BioTemps® Tips and Tricks for Successful Seating – Case of the Week: Episode 66
This issue’s featured Case of the Week from Episode 66 of "Chairside Live" provides some useful clinical techniques to help you successfully seat your next large BioTemps® Provisionals (Glidewell Laboratories; Newport Beach, Calif.) case. A dentist who regularly prescribes BioTemps called me seeking advice about this particular case when he had trouble seating it at the end of the prep appointment. His difficulties reminded me of the frustrations I have experienced at times over the last 12 years when working with lab-fabricated provisionals. I am a big advocate of BioTemps, but there are some challenges to keep in mind when dealing with any type of indirect temporary restoration.
CONCLUSION
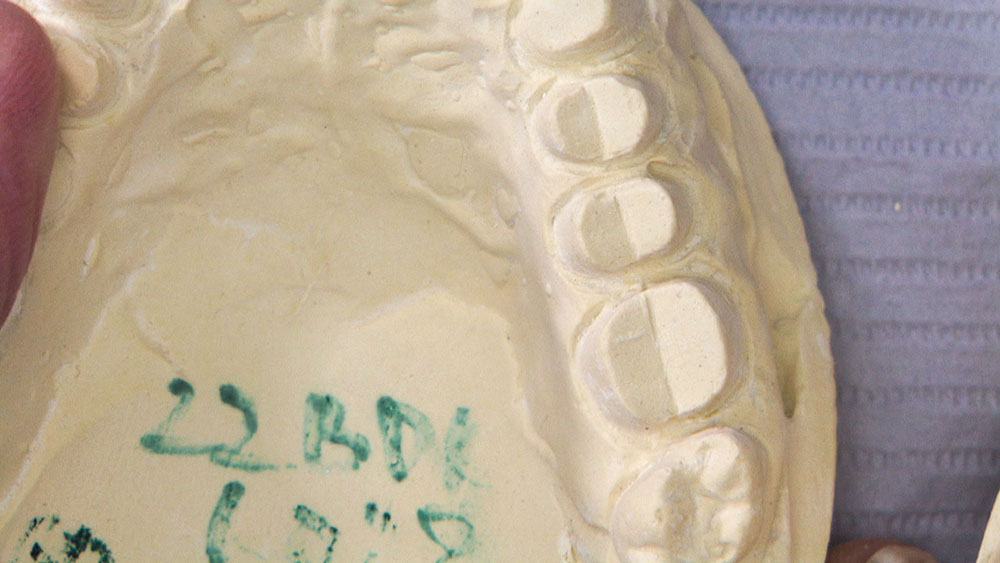
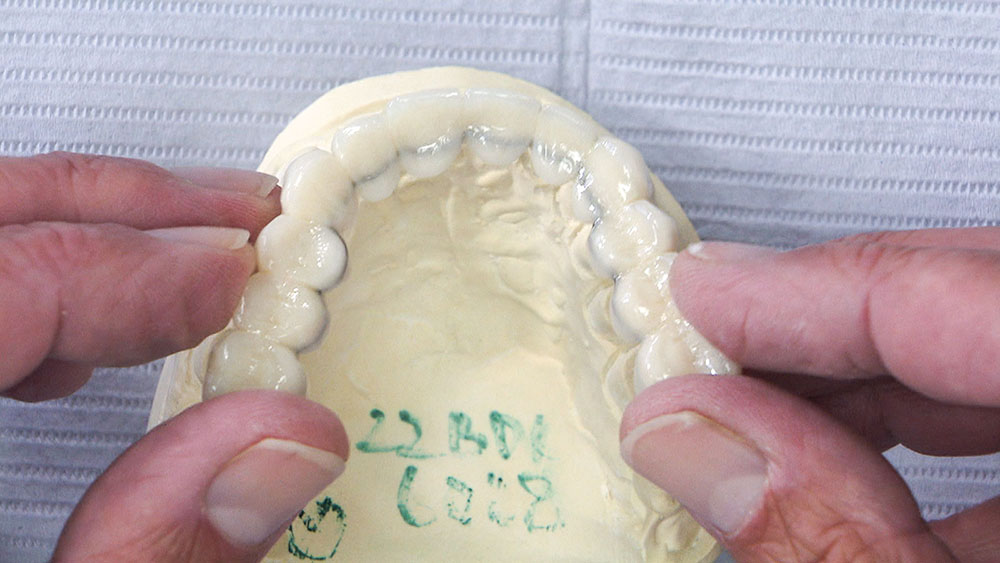
