Tooth in a Bag: Same-Day Monolithic Zirconia Crown
INTRODUCTION
The goal of every efficient practice is to provide the most durable restorations possible, while exceeding the minimum esthetic needs of the patient. Newer materials and techniques make this easier than ever before.1,2
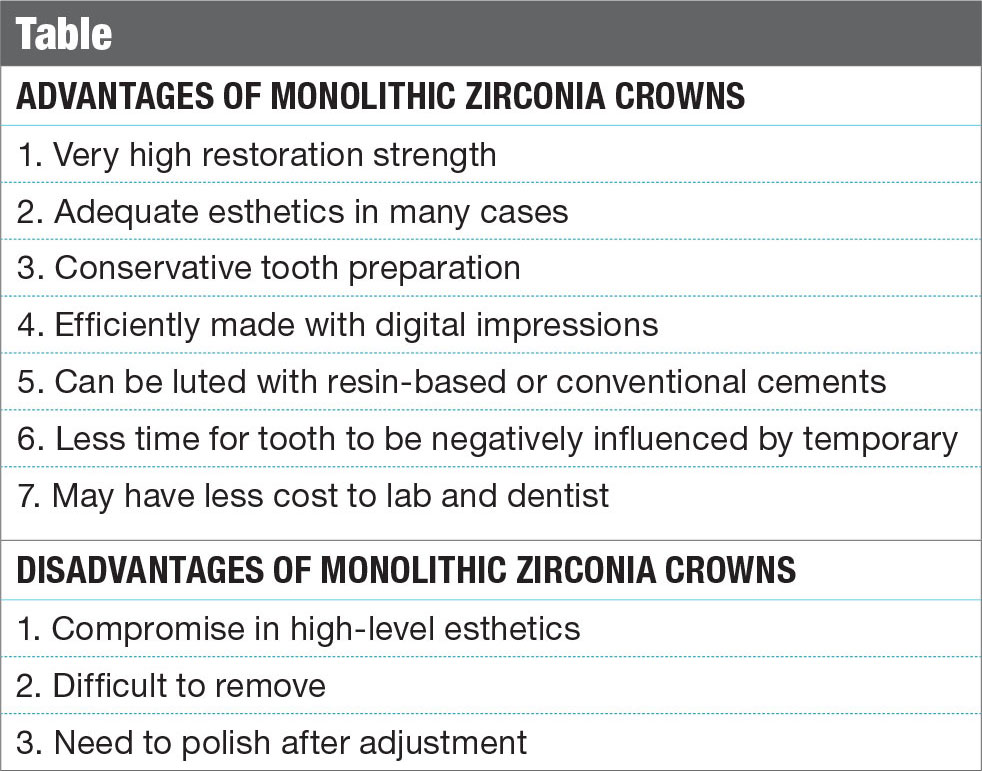
Full-contour (monolithic) zirconia crowns have become popular in the last few years because of their impressive flexural strength (1,000+ MPa), tooth color, minimal wear on opposing teeth, conservative tooth preparation and potential for excellent long-term clinical success.3,4
Monolithic yttria-stabilized tetragonal polycrystalline zirconia has become very widely used in the last few years because of its durability, excellent fit and improved esthetics (Table). Without a layering porcelain, the clinical performance has been excellent, as long as tooth preparation is adequate, and the dental laboratory and clinical materials are handled in the correct manner.5,6 Porcelain can be pressed or stacked to the surface of zirconia to improve esthetics, but this add-on material has had a history of chippage, breakage and delamination, resulting in compromised restorations. Whether layering porcelain to metal, lithium disilicate or zirconia, the weak link of the restoration is the relative weak bond of the layering porcelain to the underlying substrate (coping). This junction is where the potential for failure is highest.7,8,9,10 In those cases where the cosmetic demand can be met without layering porcelain, the potential exists for monolithic restorations to outperform those with esthetic-enhancing porcelain additions.11,12 The mantra of this clinician is to use the strongest material available that meets the minimum cosmetic needs of the patient.
Monolithic zirconia posterior crowns have the potential to outlast layered restorations such as the PFM because there is no porcelain to delaminate, chip or fracture. In very esthetically demanding situations, the practitioner must choose a material to meet the cosmetic desires of the patient. If the patient is unhappy with the appearance, it often does not matter how durable the material is.
