Photo Essay: Post-and-Core Technique with BioTemps® Provisionals
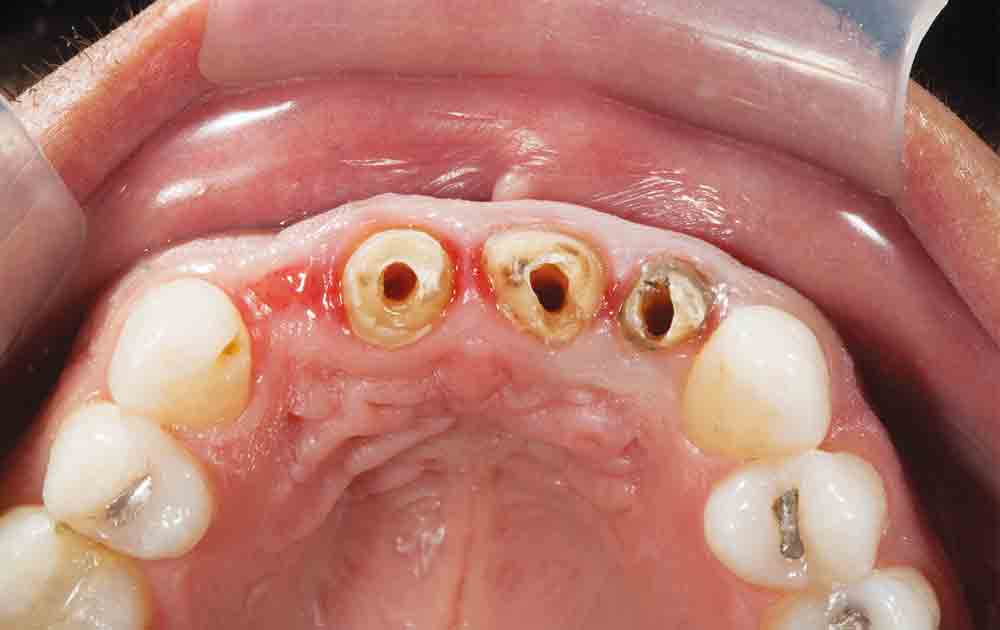
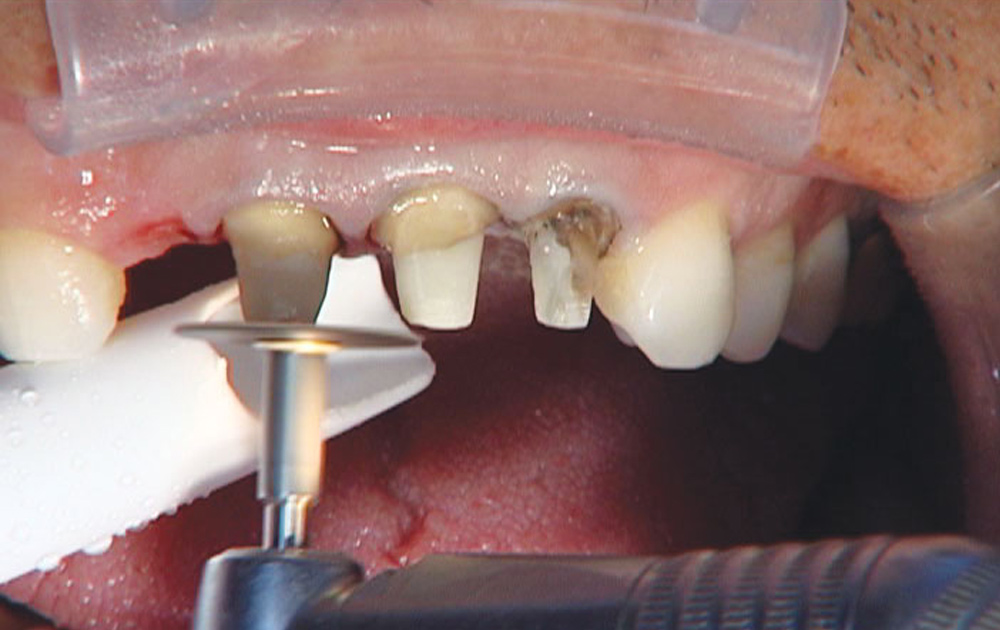
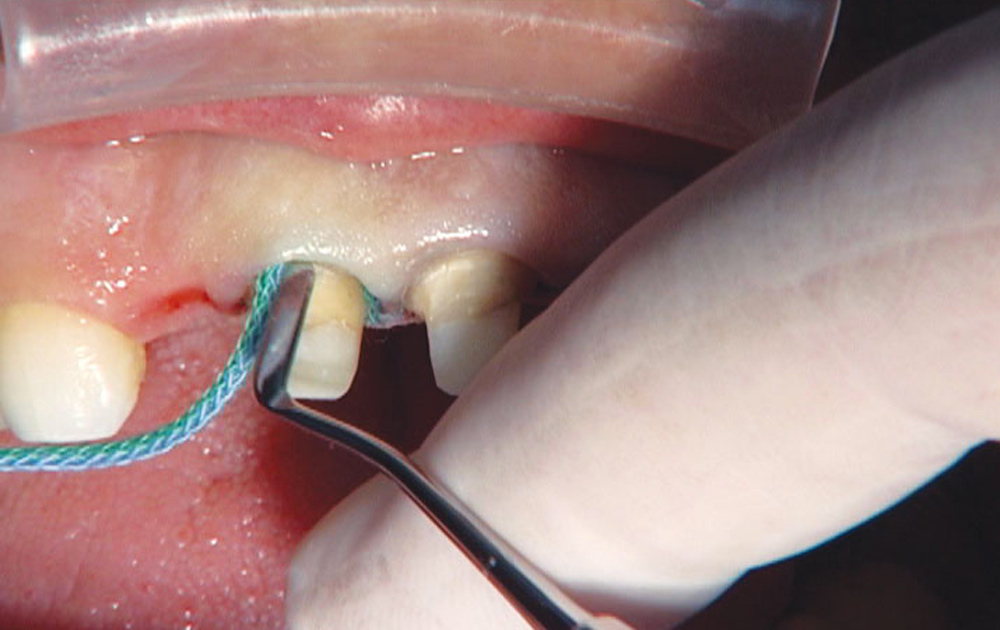
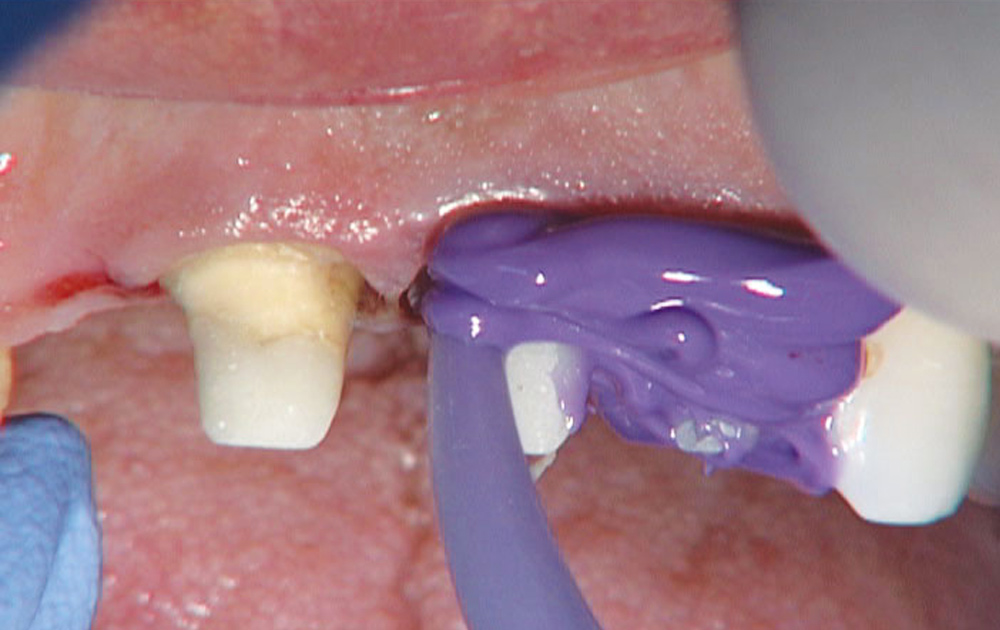
This was an interesting case because it took me away from the normal flow of procedures and forced me to think about the best way to accomplish the posts and cores for this 4-unit bridge. Because I would be doing posts and cores in conjunction with BioTemps® Provisionals (Glidewell Laboratories; Newport Beach, Calif.), I wanted to avoid having to toss the BioTemps in the trash and do chairside temps if I made the cores too large or they wouldn’t draw. I decided tooth #7 would be a cantilever pontic off of teeth #8 and #9, which would be two PFMs splinted together, and tooth #10 would be a single-unit PFM.