Sleep Disorders: Dentists Key in Treatment – Interview of R. Michael Alvarez, DDS

I recently had a chance to speak with Dr. R. Michael Alvarez, who specializes in sleep dentistry. Here, Dr. Alvarez, a longtime user of the Silent Nite® anti-snoring appliance, shares his thoughts on treating snoring and sleep apnea. Dr. Alvarez believes this largely untapped area of dentistry will be a huge growth center into the future.
Dr. Michael DiTolla: Good afternoon, Mike! Today we wanted to speak with you about the sleep dentistry side of your dental practice. You have done many Silent Nite and TAP® II appliances with us over the years. Tell me about how you got introduced to sleep dentistry. Take me back to those first few cases.
Dr. Michael Alvarez: That was some 21 years ago. I was involved with a lot of TMD/TMJ dysfunction type of therapy. After going to USC, I worked for one of my professors in Beverly Hills who was a TMJ specialist. I started doing a lot of lower splints and learned a technique called the Sears Pivot Point Technique from this dentist that I worked for, Dr. Harold Ravens. He introduced me to a lot of the pioneers in TMJ work: Dr. Gelb in N.Y., Dr. Willie May in New Mexico. I left Beverly Hills to come back to my hometown, Fremont (California), where I am now, and I brought with me the knowledge. No one here knew about TMJ. It was like a backward community in the dental field.
MD: Yes, in 1988, when I graduated, TMD was not taught well at my dental school. And we left, not so much confused, but almost devoid of any knowledge.
MA: That’s where I was; it just happened Dr. Ravens was giving a lecture on it, and I had the symptoms myself, so I asked him about it. And he said, “Why don’t you come work for me?”
MD: There’s no better way to know what a patient is going through and know the different treatment modalities than to suffer from the condition yourself, I would guess.
MA: That’s right. That was the connection for me. I can talk to the patients from personal experience. So that’s how I started in this TMD, and actually a sleep disorder called bruxism. Bruxism was the original sleep disorder dentists were working on for decades before we got involved with sleep medicine.
MD: Yes, and if I called 100 dentists right now, I’m pretty sure 99 of them wouldn’t consider bruxism a sleep disorder.
MA: Correct. And if you called the same 100, most of them would not want to treat TMD disorders.
MD: I can certainly, at times in my career, place myself in that group as well. And I think if I had as little knowledge about doing porcelain veneers as I did about TMD, I would be just as afraid of doing those esthetic restorative cases as I was of TMD. It really comes down to knowledge, doesn’t it?
MA: Yes, and I think this new magazine that Glidewell has come out with is an excellent vehicle to help educate and take some of the fear away from these procedures. So, to finish the story, I was taking some advanced courses in TMJ therapy from a dentist in Minnesota named Dr. John Witzig, a real powerhouse in orthopedic functional appliances and doing some preliminary orthodontic work. So I started using some of these appliances that mimic the Silent Nite with the same idea — reposition the mandible anteriorly. And we used it to unload TM joints.
MD: Appliances like the Twin Block?
MA: This is before the Twin Block — we were using Bionators. So I was using Bionators and orthopedic correctors on adults for the TM joint problems. What happened was, most of my patients were women between 26–65, and I told them to wear the appliance when they are having discomfort, but that they don’t need to wear it if they’re not feeling pain. It’s kind of on an as-needed basis until you get out of the pain syndrome. Well, I had a couple women who came in to see me and said, “No, I can’t do that because my husband will leave the bedroom if I don’t wear the appliance.” And I didn’t understand what that was about unless they were grinding their teeth and making noise. And they said, “No, it stops my snoring.”
MD: That’s amazing! You were trying to treat TMD and ended up solving snoring problems as well. Is it fair to say the basic premise when you were using the Bionator was, if you bring the mandible downward and forward, you will improve the TMJ situation?
MA: Correct. That was kind of advanced-type of thinking at that time. I didn’t understand it all, but I wanted to study it, so I selected a few patients who told me about this. They were consistently wearing the appliance. They had to wear it because it stopped their snoring.
MD: That is fascinating. I did my orthodontic training with a guy who learned a lot from Dr. Witzig, Dr. Brock Rondeau. He would talk about that and how you could just see the airways open up on a ceph when the patients had their appliances in.