Indications for Monolithic Zirconia Crowns
Dentists are often hesitant to change materials and techniques because of familiarity with their current methods, even if the success can be improved upon.13,14 That fear of change is often justified, particularly if there is no perceived problem with the current system or materials. New materials and techniques should be met with cautious skepticism, and the balance among clinical performance, office efficiency and scientific studies should guide our decisions for improvement.15 The quest for materials with higher esthetics or less failure, like the delamination or breakage of layering porcelain on a PFM crown, has driven us to evaluate materials like lithium disilicate and zirconia.16 With the wide variety of restorative materials today, choice of restoration material relies on the experience of the practitioner coupled with the prevailing dental education and research. Esthetic materials such as pressed ceramics, PFMs and reinforced porcelains have shown varying degrees of success depending upon the clinical indications and dental team protocol.17
Gold has a long-standing functional predictability that has not been matched by any current esthetic material. PFM crowns have dominated the dental market for many years and, despite their cosmetic shortcomings and porcelain failures, their versatility is undeniable. Lithium disilicate is a newer material and, in its monolithic form, has proven dependable.18 So at what point would it be prudent for the clinician to consider full-contour zirconia restorations? For those patients who have compromised occlusal schemes, parafunctional habits, or a history of restoration fracture, monolithic zirconia crowns may be indicated.19 Opacity of zirconia today has lessened, and overall esthetics have certainly improved over the last few years, allowing monolithic zirconia to meet the cosmetic needs of many posterior restorations.
CASE REPORT
The patient presented with a broken cusp or fractured restoration for the third time in three years. Tooth #19 had the distobuccal cusp fractured off, with a moderately sized composite resin restoration that was also fractured (Fig. 1). There was slight pain upon biting pressure, but no signs or symptoms that indicated irreversible pulpitis. The patient had been wearing a bite splint for years to control the adverse effects of clenching (Fig. 2).
The treatment plan was for a full-contour zirconia crown to address the patient’s esthetic goals and concerns about the restoration’s longevity (Fig. 3).
Tooth Preparation
For a predictable and dependable restorative outcome, proper tooth preparation that also complements the chosen dental material must be done.20,21 With monolithic zirconia, a preparation can be done with reduction very similar to that of full-gold restorations.22,23,24 A more conservative preparation can be done for monolithic materials than for PFMs or other layered porcelain restorations because reduction need only compensate for the core.24 An occlusal clearance of 1.0 to 1.5 mm is recommended, so a 330 bur (NeoBurr® #330 [Microcopy; Kennesaw, Ga.]) was used to make 1.5 mm occlusal depth grooves and the interproximal slices (Fig. 4). (Note: The usual length of the actual cutting portion of a 330 bur is approximately 1.5 mm, depending on the manufacturer. It is recommended that this be confirmed via measurement before using this bur in your office as a depth cutter.)
A chamfer margin with axial wall reduction of 1.0 mm is ideal for this material (Fig. 5). Feather-edge margins are acceptable depending upon the laboratory team’s skill, but the potential for restoration over-contouring and error in margin identification is greater compared to margins easily seen by whatever impression technique might be used. A preparation done with a 5-to-10-degree taper and easily identifiable margins can make fabrication, cementation and restorative longevity more predictable. A tapered diamond bur (NeoDiamond® #1116.8C [Microcopy]) was used for axial reduction and margin formation in the case highlighted here (Fig. 6).
Despite the ability of zirconia to be resin-cemented (bonded) to the tooth, the tapering of the opposing preparation walls, the surface area of the prep, and the height of the walls all are critical to long-term restoration retention and success. Zirconia bonding cannot be counted on to compensate for preparations designed with walls of excessive taper (more than 10 degrees) or those with very short axial walls (less than 3 mm). If these parameters are not heeded, the practitioner may experience more restoration debonding/cementing failures. A football-shaped diamond bur (NeoDiamond #1523C [Microcopy]) was used to complete the occlusal reduction. The reduction was then verified with the patient in centric occlusion (Fig. 7).
Digital Impressions
Because zirconia crowns are milled with CAD/CAM technology, their use is highly efficient if paired with digital impressions. The preparation and adjacent teeth were sprayed with an optically reflective powder (Fig. 8), and an image was then acquired with a digital impression system (CEREC® Bluecam [Sirona Dental Systems; Charlotte, N.C.]). The reflective powder improves image capture, particularly if tooth structure is more translucent. The opposing arch was also powdered (Fig. 9) and digitally captured. Next, the patient was asked to close into "normal bite on the back teeth" (maximum intercuspation) (Fig. 10), and another digital image was captured from the buccal. In our hands, after doing hundreds of restorations with this impression technique, we have had superior results with less restoration adjustments than any other indirect technique, including full-arch or quadrant trays with any of the currently popular "physical" impression materials.
