Screening Patients for Sleep-Related Breathing Disorders

The world has changed dramatically in the time since this series launched. The first article (Chairside® magazine Vol. 15, Issue 1) covered the legal necessity of initiating a program to screen all patients for sleep-related breathing disorders. Now, as we focus on rebuilding our practices after the COVID-19 shutdown, this is a particularly favorable time for clinicians to study the intersection of dentistry and sleep apnea (and other sleep disorders).
Pause to establish a screening protocol that can identify patients who may have airway or sleepiness issues. These patients can receive potentially life-saving intervention through provisional mandibular advancement devices. Screening for sleep-related breathing disorders requires no additional equipment, and this important service can expand your practice’s revenue streams.
Complaints relating to sleep and wakefulness are ubiquitous in our dental patient populations. Both adult and pediatric patients suffer.1 As a result of the high incidence of sleep-related breathing disorders, the American Dental Association (ADA) has resolved that all dentists must institute a program to screen their patients for airway and sleepiness issues.2
Screening can be accomplished in various ways. The most effective technique may be to add a few questions to your health history.
APPLYING THE ‘SNORE +’ METHOD
Generally, it is accepted that 70% of patients who snore loudly have sleep-related breathing disorders. When patients answer “yes” to question 1, apply the “Snore +” method to look for other indicators that confirm the probability of sleep disorders.
For example, a patient who reports snoring loudly every night and being treated for hypertension could be described as “Snore + Hypertension.” That patient would be referred for an evaluation by a sleep physician. Other examples include “Snore + Diabetes” and “Snore + Obesity.”
If a patient’s answers regarding airway health point to a possible airway or sleepiness risk, further screening and examination are indicated.3
Patients with a sleep disorder frequently present with a complex medical history. It is common for patients with uncontrolled obstructive sleep apnea to have previous diagnoses of certain health conditions and dental signs,3,4 such as those in the following lists.
EXAMPLE QUESTIONS FOR SCREENING
- Do you snore?
- Have you ever had a sleep study?
- Have you ever been diagnosed with sleep apnea or another sleep disorder?
- Have you ever used a CPAP device?
- Have you ever awakened gasping or choking?
- Has anyone ever told you that you stopped breathing during sleep?
- Do you doze easily or feel sleepy in quiet situations?
- Do you take naps?
- Do you feel rested after a night’s sleep?
- Do you frequently have to get up at night to use the restroom?
COMMON PREVIOUS DIAGNOSES
- Hypertension
- Stroke
- Heart disease
- Type 2 diabetes
- Obesity (body mass index > 30)
- Depression
- Gastroesophageal reflux disease (GERD)
- Sexual dysfunction
- Dementia/Alzheimer’s disease
- Cancer
- Atrial fibrillation
COMMON DENTAL SIGNS OF SLEEP-RELATED BREATHING DISORDERS
- Temporomandibular joint dysfunction
- Bruxism
- Excessive tooth wear (particularly on the anterior teeth)
- Vaulted palate
- Malocclusion (anterior crowding and crossbite)
- Constricted mandible
- Large (coated and scalloped) tongue
- Enlarged tonsils
- Small nasal valves (difficulty breathing through the nose)
- Battered soft palate
- Elongated, battered uvula
- Class III or Class IV Mallampati classification
KNOWING THE RISK FACTORS
Mallampati classification is used to determine the relative length of the soft palate and, secondarily, the size of the tongue. The longer the soft palate, the higher the risk of obstructive sleep apnea or another sleep-related breathing disorder.
