2201 Dupont Dr., Irvine, CA 92612
© 2020-2026 Glidewell. All rights reserved.
800-854-7256 USA
How saying yes to a patient can open the door to unexpected opportunities.

Over 20 years ago, with a restorative-focused practice, Dr. Gy Yatros wasn’t thinking about dental sleep medicine. But when a patient needed his help, he took a chance that changed the course of his career — and life — for the better.
Dr. Yatros recently spoke with Smile Bulletin about his experience treating his first sleep apnea patient, the mistakes and bumpy road that followed, and the simple process that resulted in a successful dental sleep practice.
Smile Bulletin: How did you get involved in dental sleep medicine?
Dr. Gy Yatros: In the ’90s, I had my restorative practice on Anna Maria Island, Florida, where I practiced until 2013. I had spent a lot of time at the Pankey Institute, and other places, trying to build a fee-for-service practice. I had a patient, and I had restored her mouth and her husband’s mouth. She came in for a recall right at the time I was having lunch. I went in to check the recall appointment, and she said: “Hey, Dr. Yatros, I’ve got a prescription here from my doctor. I’ve got apnea. I can’t wear CPAP. Can you make me one of these devices he says that you can make?”
And that’s where I said the words that changed my life. I said: “You know what? Yes, I can! Give me just a moment and we’ll talk about that. Just a minute; I’ve got to go next door.”
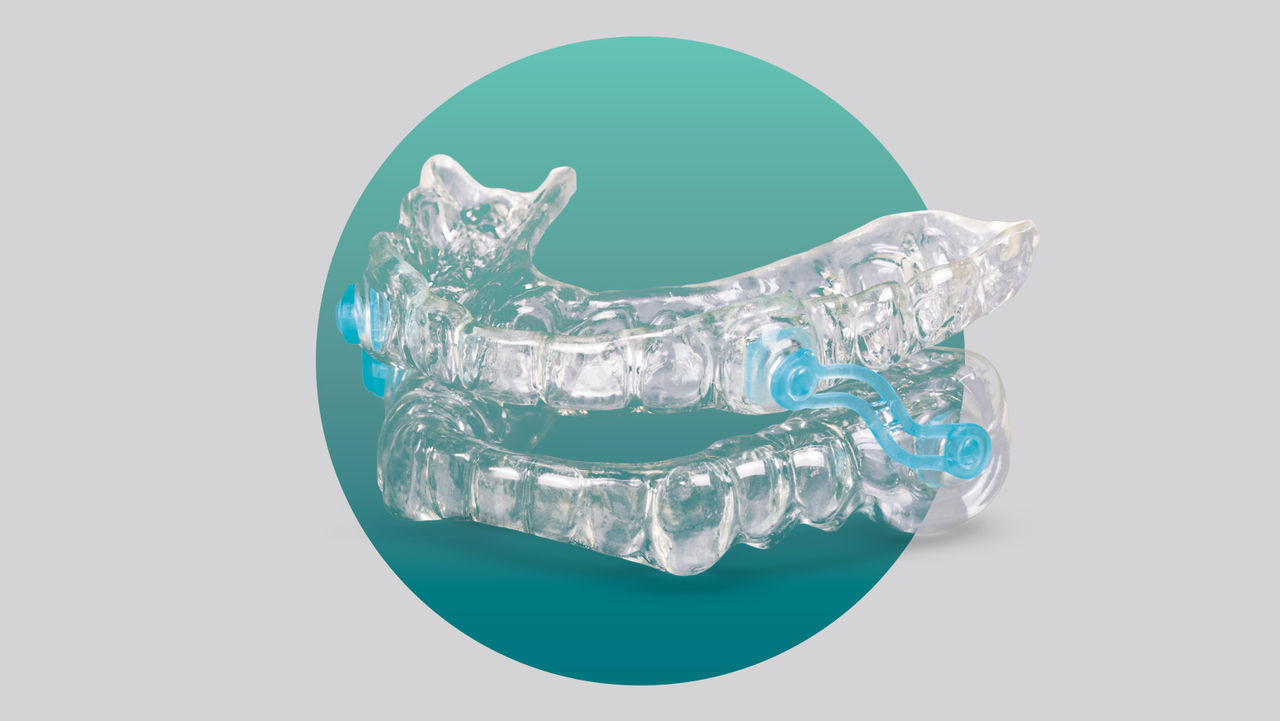
I scurried back into my office and was about to quickly finish my lunch, when I happened to spot marketing materials from Glidewell — it was a big shiny postcard with the words “Silent Nite®” on the front of it. It was perfect timing. I called Glidewell up and said, “I see y’all make these devices, so what do I need to do?”
