2201 Dupont Dr., Irvine, CA 92612
© 2025 Glidewell. All rights reserved.
800-854-7256 USA
Tooth grinding merits a deep dive into dental sleep medicine.

A friend called me recently to ask about nightguards. His dentist has been talking to him about tooth wear and the need for a Comfort H/S™ Bite Splint for a couple of years. The challenge is that nightguards are not covered by dental insurance and “cash is king in a pandemic.”
I asked the following three questions, and I think I fixed the problem.
Question 1: How old are you?
“I’m 58 years old,” he said.
Question 2: Is the collar size of your shirt larger than 17 inches?
“Yes.”
Question 3: Has anyone observed that you stop breathing while sleeping?
“Randy, I have sleep apnea. I have been on CPAP for over four years. What does this have to do with tooth grinding and getting a nightguard?”
I then continued the discussion as follows:
A sleep apnea device — also called a mandibular advancement device (MAD) — could provide you with the tooth protection required and complement your continuous positive airway pressure (CPAP) therapy. A sleep apnea device also can be used as an alternative when access to a CPAP machine is simply not feasible (e.g., while camping or on a plane). An oral sleep appliance is essentially two nightguards joined in a way that advances the mandible, adds tone to the airway, and defends the airway from collapse. An upper and lower nightguard will defend the teeth from wear associated with sleep bruxism.
Sleep researchers have shown that treating sleep apnea with CPAP will alleviate some or all of your sleep bruxism. Most patients only wear their CPAP device four to five hours per night. An oral appliance will help protect your teeth and manage your airway for the balance of the night. There is no clinically relevant difference between MAD and CPAP therapies in the treatment of mild or moderate OSA when both treatment modalities are titrated objectively.

Patients who suffer from sleep apnea can find relief with either a mandibular advancement device (MAD) or a continuous positive airway pressure (CPAP) machine. It’s beneficial to provide a MAD to patients who are unable to tolerate CPAP therapy throughout the night.
There is no clinically relevant difference between MAD and CPAP therapies in the treatment of mild or moderate OSA when both treatment modalities are titrated objectively.
Patients who have an OSA diagnosis have many treatment options. Unfortunately, treatment is not delivered or coordinated by a single provider. Asking your physician for a sleep appliance for use when traveling, or more importantly in case of power outage, is prudent and within the standard of care, but is not easy to access. Additionally, if you have had a CPAP machine for four years, your durable medical equipment (DME) coverage will accommodate a sleep appliance, and the cost of the appliance will be your copay.
One of the benefits of this strategy is the improved efficiency of your airway. A more patent airway may allow you to bring your CPAP pressure down. This will make your CPAP therapy more tolerable and you may find it easier to comply with treatment over time. The best news is that the appliance is covered by medical insurance with a prescription. Access to providers who offer this service is improving. If you are currently under care for sleep apnea, this additional option is likely available to you.
At Glidewell, we understand that sleep apnea is a life-threatening condition that requires nightly treatment. A CPAP machine is an excellent option; however, studies have shown that compliance is the biggest challenge, and when you factor in power outages and lifestyle events like camping, it gets even worse.
It is clear that patients need other options, such as an oral appliance, to manage their condition and still live a full and healthy life. This year, due to hurricanes and wildfires, we have had the worst year on record of power outages. This is not a single data point. In fact, there has been a steady increase in weather-related power interruptions over the last 40 years. In the first eight months of 2020, over 2 million people lost power, in some cases for a week or more.
There is a direct connection between tooth grinding during sleep (sleep bruxism) and sleep apnea, which causes disrupted sleep patterns (also called micro-arousals). The condition of sleep bruxism is estimated to affect 8% of the adult population and the condition gradually decreases as the patient gets older. Tooth grinding is an interesting phenomenon. It actually covers clenching, grinding, bracing, or thrusting of the jaw while awake or asleep.

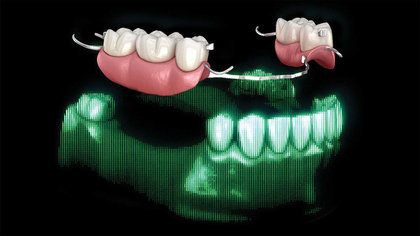
Patients who wear a nightguard (left) for sleep bruxism may benefit from learning about an oral sleep appliance (right).
Sleep bruxism is characterized as sleep-related rhythmic masticatory muscle activity (RMMA), which is usually associated with fragmented sleep patterns. These micro-arousal sleep patterns are frequently seen in patients who have sleep apnea. The cycle of sleep, then airway obstruction, then arousal, often involves RMMA, resulting in worn and broken dentition, jaw and muscle pain, and temporal headaches. For years, dentists have prescribed nightguards to defend teeth from damage without understanding the sleep disorder associated with it; however, the micro-arousals still occur and the RMMA activity continues.
 There is a connection between tooth grinding during sleep (sleep bruxism) and sleep apnea, which causes disrupted sleep patterns.
There is a connection between tooth grinding during sleep (sleep bruxism) and sleep apnea, which causes disrupted sleep patterns.
An oral sleep appliance that provides stability to the airway and more restful sleep patterns, as well as dentition protection, is an excellent choice for patients with this condition. Bruxism is such a common condition that at Glidewell we have made more than 2.7 million nightguards over the last five years.
When an oral appliance is used together with a CPAP machine, it can serve to activate the muscles and ligaments of the airway, splinting the airway open to allow the CPAP to work at a much lower pressure. Lower pressure is one of the keys to a more comfortable patient and a better night’s rest.
My friend is a perfect example of a patient who can benefit from oral appliance therapy. If you’re finding that your patients suffer from sleep bruxism and wear a CPAP, consider discussing oral appliance therapy as a solution for promoting healthy dentition and high-quality sleep.
To learn more about snoring and OSA, as well as receive a straightforward protocol for screening and treating patients, visit glidewelldental.com/pmad.
Send blog-related questions and suggestions to hello@glidewell.com.