For assessment, a patient would need to sit upright, open the mouth wide and stick out the tongue. The classifications of 1–4 are determined by how much of the soft palate and uvula are visible when looking into a patient’s mouth from the front. A patient with a Mallampati classification of 3 or 4 has a high probability of having obstructive sleep apnea.5
MALLAMPATI CLASSIFICATIONS
- Class I: Uvula, fauces, soft palate and tonsil pillars are visible
- Class II: Uvula, soft palate and fauces are visible
- Class III: Base of uvula and soft palate are visible
- Class IV: Only hard palate is visible
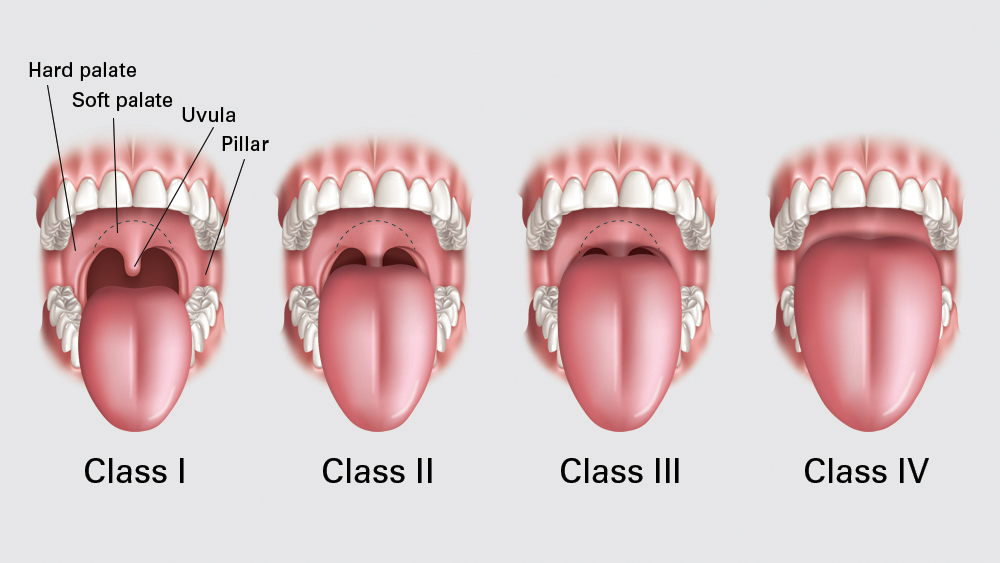
Clinicians can use the Mallampati classifications to evaluate the relative length of the soft palate and, secondarily, the size of the tongue. The longer the soft palate, the higher the risk of obstructive sleep apnea or another sleep-related breathing disorder.
Once a patient is identified as having a high probability of a sleep disorder, it is important to assess how the potential issue might be affecting the patient. The Epworth Sleepiness Scale (ESS) is a screening tool that can assist dentists and physicians in determining patients’ relative sleepiness.6
The ESS features a series of eight questions designed to determine the likelihood of a patient falling asleep in common situations. If a patient has a high probability of falling asleep at an inappropriate time, it is prudent for a dentist to initiate immediate care.
However, the ESS is limited in that it evaluates only the level of daytime sleepiness. The maximum score on the ESS is 24, and patients who score 10 or more on the ESS are excessively sleepy. It is not uncommon for these patients to have automobile accidents or other types of serious injuries.
When screening procedures uncover patients who have ESS scores ≥ 10, practitioners should use every reasonable means to lessen the probability of these patients causing injury to themselves or others. If a patient has a high probability of having a sleep disorder, it is important to assess the severity of the patient’s symptoms to determine whether any provisional therapy is indicated.
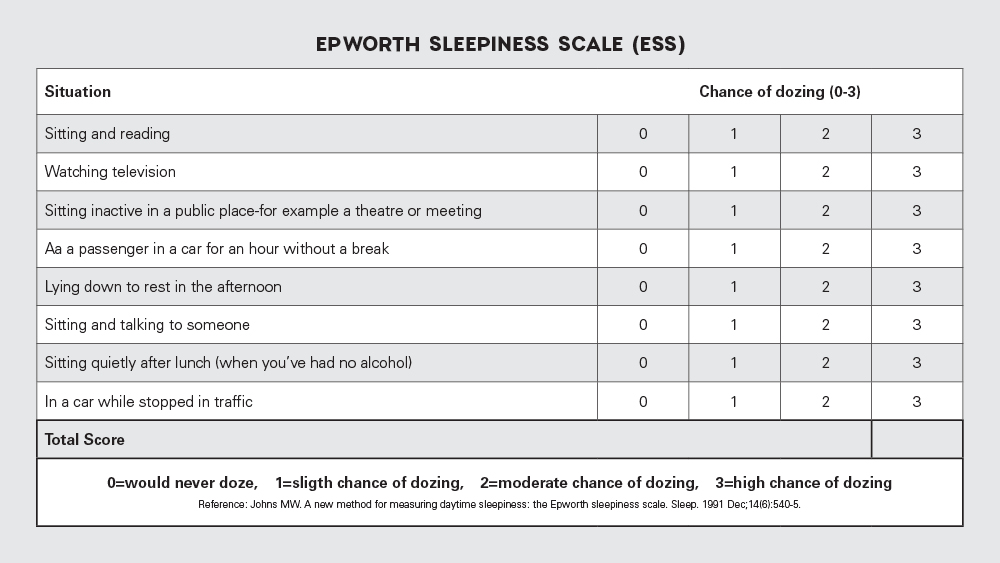
The Epworth Sleepiness Scale (ESS) can be a helpful screening tool for determining whether a patient is dangerously sleepy and needs immediate therapy.