They said, “Just take a couple alginate impressions and a CO bite” — that’s what we used to call it back then. I said, “OK,” and asked how much it was, and they said it was $99.
I went in to see my patient and said, “Yeah, we can do that for you.” I always joke that I used my complicated accounting system to come up with a fee. I told her it was going to be $300. That’s what I used to do. Now I do business consulting; that’s not the way you should set your fees, by the way. But I charged her $300, we did some alginate impressions, and I handed the Silent Nite appliance to her a couple of weeks later.
Dr. Gy Yatros treated his first sleep apnea patient with an oral appliance.
I didn’t think much of it until a few days later when I saw this same patient coming through the door into the reception room. I knew she didn’t have an appointment because we had a morning huddle that day. And my first thought was: She’s spent tens of thousands of dollars on her mouth, and some porcelain’s broke or something. What’s she doing here unannounced? She’s got an issue.
But she didn’t seem upset, and — as I tried to get into my office without her seeing me — she came in and grabbed me. “Hey, Dr. Yatros, I’ve got to talk to you,” she said.
I thought, Oh, no. What’s wrong here?
She hugged me and said: “I just want to thank you for this. I feel so much better. My husband will sleep in the room!” Her chief complaint was the snoring, and that’s what got her to complete a sleep test. Her husband wouldn’t sleep in the same room.
“This is fantastic,” she said. “I’m going to tell all of my friends, if that’s OK.”
That was fine with me. She started telling her friends, and I’d have one or two people come in per month because she’d referred a few people in. And I made them these snore guards. Then the doctor who had worked with her, Dr. Sanjay Yathiraj, called me up and said: “Dr. Yatros, I want to meet you. I didn’t realize there was someone on Anna Maria Island that was trained in sleep.” Of course, I wasn’t. I didn’t know what the heck I was doing.
He said, “I’m going to start sending you patients, if that’s OK.”
I was happy at that point because I was in the first stage of learning. I said: “That sounds great! Send me some patients.”
SB: The first stage of learning? Can you elaborate on that?