MA: So that’s how it progressed. From TMD, to orthodontic/orthopedic work, into sleep disorder work. First, I went to the dental literature. I was looking for articles on snoring treatment or snoring improvement with an oral appliance, and there was nothing in the literature — remember, this was back in 1985. So I went to medical literature and found one article — only one — published in 1982 in the Journal of the American Medical Association. A psychiatrist in Chicago, Dr. Charles Samelson, had collaborated with a Ph.D. psychologist researcher at Rush Presbyterian St. Luke’s Medical Center in Chicago, and had written a paper on an oral appliance that helps reduce snoring and obstructive sleep apnea. Of course, I didn’t know what apnea was, so I read the article, and there was a number to call for a reprint, so I called the number and Dr. Samelson answered the phone. It was so wild. So I told him I’d done some anecdotal therapy with mouthpieces that moved the mandible forward on a couple patients, and they reported that their snoring was reduced or eliminated. And he said, “That’s good, but you have to have research behind it to make those claims.” He said his appliance had done that in 1982 by publishing the paper and the research. He said I needed to study his mouthpiece first and understand it better.
MD: What was the name of his appliance?
MA: It was called the tongue-retaining device. I was in a different league when I went to study this thing. Your tongue goes into a sleeve — like a vinyl sleeve — and it’s held out of the mouth.
MD: So there is some attachment to the teeth, I would assume?
MA: Well, actually, there’s a minor attachment. The device was very light or no retention. They’re non-retention appliances, but troughs that go around teeth are kind of shaped to go around the arches, and the tongue is held in the sleeve with a suction or vacuum. It has a turkey-baster type of effect.
MD: Have you worn one of these?
MA: I have.
MD: How would you rate the comfort on a scale of 1–10?
MA: Probably a 2 or a 3, but I liked it because I wore it and it really worked for me. When I turned 40, I started snoring and my wife told me I better start using one of those things I was talking about. It was actually very comfortable for me. Historically, about 10%–15% of the population with sleep disorders can accommodate this appliance and wear it. So its comfort is probably the biggest problem.
MD: That’s funny because I just turned 41 and it’s been requested that I start wearing a Silent Nite. It’s good to hear you say that the same thing happened to you at 40. Do patients tend to report the same type of experience to you?
MA: Yes. Well, I started lecturing on this with Dr. Samelson. He was trying to train medical doctors and lab technicians in the medical field to deliver the tongue-retaining devices. I went with him, saw how he presented, how he was trying to train these doctors and nurses to deliver a dental device. I pointed out to him that dentists are the group of people that should be doing these types of appliances. We’re used to working in the mouth with saliva and adjusting appliances, etc. And I took him to Dr. Witzig’s advanced course on TMD at the time. He was so impressed because there were 500 dentists at this hotel course. He was seeing all this amazing work that was being done, and decided we would start lecturing to and training dentists. I started a Continuing Education company in 1987, where he and I would lecture to dentists at accredited sleep disorder centers across the country and internationally as well. We were training dentists to show them how they play a role in sleep disorder medicine. We also started certifying them in using the tongue-retaining device. At this time, other appliances, such as mandibular advancement devices, were beginning to have papers published with one case or two or several. So we were starting to see more publishing on the therapy that I worked on. And Dr. Samelsen was impressed with the fact that both types of devices were working on helping snoring and sleep apnea.
MD: So when patients reported that it helped their snoring problem, you must have begun to realize that there was a significant portion of your practice that could be helped by these appliances.
MA: Actually, I didn’t think of that. I thought of, “How?” What am I missing? How come I never learned about snoring and a mouthpiece? All the work I’d done with Dr. Witzig and Dr. Ravens, no one had ever mentioned snoring as a problem that we would ask patients as a symptom. It was more of a curiosity. Is this really happening? Or is it just anecdotal or coincidental? When I saw the paper published, I knew there was something behind this. It was a different type of device, but it was a device. So I was able to help Dr. Samelson go to a dental laboratory called Professional Positioners in Wisconsin. They had a lab tech who was able to take his idea, the tongue-retaining device, and make custom oral TRDs. Models were sent to the lab and the TRDs were constructed to the arch shape — customized instead of “one size fits all.” So that’s the development of the TRD and the training that occurred. I started asking more patients in questionnaires about snoring. When people would walk into my office, my staff would ask about any snoring problems. So then I really started looking for it, and I got quite a few patients into treatment.