Immediately after the digital images were captured, the assistant cleaned the powder off of the preparations (and opposing teeth) with an air water spray. This was followed by scrubbing the preps with the brush tip of a Dento-Infusor® syringe (Ultradent; South Jordan, Utah) and ViscoStat® Clear (Ultradent) containing a 25% aluminum chloride gel. This technique allows for the mechanical removal of the contrasting powder and acts to wet the tooth and to reduce unwanted fluid seepage from the gingiva (Fig. 11).
Provisionalization
When provisional restorations are made, care must be taken with the choice of transitional cements if dentin resin bonding is to be done during the final luting process. With various dentin-bonding systems, certain cements have been shown to decrease bond strength values considerably.25 For patients who are not scheduled to return the next day, a temporary may be made, but a noneugenol temporary cement is warranted because of the potential for interference of the definitive resin cement bond to the dentin.26,27 For only a few hours or days, the temporary is often "cemented" with a lining of polyvinyl wash impression material. That provides adequate short-term retention, easy cleanup and no negative effects that the temporary cement may have on definitive cementation. For those offices that have no agreement with a dental laboratory for fast turnaround, or for less-than-dependable patients who may not return promptly, it is advisable to make a traditional provisional restoration and lute it with a noneugenol temporary cement.
Digital Dentistry and Efficiency
Zirconia crowns are laboratory-fabricated CAD/CAM restorations that are made either from a digital impression or from a conventional impression that is poured up and then digitized. This latter method can introduce traditional errors into the system via inaccuracies and distortions in the impression material, inaccurate model-making and improper die-trimming. Digital impressions bypass all of these potentially error-laden steps, and increase efficiency by decreasing time, cost and materials used.
The CEREC Bluecam, PLANMECA PlanScan™ (E4D Technologies; Richardson, Texas) and the Lava™ C.O.S. (3M™ ESPE™; St. Paul, Minn.) are a few of the growing number of digital systems that are being used to capture digital dental impressions. A tremendous advantage is to be able to send a digital impression over the internet, and then have the laboratory team design the restoration, mill it and customize it in a very short period of time. Because contacts and occlusion are done in the design software on the computer, models are not needed, and the fabrication time in the lab is less than two hours when no layering porcelain is done.
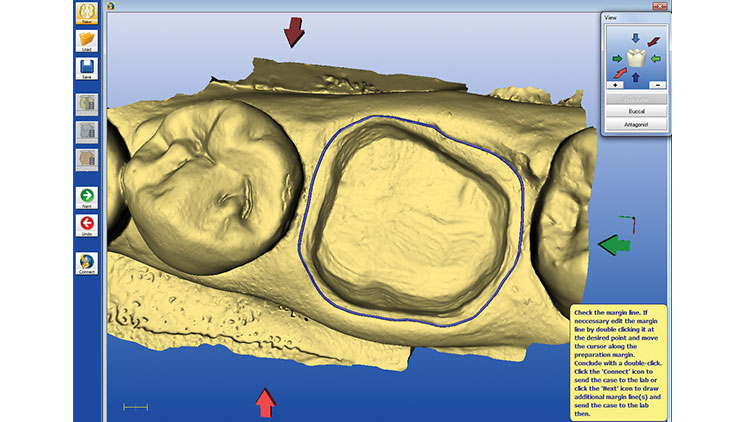
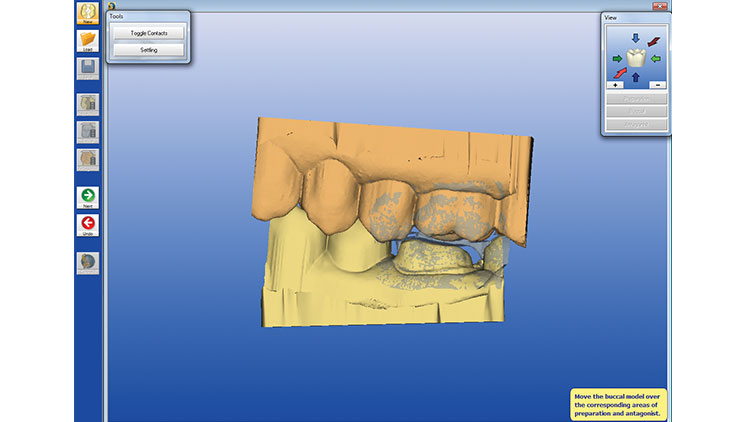
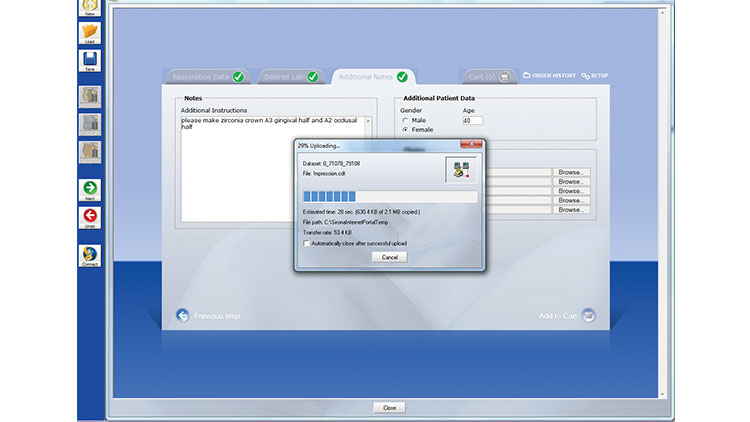