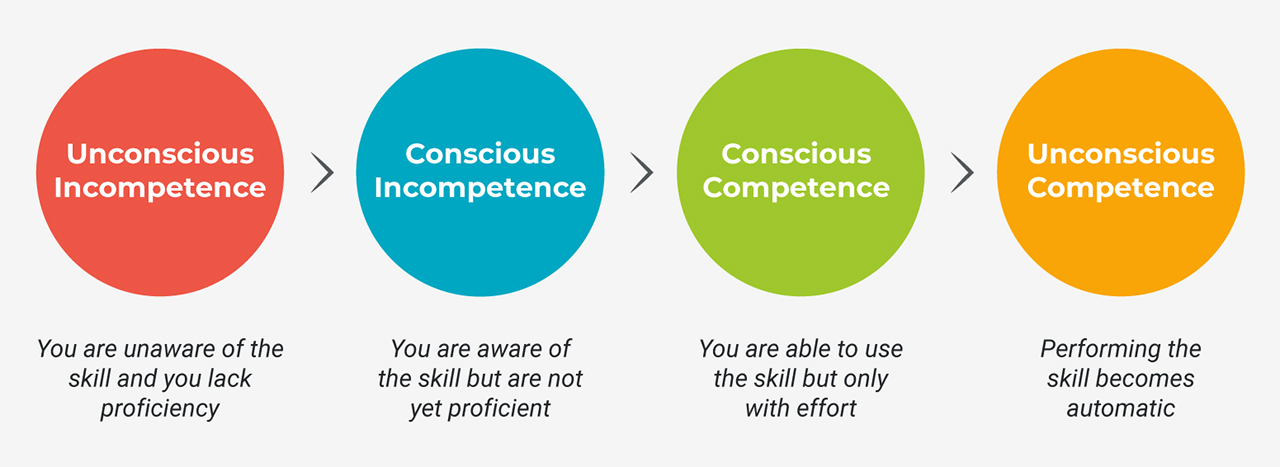
GY: There are four stages of learning. The first stage is a really great place to be, but unfortunately you can’t stay there forever. That’s where I was: unconscious incompetence. I didn’t know what I was doing. I had no training on this. I didn’t really even understand what sleep apnea was. Unconscious incompetence is when you don’t know that you’re not doing a good job. I was not conscious that I was doing a poor job — and that went on for a while, maybe six months to a year.
And then I did start having some complications. I had one patient whose bite changed and another that Dr. Yathiraj called me about. He said: “This patient’s AHI isn’t any better. You gave him this device and…”
I said, “The A-H-what?” I didn’t know what AHI was. And I thought, I probably ought to learn something about this if I’m going to be doing a few of these devices a month.
I tried to start doing education, but back then, there was nowhere to learn. It was really tough. I went to the AADSM and they didn’t teach the systems that you needed in a practice. I almost gave up because, at that point, I was in the second stage of learning: conscious incompetence. So I knew I was not doing a good job.
That’s no fun. You don’t feel good about yourself at that point. That’s where a lot of people quit. I almost quit, but I knew sleep dentistry was worthwhile because a lot of patients did really well.
The great thing that came out of joining the AADSM was that they sent me an email asking if I wanted to have a mentor because they were starting a mentorship program. There was no cost, so I agreed, and they assigned me to Dr. Richard Drake, who is now my partner at Dental Sleep Solutions and DS3. Through meetings with him, I realized there was a way to do this, and I learned how to organize dental sleep in my practice to get to the third stage of learning, which is conscious competence. In this learning stage, you can do it, but you’ve got to think about it. It’s not as fluid as, say, driving your car after you’ve driven for years. Instead, you have to think about every turn.

Dr. Yatros (right) with Dr. Richard Drake.
Through time and better systems, dental sleep became second nature. And the fourth stage of learning is where you want to be, which is unconscious competence, where you just go and do it. You don’t have to think about it — like when you’re driving your car after you’ve driven for years.
In 2013, I got so busy with dental sleep medicine that I sold my dental practice to concentrate on treating snoring and sleep apnea. Now, I have three practices where we just do dental sleep medicine. I have an associate partner who sees a lot of the patients, and I spend 80% of my time training other dentists and the other 20% treating dental sleep patients.
SB: How long does it take to build a practice focused on dental sleep medicine?
GY: It took me a lot longer than it would now. Today, it’s a whole lot shorter. The barriers for dental sleep medicine have gotten so much lower. For example, originally, the biggest barrier was getting patients sleep tested. Now, even in the last two months, it’s gotten a lot easier because telemedicine is widely available. We can get people tested; we can get them treated. However, I think it’s a matter of how much effort you put in.
One of my mantras is that dental sleep medicine is not difficult. There’s nothing difficult about taking a protrusive bite, fitting a device, or even dealing with insurance and getting patients tested. All of those things are not difficult compared to doing a root canal or crown prep — or even dentures. But it’s complex. There are a lot of moving parts, and it’s just a matter of having systems in place that are well organized, and team members who can help orchestrate those systems and make the process go smoothly.
