Photo Essay: Treatment Planning After Facial Trauma

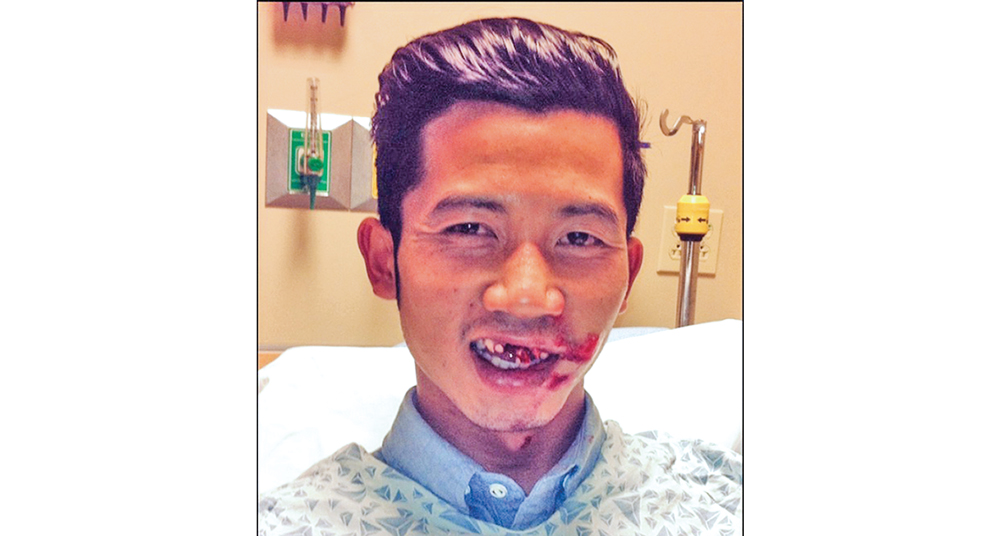
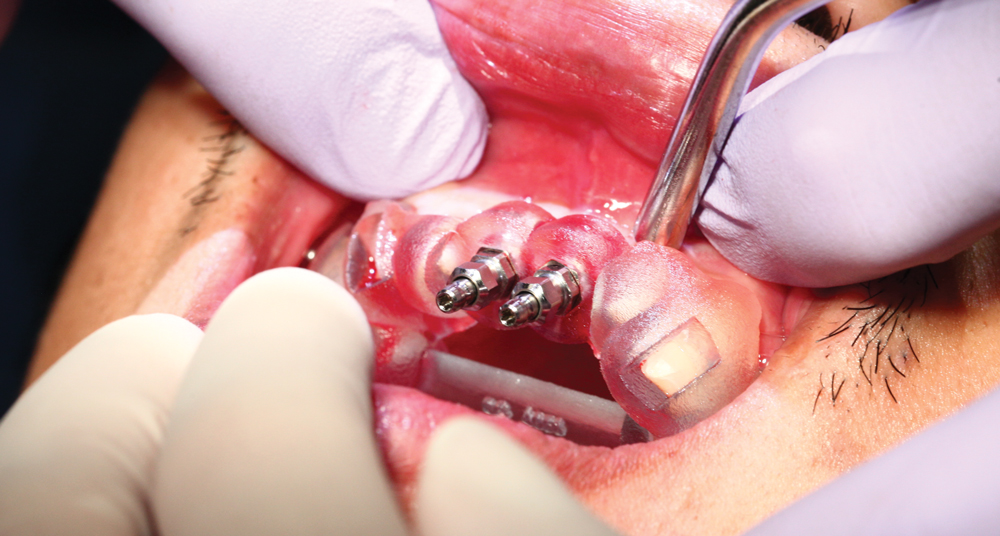
A Glidewell Laboratories dental technician was in a motorcycle accident and was taken by ambulance to the hospital. Fortunately, his injuries were not life-threatening; however, the trauma resulted in the loss of his maxillary central incisors as well as other facial injuries. Several months after being released from the hospital, he presented to the operatory to receive dental treatment. In the following case report, I used Obsidian® lithium silicate ceramic in conjunction with guided implant surgery to restore five anterior units.