The chairside assistant (or the doctor) draws the margin in the software and validates the occlusion (Figs. 12, 13). Next, the digital images are sent via the internet (CEREC Connect [Sirona Dental Systems]) to the dental laboratory team, where the design is finalized and the restoration is then completed (Fig. 14). (Note: A confirmation is sent to the doctor that the laboratory team has received the case. In addition, the doctor should call the lab team to ensure completion of the case and to verify the time of return to the office.)
It is important to have a good relationship and to establish excellent communication with the laboratory team. The lab team must understand how the dentist wants the nuances of the restoration to be. Factors such as characterization, emergence profile, occlusal detail and esthetic characteristics should be worked out in advance, or explained when the case is uploaded.
Furthermore, along with a shift in philosophy for the dentist doing digital dentistry with zirconia crowns, the laboratory team must do things a bit differently as well. Total time in the laboratory (including design, custom staining and baking) is less than two hours. Digital impressions and the lack of a need for stone models cut lab fabrication time down greatly, with no reason for a case to sit on a shelf somewhere for two weeks to do a procedure that takes such little time. The "waiting" time in the lab is only for finalizing the design, cutting the sprue off after milling, application of stain if needed, and final firing of the case in the oven. With no models to pour, nothing to mount, no stacking or pressing of porcelain, and no polishing, the lab owner has a very limited time commitment required from his or her technician team. Even a nonlocal lab can overnight the case and have it back to the dentist in less than 48 hours. This reduces the patient’s time in the provisional restoration, along with any possible time-related negative effects such as microleakage, tooth movement and occlusion changes.
Digital impressions bypass all of these potentially error-laden steps, and increase efficiency by decreasing time, cost and materials used.
Tooth in a Bag: "No-Modelaphobia"
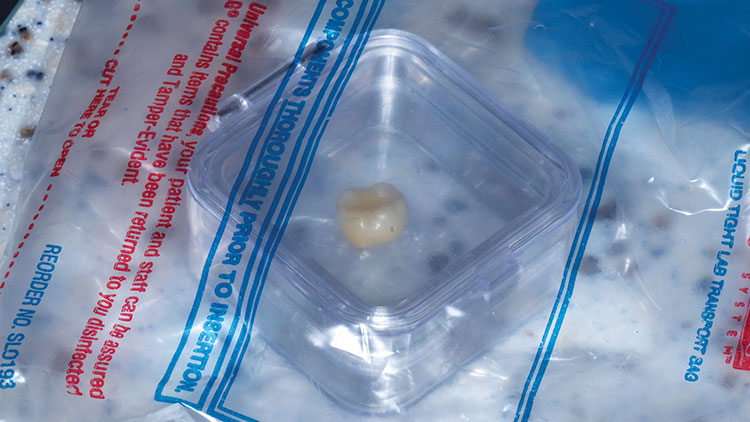
It is certainly a change to receive a restoration with no models to hold! "No-modelaphobia" is hard to overcome until one trusts the system. For those who can’t go on the proverbial "model wagon," laser-contoured models may be ordered by most labs for an additional fee (and taking several days). The negative effects of the additional time in the temporary far exceed the benefits of checking the restoration on the model.28 The accuracy of the system is undeniable, as long as proper tooth preparation and accurate imaging are accomplished.29,30,31
The next morning, the monolithic zirconia crown (BruxZir® Solid Zirconia [Glidewell Laboratories; Newport Beach, Calif.]) was returned in a jewel case in a bag (Fig. 15). About the only thing that could be examined while in the bag was the shade (Fig. 16).