SB: Do you have any advice to readers about how they can set themselves up to be successful with dental sleep medicine?
GY: Most importantly, before setting up anything, you have to decide that this is important. You have to believe that, as a dentist, you should be looking at the airway and talking to patients about their risk for suffocating at night. You have to embrace that.
I find that that’s the biggest challenge: Dentists feel uncomfortable. So the first step is to fully vest themselves and believe in what they’re doing. Then we break it down into what we call the four pillars for dentists’ success in dental sleep medicine:

To make dental sleep medicine a bigger part of the practice, Dr. Yatros says dentists should understand and believe in the importance of airway health.
SB: How should dentists start the conversation with patients?
GY: Once they make up their mind that this is their job and they feel good about it, they’ll talk to patients about snoring and sleep apnea. It’s not hard to give someone a questionnaire to see who’s at risk. They should ask, “Do you snore?” If so, they can go down the route of treating the airway. Half of adult patients snore. So it’s about having confidence and initiating that discussion.
Then they need to be trained. Being competent gives you confidence. To gain confidence, I recommend making sleep devices for your friends and family. Dentists know enough people in their circle of friends and family who need a solution for their airway.
SB: Have there been any recent changes — opportunities or challenges — in dental sleep medicine?
GY: I will admit, I’m coming at this from a biased point of view because I am very passionate about dental sleep medicine. I think it’s the best thing I ever did — other than marrying my wife Maria and having our son Nick. Nothing’s been more fulfilling professionally than being involved in it.
When it comes to dental sleep medicine, there are definitely opportunities that weren’t there before. If we go back to 2006, we didn’t have home sleep testing. Insurances didn’t cover this and even the standard of care did not include dental devices as a first line of therapy for OSA. All of that has changed over the last 10–15 years. What’s changed in the last three months is that telemedicine has become the norm. And not only has it become the norm, but insurance companies are also paying for telemedicine visits — which they did not prior to COVID-19.
One of the challenges has been getting your patient sleep tested because there’s this big controversy over whether dentists should be allowed to order sleep tests. Even if the state allows that or even if you believe you can, some insurance companies — along with Medicare — won’t honor the sleep test if ordered by the dentist. That’s been a challenge.
Right now, there are several companies we’re working with. You can have the patient go to a telemedicine visit. You say: “You’re at risk. You need to be tested. Let me set you up with a telemedicine visit.”
The patient can meet the doctor on the computer or iPhone. The doctor says, “Yes, you’re at risk.” The doctor orders the test. There are disposable tests that are mailed or delivered to the patient. With some of the services, we can get the test results back within a week. And I’ve done everything above board because the doctors ordered the test, the sleep doctors read the test, and now we have a diagnosis and all the paperwork delivered back to us that we’d spend weeks tracking down from the local doctors to get. That piece has really changed.
In addition, over the last couple of years, the testing itself has changed. The units have gotten smaller and more comfortable. Services are available to do this, so getting your patient tested is much easier now.
For dentistry, the one thing that is common with almost every dentist I’ve talked to over the last several months is that they seem to be more stressed than they ever have been and they’re making less money. My analysis of that is it has to do with the PPE. It’s disrupting the workflow, and then we’re all stressed about the pandemic.
Is there an opportunity for dental sleep medicine? Yes, because we don’t make aerosols. We don’t have the PPE requirements of a dental office. We model ourselves after a doctor’s office. So you can practice in today’s world a lot easier.
Most of our appointments can be handled over teledentistry now; we’ve pivoted to that. That includes our consults and follow-ups, and we can even use the Glidewell™ Self-Impression Kit for the people who don’t want any contact at all. That’s a great option. You can theoretically do a 100% contactless treatment with dental sleep medicine. You can’t do that in dentistry.