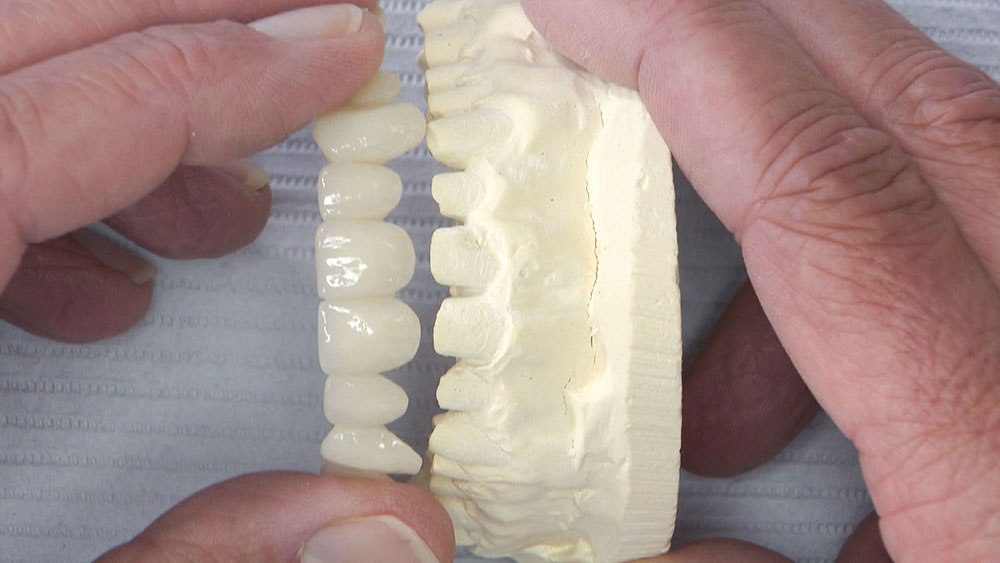
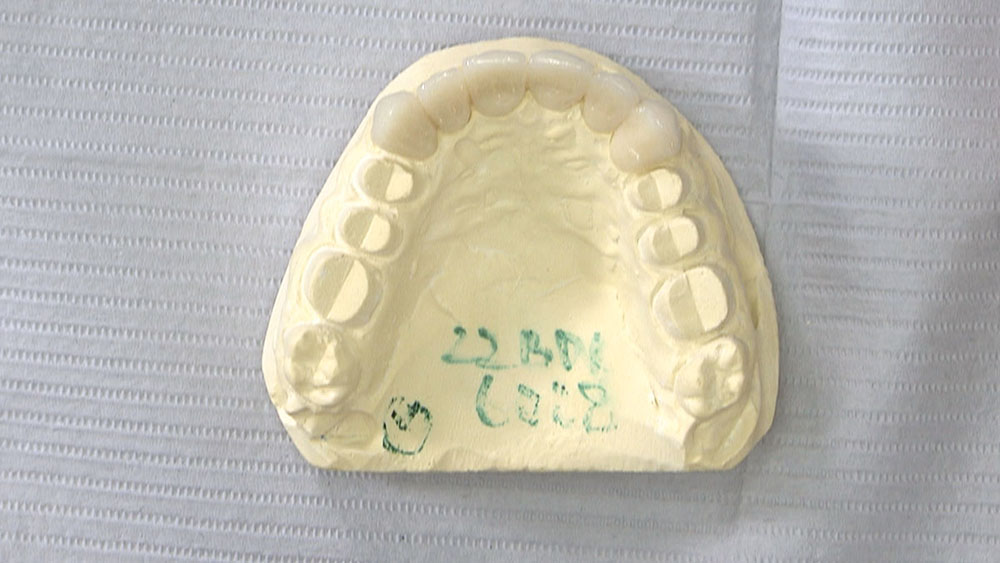
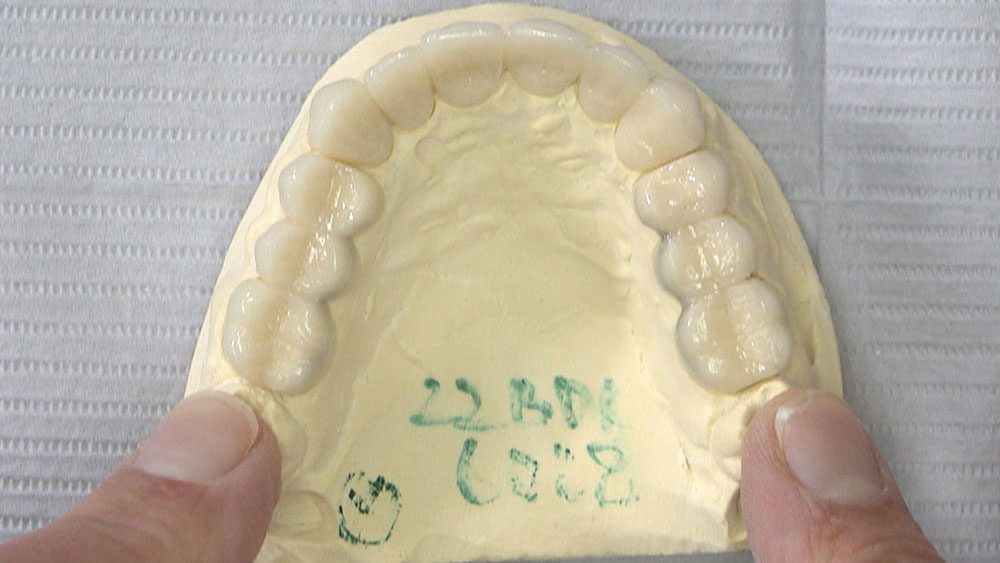
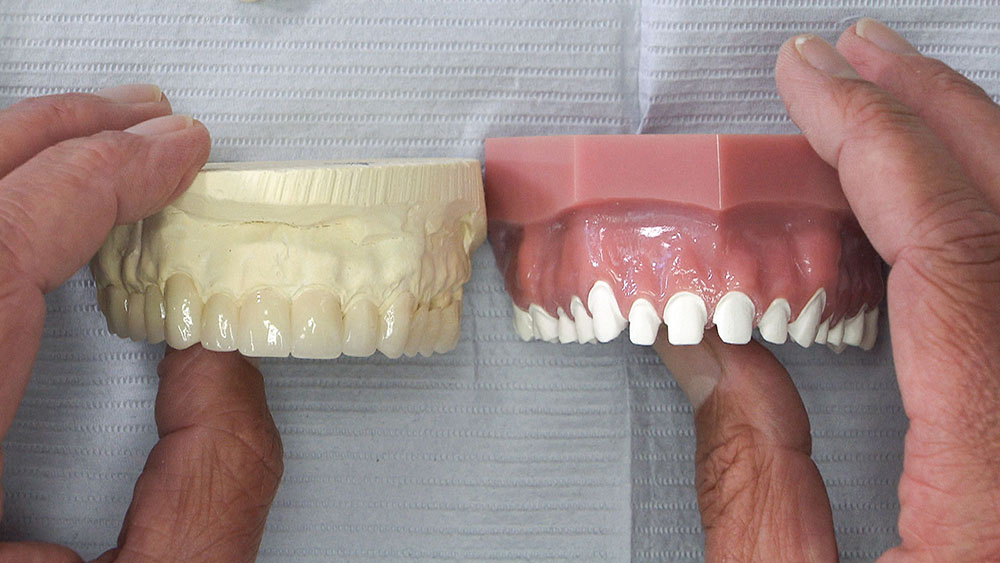
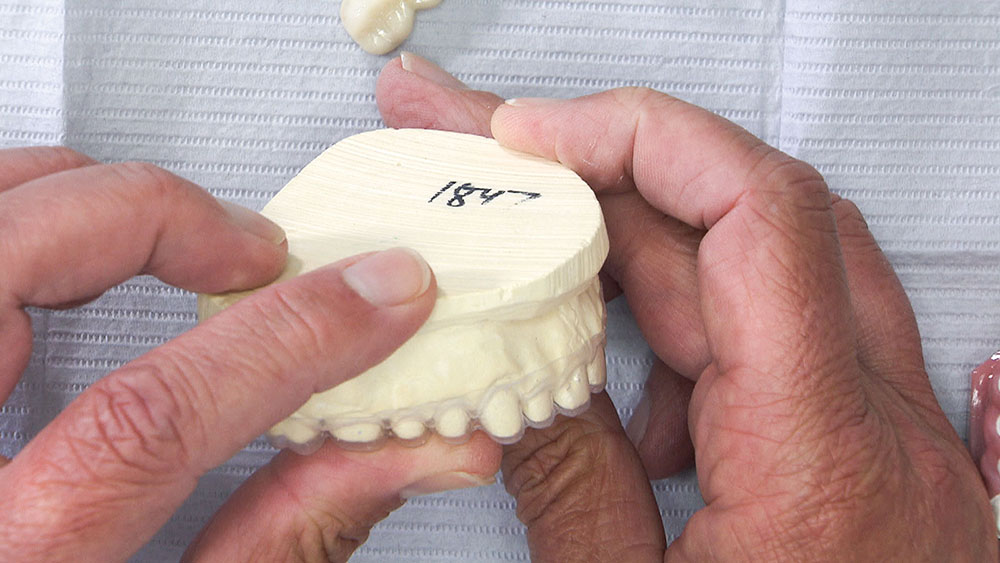
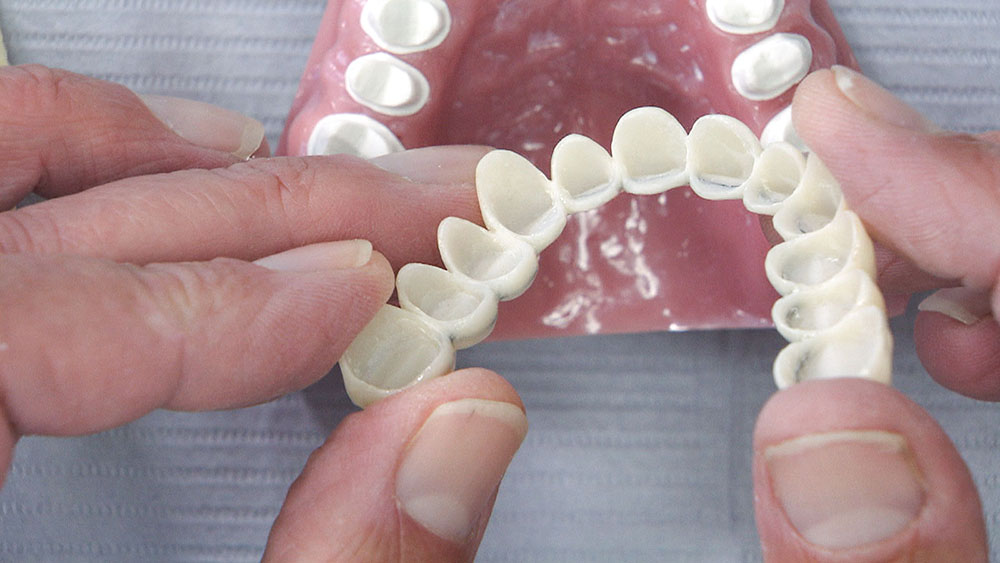
When seating a large BioTemps case, fit issues can occur because the dentist is prepping the patient for single units, but the BioTemps technician is prepping for a bridge that will draw. To avoid unnecessary frustration, I always recommend that dentists request the BioTemps be made in three segments. While this approach may seem like more of a hassle, I don’t think you’ll have any issue doing one posterior segment first, the other posterior segment next, and then prepping the anterior segment. Yes, sometimes you’ll have to adjust the contacts to get the BioTemps to seat