Cementation Considerations
The cementation of any restoration is either adhesive or nonadhesive. A major clinical advantage of zirconia is that it can be either conventionally cemented or resin-bonded into place. The determining factor should be the resistance form of the preparation and the anticipated occlusal forces.32,33 When preparations are short, overly-tapered, or if occlusal forces are heavy, bonding with a resin cement is indicated. In these situations, resin cements provide maximum restoration retention, microleakage prevention and increased fracture/fatigue resistance of the restorative material itself.34,35 Bonding involves more meticulous attention to detail, such as isolation, dentin preparation and cleanup, than traditional luting materials such as a glass ionomer or zinc phosphate.
Nonadhesive cementation is a viable option if the amount of surface area and degree of divergence of the prepared walls can provide sufficient micromechanical retention. Resin-reinforced glass ionomer cements like RelyX™ Luting (3M ESPE) or GC Fuji Plus™ (GC America; Alsip, Ill.), and newer bioactive cements such as Ceramir® (Doxa Dental Inc.; Newport Beach, Calif.) have been popular choices because of lower reported sensitivity, ease of use, and long-term clinical success on retentive preparations.34,36
The most efficient cementation would be the one that bonds well to enamel, dentin and substrates like zirconia.37 Because of the higher opacity of most zirconia products today, there is little influence of the cement on final restoration color, as long as the margins are not in an esthetically critical zone.
Using a Bioactive Cement
For this case, we chose to use a hybrid calcium aluminate/glass ionomer cement (Ceramir). Studies have shown that Ceramir has performed very well in clinical situations after several years with extremely low patient sensitivity.38 It is intended for the definitive cementation of crowns and fixed partial dentures, gold inlays and onlays, prefabricated metal and cast dowel and cores, and all-zirconia or all-alumina crowns. The cement is a water-based composition comprised of calcium aluminate and glass ionomer components, and has been demonstrated to be bioactive in that it stimulates the formation of hydroxyapatite in in-vitro testing.39
The tooth was wiped with a 2×2 gauze, and then the fit of the restoration was verified on the tooth. The cement was triturated (a creamy, almost mousse-like consistency) and was loaded into the crown (Fig. 17). After the tooth was again slightly dried with 2×2 gauze, the crown was seated into place, and the patient was asked to hold "slight" biting pressure on a cotton roll (Fig. 18). Cleanup began about one to two minutes later. Unlike the difficult cleanup often associated with bonded resin cements, this bioactive cement peels off easily in a rubbery, gel-like (firm) state, making its removal easier than most other cements (Fig. 19). The occlusion was checked at about five minutes (Fig. 20), and adjustments were done with a finishing diamond bur (Gold Diamond 392-018-8 F [Diatech; Charleston, S.C.]) attached to a high-speed handpiece with water and light pressure. (Note: Adjustments are rare in our office when digital impressions are used if the lab team follows proper fabrication parameters, and if the restoration is placed within 48 hours.) Finally, polishing was completed with a rubber porcelain polishing system (Jazz® Porcelain Polishers [SS White Burs, Inc.; Lakewood, N.J.]) (Figs. 21, 22).
As zirconium oxides are used more with time, it may be prudent to have a few burs designed for more aggressive zirconia recontouring, complete removal, or endodontic access (e.g., Great White® Z Diamond burs [SS White Burs, Inc.]). These diamonds come in various sizes, and make gross zirconia removal much faster with less stress on the handpieces, doctor and crown itself.
CLOSING COMMENTS
There is no doubt that speculation will exist on several levels. First, as great as the apprehension probably was for those who were encouraged to leave their copper band impressions behind when everyone went to vinyl polysiloxane quadrant impressions, there is fear of the unknown when taking the plunge into digital impressions. There is probably still an excellent clinician taking plaster impressions or using a dip tank for developing bitewings. One should not encourage change just for change’s sake, but instead for bettering patient service and clinical outcomes.