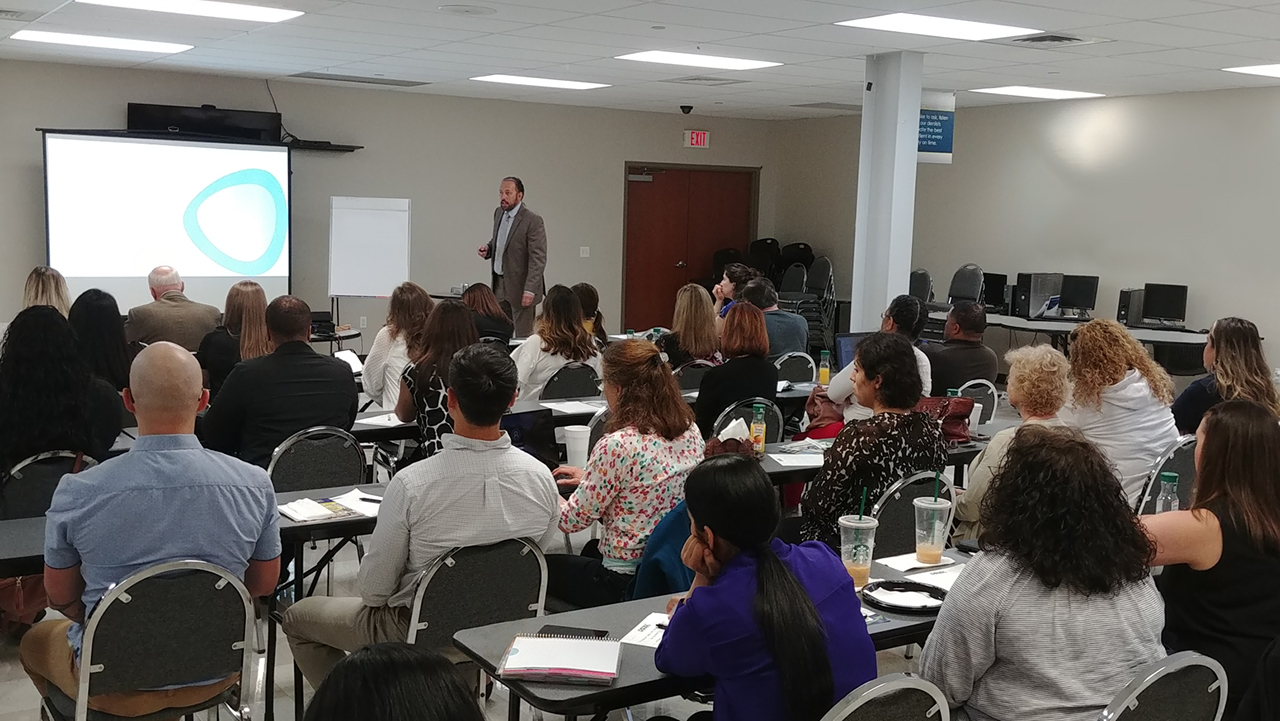
Dr. Yatros gives back to the profession by sharing his knowledge about dental sleep medicine.

Dr. Yatros, center, with team members at New Concept Sleep, a dental sleep practice with three locations on Florida’s Gulf Coast.
SB: In conclusion, what is your advice for dentists considering involvement in dental sleep medicine?
GY: You’ve got to be able to take a chance. You can’t just stay in your comfort zone. Had I not taken a chance, my life would be totally different today. Dental sleep medicine is the central part of my work life — all because I took a chance and made a dental device, the Silent Nite Sleep Appliance, for someone 20 years ago.
So many people feel like they’ve got to have all the stars aligned before they get started with dental sleep. But they just need to get out there and start doing this.
SB: Thank you for sharing your story, Dr. Yatros.
GY: Thank you for the opportunity.
To learn more about snoring and OSA, as well as receive a straightforward protocol for screening and treating patients, visit glidewelldental.com/pmad.
To learn more about Dr. Yatros, his courses and the DS3 system for dental sleep medicine, visit ds3sleep.com.
Send blog-related questions and suggestions to hello@glidewell.com.