MD: Walk me through a typical treatment plan for someone you treat for snoring today. Walk me through the protocol and how you might use a Silent Nite in that process.
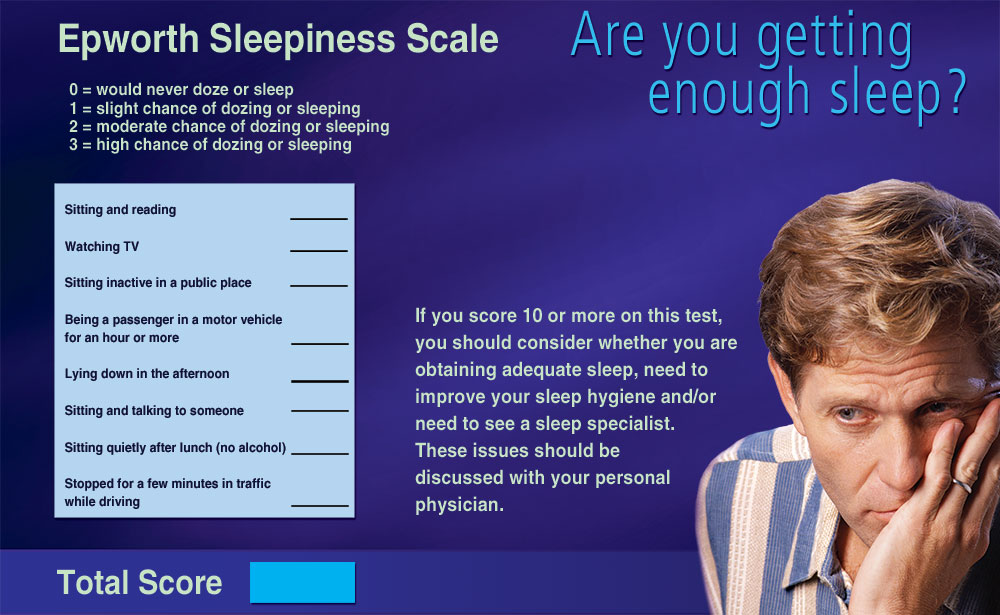
MA: The protocol from the Academy of Dental Sleep Medicine is that there has to be a physician involved in the diagnosis. Is it just benign snoring? Is it upper airway resistance syndrome? Is it obstructive hypopnea? Obstructive apnea? What is it, and how severe is it? The first line of protocol is a sleep study or a medical doctor’s referral to a dentist for an appliance.
MD: For the dentist who is reading this and finding out about it for the first time, how do they find a sleep doctor in their area who they can work with or at least approach?
MA: There are so many accredited sleep disorder centers in this country. It’s the biggest-growing field in medicine right now. All you have to do is look for a sleep disorder center, and there is a doctor who is affiliated with it. Either an MD or a Ph.D. And they are all over the place.
MD: Are there any good websites that might serve as an introductory place for them to find out about this?
MA: American Academy of Sleep Medicine (aasmnet.org) and Academy of Dental Sleep Medicine (dentalsleepmed.org). It’s an excellent way for dentists who want to get involved with this work to learn about the field. There is actually some protocol. The Academy of Dental Sleep Medicine has a way where we actually do board certification. We work with American Academy of Sleep Medicine. They are our advisors. They help us with our testing to certify dentists. So there is a whole avenue of specialists in this field. Some dentists don’t want to get involved with all that. The best thing for them is just to learn to not go into a lot of difficult cases, but know that there are some alternatives, and have the dentists who are involved in sleep disorder medicine help you if you have a problem. If you try a Silent Nite and you go so far, and if you get stuck, you can refer to someone else. It’s like with an endodontist — you try to do the endo, and if you get stuck, you send them to a specialist.
MD: So let’s say for our hypothetical patient that they go see a sleep doctor and there is no sleep apnea — it’s just a snoring case. How would you treat that case at that particular point?