Convincing a dental technician to agree to start work on a crown within hours of receiving the digital file and returning it the next day will also be a challenge for some who have the habit of setting a case in a bin on a shelf for days before action. Without the need for layering porcelain, the fee charged by the lab may even be less because of a reduction in technician time. Some clinicians may suffer withdrawal when forced to give up their models, articulators or pindexed plaster (PINDEX® System [Coltène/Whaledent Inc.; Cuyahoga Falls, Ohio]). Even considering having a patient walk out of the office without a temporary will be outright heresy to some.
Nonlayered tooth-colored crowns, digital impressions, no models, single-day lab fabrication, and bioactive cements may one day become the standard in dentistry; it has in this office. The rewards gained by having very accurate restorations that are extremely convenient and comfortable for the patient, all while keeping the office overhead low, far outweigh the stress associated with change.
ACKNOWLEDGMENT
Dr. Griffin would like to thank Dan Becker, CDT, at Becker Dental Lab (beckerdentallab.com) in Herculaneum, Missouri, for his fine work and commitment to current trends in dentistry.
References
- ^Christensen GJ. The ceramic crown dilemma. J Am Dent Assoc. 2010 Aug;141(8):1019-22.
- ^Rosentritt M, Ries S, Kolbeck C, et al. Fracture characteristics of anterior resin-bonded zirconia-fixed partial dentures. Clin Oral Investig. 2009 Dec;13(4):453-7.
- ^Quinn JB, Cheng D, Rusin R, et al. Fractographic analysis and material properties of a dental zirconia. Poster presented at: IADR/AADR/CADR 83rd General Session; March 10, 2005; Baltimore, MD. Abstract 0560.
- ^BruxZir and milled IPS e.max CAD: very promising 1-year results. Clinicians Report. 2012 Jun;5:1-2.
- ^Larsson C. Zirconium dioxide based dental restorations. Studies on clinical performance and fracture behaviour. Swed Dent J Suppl. 2011;(213):9-84.
- ^Quinn GD, Studart AR, Hebert C, et al. Fatigue of zirconia and dental bridge geometry: Design implications. Dent Mater. 2010 Dec;26(12):1133-6.
- ^Donovan TE. Factors essential for successful all-ceramic restorations. J Am Dent Assoc. 2008 Sep;139 Suppl:14S-18S.
- ^White SN, Miklus VG, McLaren EA, et al. Flexural strength of a layered zirconia and porcelain dental all-ceramic system. J Prosthet Dent. 2005 Aug;94(2):125-31.
- ^Beuer F, Stimmelmayr M, Gernet W, et al. Prospective study of zirconia-based restorations: 3-year clinical results. Quintessence Int. 2010 Sep;41(8):631-7.
- ^Guess PC, Zavanelli RA, Silva NR, et al. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010 Sep-Oct;23(5):434-42.
- ^Ishibe M, Raigrodski AJ, Flinn BD, et al. Shear bond strengths of pressed and layered veneering ceramics to high-noble alloy and zirconia cores. J Prosthet Dent. 2011 Jul;106(1):29-37.
- ^Ozkurt Z, Kazazoglu E, Unal A. In vitro evaluation of shear bond strength of veneering ceramics to zirconia. Dent Mater J. 2010 Mar;29(2):138-46.
- ^Burke FJ, Ali A, Palin WM. Zirconia-based all-ceramic crowns and bridges: three case reports. Dent Update. 2006 Sep;33(7):401-2, 405-6, 409-10.
- ^Kugel G, Perry RD, Aboushala A. Restoring anterior maxillary dentition using alumina- and zirconia-based CAD/CAM restorations. Compend Contin Educ Dent. 2003 Aug;24(8):569-76.
- ^Rekow ED, Silva NR, Coelho PG, et al. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011 Aug;90(8):937-52.
- ^Christensen RP, Ploeger BJ. A clinical comparison of zirconia, metal and alumina fixed-prosthesis frameworks veneered with layered or pressed ceramic: a three-year report. J Am Dent Assoc. 2010 Nov;141(11):1317-29.
- ^Donovan TE. Porcelain-fused-to-metal (PFM) alternatives. J Esthet Restor Dent. 2009;21(1):4-6.