A positive response to the airway questions in your health history raises a concern that the patient may have one of many possible sleep disorders. In-office screening surveys may not effectively distinguish between patients who have sleep hygiene issues versus those who have a diagnosable sleep disorder. Only an overnight sleep test can provide a definitive diagnosis.
Therefore, all patients who screen positively for sleep-related breathing disorders must be referred to a physician for evaluation. Under current protocols, sleep physicians are tasked with the responsibility of determining the most appropriate therapy.
However, in light of the limited number of sleep physicians in the U.S., wait times are becoming unacceptably long. It is not uncommon for patients to wait months for an appointment with a sleep physician. Given the serious consequences of excessive daytime sleepiness, it is important for clinicians to provide provisional dental treatment options for patients who are facing such burdensome wait times.
If a patient is excessively sleepy upon screening, a provisional mandibular advancement device is a reasonable therapy to be utilized during the wait for a definitive diagnosis and treatment.
The Silent Nite® Sleep Appliance is a typical recommendation for a provisional mandibular advancement device. The Silent Nite sleep device, which can be fabricated by Glidewell in five in-lab working days, is reasonably priced. The price is important as all provisional therapy is provided on a cash basis. Because there is no definitive diagnosis, medical insurance benefits are unavailable.
If a patient is excessively sleepy upon screening, a provisional mandibular advancement device is a reasonable therapy to be utilized during the wait for a definitive diagnosis and treatment.

CONCLUSION
It is now a legal requirement for all dentists to screen their patients for sleep-related breathing disorders. If, during screening, you identify a patient who is dangerously sleepy, a provisional mandibular advancement device such as a Silent Nite appliance may be necessary to minimize risk for the patient as well as your dental practice.
Make sure to read the next article in this series. In part three, we’re discussing how to safely implement provisional mandibular advancement devices as interim dental treatments for possible sleep apnea and other sleep disorders.
Click here for Part 1: "Why Every Dentist Must Screen for Sleep-Related Breathing Disorders"

Click here for Part 3: "Providing Immediate Treatment: Introducing the PMAD Protocol"
References
- ^Redline S, Larkin E, Schluchter M, et al. Incidence of sleep disordered breathing (SDB) in a population-based sample. Sleep. 2001;24:A294.
- ^American Dental Association [internet]. Chicago: American Dental Association; c2019. The role of dentistry in the treatment of sleep related breathing disorders [cited 2019 Aug 25]. Available from: www.ada.org/~/media/ADA/Member%20Center/FIles/The-Role-of-Dentistry-in-Sleep-Related-Breathing-Disorders.pdf.
- ^Barkoukis T, Matheson J, Ferber R, Doghramji K. Therapy in sleep medicine. Philadelphia: Elsevier/Saunders; 2011.
- ^Berley JK, Carstensen S. The clinician’s handbook for dental sleep medicine. Chicago: Quintessence Publishing; 2019.
- ^Yu JL, Rosen I. Utility of the modified Mallampati grade and Friedman tongue position in the assessment of obstructive sleep apnea. J Clin Sleep Med. 2020 Feb 15;16(2):303-8. Epub 2020 Jan 13.
- ^Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540-5.