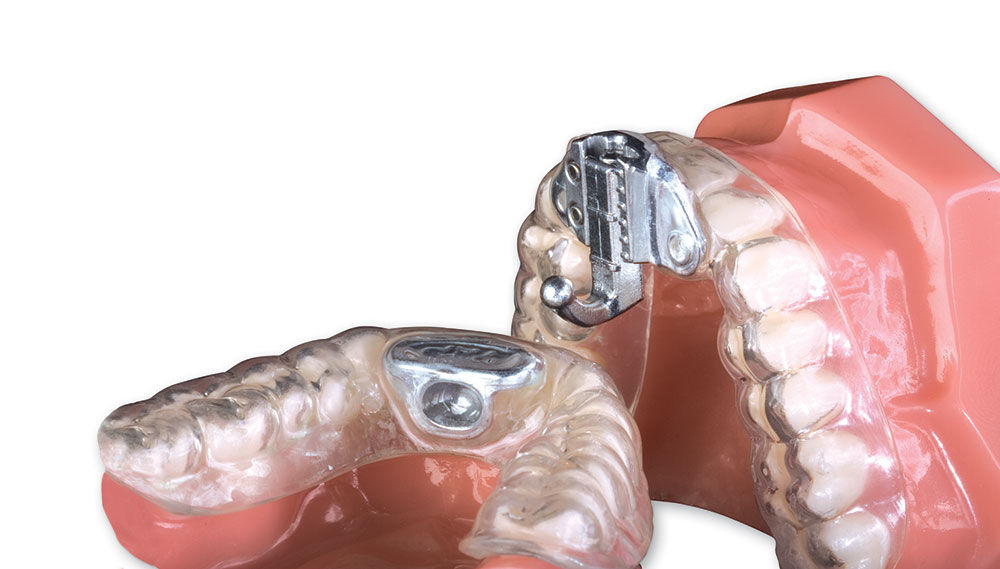
MA: I’ve had patients come in without a sleep study and they complain of a severe snoring problem. I tell them we can help them. I use the Silent Nite as a diagnostic appliance or as a trial appliance or a temporary appliance, if you will. I don’t have to have a sleep study to make this device for a patient. As we go along, I encourage a patient to get a sleep study, to get a diagnosis. It’s basically if you want to get into a long-term device or therapy. One of the positive things Glidewell has done is incorporate the TAP and TAP II appliances, because that is considered a long-term appliance. It has FDA approval for treating sleep apnea.
MD: I like your idea of using the Silent Nite that way because you give the patient and their spouse immediate relief, and you continue to gather more diagnostic information to make a decision on a more definitive appliance.
MA: I also use it as a training appliance. I’m training patients who have never worn a mouthpiece or a retainer to wear an appliance for the first time. The Silent Nite is so user-friendly because of its flexibility; it’s small, lightweight, there are no metal pieces. Patients need to get trained in wearing these, and it’s an excellent training device for a long-term appliance.
MD: I’ve had my Silent Nite for a week now, and I still haven’t made it through a night without taking it out at some point during the night.
MA: I tell my patients that, in the first week, if they have any difficulty the first week, take it out and leave it out. In the second week, I want them to take it out, rinse it off in some cool water and put it back in. The third week, I want them wearing it consistently. I have them come back three-to-four weeks after they start wearing the Silent Nite.
MD: This is a great example of me learning how to deal with patients by having to deal with it myself. I’m glad you just gave me permission to take it out for one more night!
MA: The Silent Nite also is a first-line approach at helping open up the airway. It allows some lateral movement. There is a little bit of vertical opening the patients can experience, so they can actually breathe through their mouth if they have a cold or allergies. I tell patients that, after we’ve used it as a diagnostic appliance and we go on to a TAP appliance, then the Silent Nite becomes a backup appliance for the long-term appliance. So it always has value.
MD: So they aren’t getting the Silent Nite at the beginning of treatment, then getting a definitive appliance and throwing it away. They didn’t spend this several hundred dollars just for two or three weeks.
MA: They’ll end up with two appliances.
MD: And maybe the patient could even wear it if they had a cold or something.
MA: Definitely.
MD: To get back to one other thing: Would you say the tongue-retaining device has fewer side effects than the mandibular repositioning appliances?
MA: It does because it does not do as much … has less effect on the TMD muscles.
MD: Do you still use the TRD?
MA: I still use the TRD. It’s still only 10%–15% of the patients who can tolerate it.
MD: Let’s take a patient who comes in with a sleep study and has been diagnosed with obstructive apnea — how do you approach that patient? Do you still make the Silent Nite or do you go right into the definitive appliance?
MA: I still make the Silent Nite. The reason is, some of these patients have never worn an oral appliance. They really need to get something that’s made quick, that’s easy, that’s user-friendly. They know it’s not meant for long-term use, but it will help them start.