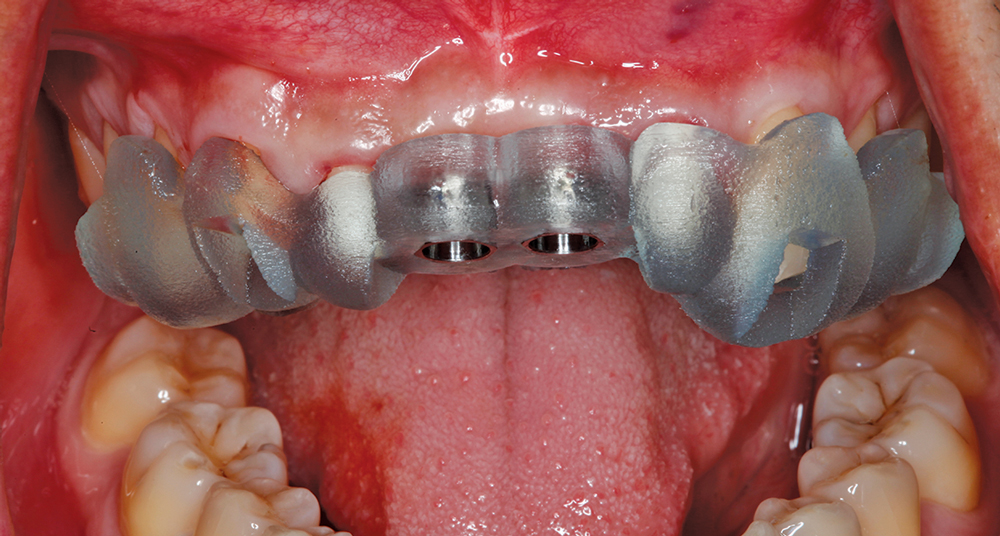
The intaglio surface of the BioTemps was checked with FIT CHECKER and relieved as necessary, to ensure that no functional load was placed on the implants during the osseointegration period.
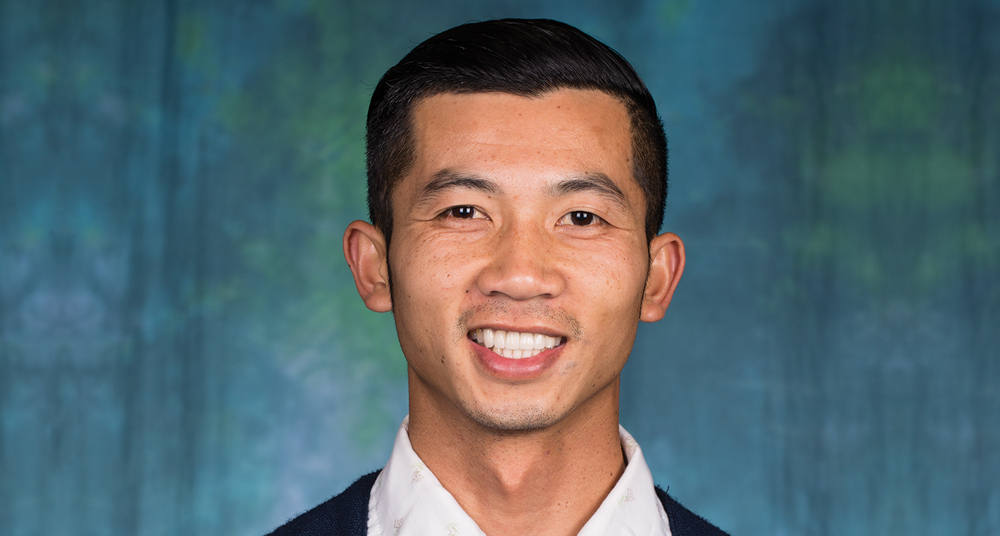
Conclusion
This patient was able to have highly esthetic final results because of careful planning of the surgical and restorative phases, and extended tissue recontouring during the provisional period. Cases such as this require a more methodical, time-intensive approach to obtain the ideal final result. Patients who experience such extensive dental trauma are often eager to achieve final restorative results as quickly as possible, and a clinician must balance those desires with the requirements of the specific case. With the aid of Obsidian ceramic, which acted as an ideal solution for this case because it has the ability to match across a variety of restorative types, the patient was restored to the pre-accident function and an improved level of esthetics.
This patient was able to have highly esthetic final results because of careful planning of the surgical and restorative phases, and extended tissue recontouring during the provisional period.