completely; and because they have the tendency to rock faciolingually, you’ll want to be sure to have the patient bite together before you reline to avoid a Bucky Beaver look. (To counter this tendency, some dentists prefer to seat all three BioTemps segments at the same time using impression putty or the bailout splint and bis-acryl material.) But BioTemps Provisionals continue to be one of our best-selling products, and for good reason. These durable temporary restorations exhibit lifelike esthetics that rival natural teeth, allowing dentists to provide their patients with a beautiful smile as soon as they prepare their teeth. Our lab now also offers a "scan and save" program with the BioTemps product, where we digitally scan the BioTemps in the lab before sending them to you to try in the patient’s mouth. If you and your patient are pleased with how the BioTemps look at try-in, we can replicate their size, shape, length, contour and surface texture exactly in the final ceramic restorations using the stored digital data.
References
- Fondriest JF. Using provisional restorations to improve results in complex aesthetic restorative cases. Pract Proced Aesthet Dent. 2006 May;18(4):217-23.
- Zwetchkenbaum S, Weiner S, Dastane A, Vaidyanathan TK. Effects of relining on long-term marginal stability of provisional crowns. J Prosthet Dent. 1995 Jun;73(6):525-9.
- Bevilacqua L, Biasotto M, Cadenaro M, Di Lenarda R, Dorigo E. Reaction exothermia of 2 relining resins for temporary crowns. Minerva Stomatol. 2005 Jan-Feb;54(1-2):35-41.
- Roe P, Patel RD. Fabrication of a modified repositioning key for relining provisional restorations. J Prosthet Dent. 2010 Dec;104(6):401-2.