MD: That’s a good point. So you’re doing Silent Nites, I guess, on almost every one of your patients because you want them to get used to an oral appliance, and it’s always going to be their backup appliance, as well.
MA: Right. I’m speaking in Texas next week to a group of TMJ specialists — craniofacial group — and that’s what I’m talking about is trial appliances.
MD: That’s interesting. I wanted to address some of the side effects really briefly. I know some doctors have called us who perhaps haven’t had the same amount of education you have, and they’re a little concerned when the patient comes back and says that, when they get up in the morning, for about 20 or 25 minutes they can’t seem to get their teeth together to eat breakfast. Can you talk about changes in occlusion?
MA: Occlusion — the teeth have not moved, but the muscles have changed during the night; they have moved. When the mouthpiece is taken out, these muscles cannot find their length. So what I do, it’s called a leaf gauge therapy. I use a small piece of vinyl like the material for the Silent Nite — or the old elastic Silent Nites — and I have them do a de-programming exercise in the morning that helps these muscles de-program and get back to their working length. They are very simple exercises.
MD: I assume it would consist of putting it between the anterior teeth and having them bite together.
MA: What they do is suck, bite and swallow. So sucking and swallowing muscles are the ones that are not getting the right length — the opening muscles. The closing muscles have been exercised all night, and then the opening muscles oppose them. When you take the appliance out, the opening muscles just don’t have the ability to get their bite back right away. (These are older people.) So, by doing the exercises, you get away from this jackpot — the dentist can — and help the patient get their bite back faster.
MD: For what percent of patients would you say that particular side effect occurs?
MA: About 20% of the patients.
MD: So if you make four or five of those, it’s going to happen in one of the patients, statistically.
MA: The other thing you get is, patients will complain of TMD-type symptoms — muscle pain.
MD: Oh, but it’s muscle pain more than TMD pain?
MA: Well, it is TMD pain, but it’s muscles — the same muscles we’re talking about. That’s another level up, where they have actual pain involved. They do the same exercise for that.
MD: How about teeth shifting?
MA: Especially appliances like boil-and-bite and Silent Nite for long-term use will also create this teeth movement because of the nature of the material. It’s like an orthodontic retainer, almost. Because of the forces of the lower jaw pulling back, you’ll get movement in lower teeth and upper teeth in different directions if you do it long-term. Silent Nite is just not strong enough to be a stable appliance for teeth to stay in their right positions.
MD: Whereas an appliance like the TAP …
MA: You have a better chance. And I do have some problems with TAPs because they do use that rubberized material, also. In the future you’re going to start seeing more of an acrylic appliance. There is a problem with tooth movement in long-term use of any oral appliance. Every dentist should have the informed consent form.
MD: What has your experience been with UP3 (uvulopalatopharyngoplasty) surgery to reduce snoring in the patients that you’ve seen? How does that work as a treatment modality with or without oral appliances?
MA: I usually tell patients that they should try the oral appliance first. If there is still snoring or apnea problems, then using the UP3 surgery, either the laser type or the scalpel type, as an adjunct to oral appliance therapy would then be indicated. But that does not mean they are cured — they still have to use an oral appliance after the surgery.
MD: And I’m assuming you’re suggesting the oral appliances first because it’s such a conservative treatment modality?
MA: And there’s less than 50% success with the UP3 surgery anyway for sleep apnea.
MD: That’s very scary.
MA: That’s why you don’t want to use it as a first line of therapy. One new therapy that’s much nicer, it’s called radio frequency therapy, and this is where a probe is introduced into the soft palate, and heat is introduced, and what happens after three days is, the tissue shrinks. So the uvula and soft palate will shrink without surgery, without cutting.
MD: Without tissue sloughing, either?
MA: Without sloughing. So it’s a nicer procedure, less painful, and the recovery is quick.
MD: I’ve been told the gold standard in treatment of sleep apnea is CPAP. Can you talk a little bit about that?
MA: CPAPs are excellent, but they really are best for people with severe sleep apnea. The American Academy of Sleep Medicine came out with a position paper in June of last year at the annual meeting that said, for people with mild to moderate sleep apnea, the first line of therapy is an oral appliance, not CPAP. It has lost its gold standard for mild to moderate sleep apnea patients.
MD: If a Silent Nite is an 8 on a scale of 1–10 for comfort, what would a CPAP be?
