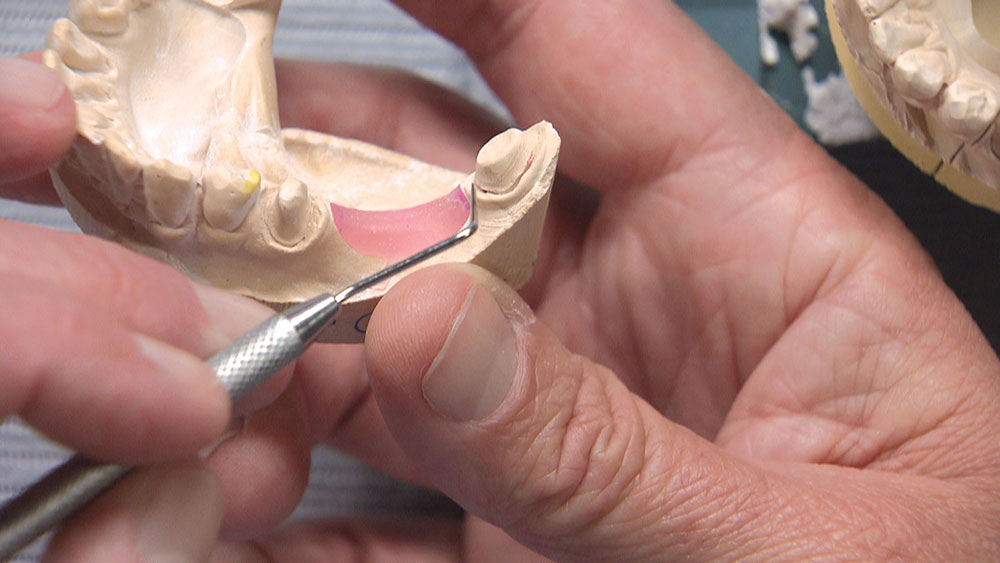
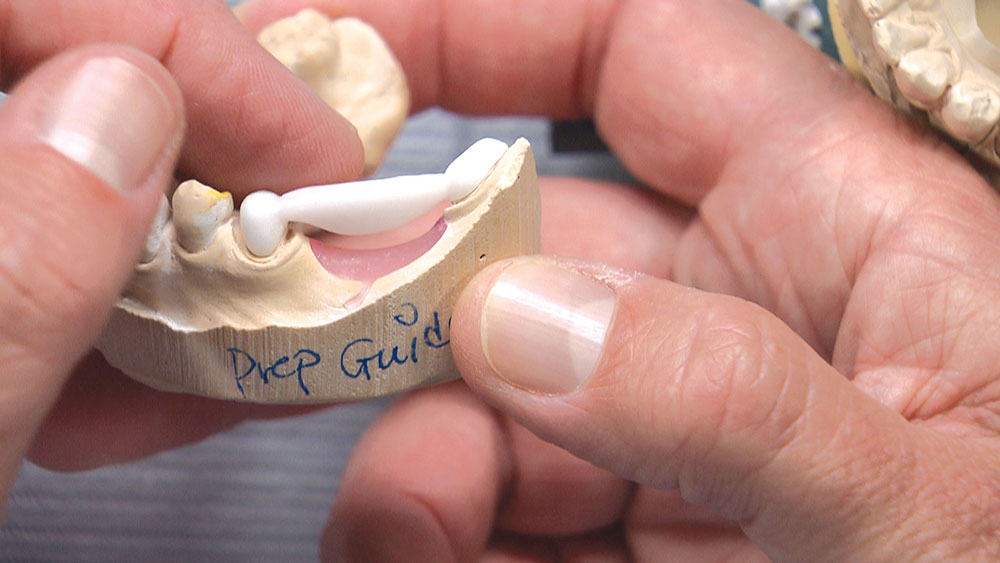
As the dentist, you have a few choices in a case like this. You could have the patient come back in for another appointment to reshape the molar so the bridge will fit; or, rather than reshaping the back tooth, you could propose placing two implants between the bicuspid and the molar and then two single-unit crowns — though getting the patient to agree to this might be a stretch. Alternately, you could have the lab make you the actual bridge and a prep guide at the same time. Then, before trying in the permanent bridge, you could adjust the mesial and mesial-lingual portions of the molar until the framework goes down in the mouth like it did on the prep guide. If there are no contact issues or occlusion problems, you know the bridge is all the way down and you have saved yourself and your patient a return appointment. For this third approach to be successful, however, you will need to anesthetize the patient and be committed to doing the necessary preparation to get the bridge seated all the way and in one piece — especially if you’re doing a zirconia bridge without any kind of attachment, stress-breaker or telescopic coping. Whether you want to schedule a separate appointment or try to seat the bridge using the prep guide, the lab is more than happy to guide you in achieving clinical success.