- ^Silva NR, Thompson VP, Valverde GB, et al. Comparative reliability analyses of zirconium oxide and lithium disilicate restorations in vitro and in vivo. J Am Dent Assoc. 2011 Apr;142 Suppl 2:4S-9S.
- ^Wall JG, Cipra DL. Alternative crown systems. Is the metal-ceramic crown always the restoration of choice? Dent Clin North Am. 1992 Jul;36(3):765-82.
- ^Beuer F, Aggstaller H, Richter J, et al. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009 Mar;40(3):243-50.
- ^Abou-Madina MM, Özcan M, Abdelaziz KM. Influence of resin cements and aging on the fracture resistance of IPS e.max press posterior crowns. Int J Prosthodont. 2012 Jan-Feb;25(1):33-5.
- ^Baltzer A. All-ceramic single-tooth restorations: choosing the material to match the preparation—preparing the tooth to match the material. Int J Comput Dent. 2008;11(3-4):241-56.
- ^BruxZir preparation guide. Available at https://bruxzir.com/assets/downloads/scientific-clinical-compendium.pdf. Accessed November 8, 2012.
- ^Tooth preparation guidelines for zirconia crowns. The Dental Advisor. July 2009. Available at https://www.dentaladvisor.com/pdf-download/?pdf_url=publications/clinician-technique-guide/toothpreparation-gui-delines-for-zirconia-crowns.pdf. Accessed October 9, 2012.
- ^Paul SJ, Schärer P. Effect of provisional cements on the bond strength of various adhesive bonding systems on dentine. J Oral Rehabil. 1997 Jan;24(1):8-14.
- ^Meyerowitz JM, Rosen M, Cohen J, Becker BJ. The effect of eugenol containing and non-eugenol temporary cements on the resin-enamel bond. J Dent Assoc S Afr. 1994 Aug;49(8):389-92.
- ^Carvalho CN, de Oliveira Bauer JR, Loguercio AD, Reis A. Effect of ZOE temporary restoration on resin-dentin bond strength using different adhesive strategies. J Esthet Restor Dent. 2007;19(3):144-53.
- ^Ribeiro JC, Coelho PG, Janal MN, et al. The influence of temporary cements on dental adhesive systems for luting cementation. J Dent. 2011 Mar;39(3):255-62.
- ^Mayer T, Eickholz P. Microleakage of temporary restorations after thermocycling and mechanical loading. J Endod. 1997 May;23(5):320-2.
- ^Scotti R, Cardelli P, Baldissara P, Monaco C. Clinical fitting of CAD/CAM zirconia single crowns generated from digital intraoral impressions based on active wavefront sampling. J Dent. 2011 Oct 17. [Epub ahead of print]
- ^Ender A, Mehl A. Full arch scans: conventional versus digital impressions—an in-vitro study. Int J Comput Dent. 2011;14(1):11-21.
- ^Quinn F, Gratton DR, McConnell RJ. The performance of conventional, fixed bridgework, retained by partial coverage crowns. J Ir Dent Assoc. 1995;41(1):6-9.
- ^Foster LV. The relationship between failure and design in conventional bridgework from general dental practice. J Oral Rehabil. 1991 Nov;18(6):491-5.
- ^Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater. 2011 Jan;27(1):71-82.
- ^Dalby R, Ellakwa A, Millar B, Martin FE. Influence of immediate dentin sealing on the shear bond strength of pressed ceramic luted to dentin with self-etch resin cement. Int J Dent. 2012;2012:310702.
- ^Vargas MA, Bergeron C, Diaz-Arnold A. Cementing all-ceramic restorations: recommendations for success. J Am Dent Assoc. 2011 Apr;142 Suppl 2:20S-4S.
- ^Jefferies SR, Pameijer CH, Appleby DC, et al. Prospective observation of a new bioactive luting cement: 2-year follow-up. J Prosthodont. 2012 Jan;21(1):33-41.
- ^Jefferies SR, Appleby D, Boston D, et al. Clinical performance of a bioactive dental luting cement—a prospective clinical pilot study. J Clin Dent. 2009;20:231-7.
- ^Lööf J, Svahn F, Jarmar T, et al. A comparative study of the bioactivity of three materials for dental applications. Dent Mater. 2008 May;24(5):653-9.
Reprinted by permission of Dentistry Today, ©2013 Dentistry Today.