MA: 0 or 1. It’s horrible. I have people who’ve turned in their CPAP machines to me when they get their oral appliance because they are not using them. I use them to demonstrate to patients, and they can feel it. They can actually try it on.
MD: Have you seen patients who come to you and they already have a CPAP, and then you put them in an oral appliance and hook them up to the oximeter, and they can see their numbers go up anyway, and they can get rid of their CPAP and just use an oral appliance?
MA: Well, not with my oximeter. I have them do a follow-up sleep study. That is the best way to have objective data to see if it is effective enough successfully with an oral appliance. But yes, we’ve had quite a few people come off CPAP machines. The reason is, the gold standard in the past has been mild to moderate apnea patients have been getting CPAP machines, but now can go to oral appliances.
MD: That’s huge.
MA: It’s so huge. We don’t have enough dentists. With this position paper, we don’t have enough dentists in the country to take care of all these patients. So this work you’re doing is so important.
MD: I’m sure dentists are interested in insurance coverage for the sleep studies and oral appliances. Is there a range of fees you’ve seen?
MA: Sleep studies are usually covered by medical insurance. Medical doctors are the ones that should be prescribing the sleep studies, and then the insurance will pay for them. We’re out of that loop as dentists. The oral appliances, if the patient has a diagnosis of sleep apnea, there is a better chance for insurance coverage for the oral appliance like the TAP appliance. Insurance companies probably won’t pay for the Silent Nite. The way I have had insurance companies pay for the Silent Nite, I bill them for the exam, consultation and diagnostics, and charge $500. That includes the Silent Nite. I bill medical insurance.
MD: So dental insurance gets billed for none of it?
MA: Once in a while people have bruxism coverage, and even under orthodontics, under retainers, you can possibly bill dental insurance. But, as you know, dental insurance is very limited in what they pay. Not very many people have plans that cover orthodontics or the bruxism appliances.
MD: What would you say an average charge is for a more definitive appliance like a TAP II?
MA: I charge $2,000. That includes six months of follow-ups.
MD: How often do you see the patients?
MA: First, I see them on a three-week basis, then monthly, then every two months, then annually.
MD: So your practice is pretty much limited to sleep disorder and TMD?
MA: No, I have a general dentistry practice, also. It’s about 50% restorative, 50% sleep and TMD.
MD: Talk to me a little about the people who are dealing with sleep apnea and are dealing with daytime sleepiness. When their conditions significantly improve with an oral appliance, tell me a little about what they have to say about the improvement in their lives.
MA: Well, it’s a complete shift in their life. The quality of their life changes dramatically. People can’t thank you enough. It’s probably one of the most rewarding fields in dentistry, where you can help a person without picking up a drill to work on their teeth. It’s just a very satisfying feeling when people come in or their spouses come in or send candy or flowers saying, “Thank you for helping me.”
MD: We see patients get emotional when they get their new veneers because they feel like they can smile for the first time. But, when somebody’s felt like crud for the last 20 years and now suddenly they feel good again, that I’m guessing you’ve seen some tears before.
MA: Oh, yeah. And these men who are such tough guys and they try to hold it in, but I know they are so happy. Because, you know, this makes their wives happy.
MD: Talk a little about how treating something like sleep apnea can improve the overall help of the patient.
MA: There’s a direct link with people who have sleep apnea to cardiovascular problems like heart attack and stroke. There’s a mortality rate for anyone who has sleep apnea that’s untreated. That means they’re going to die sooner of a heart attack or a stroke. So there’s a definite correlation. There’s a direct link to cardiovascular accident. It’s already in the literature. It’s nothing new.
MD: It’s amazing that this area of dentistry that’s unknown to so many dentists and still relatively young, it seems to be one of the biggest areas that really does have an affect on health of the patient and might even be a life-and-death situation.
MA: Yes, in the future, future generations of children who don’t have a lot of fillings, who have straight teeth because they’ve had ortho — dentistry is going to move to this type of work. You’ll be mandated to do this work. It’s already happening. The American Academy of Sleep Medicine said that, for people with mild to moderate sleep apnea, the first line of therapy is to go see a dentist. It’ll take time for this position paper to reach doctors and dentists, but it’s going to happen.
The American Academy of Sleep Medicine said that, for people with mild to moderate sleep apnea, the first line of therapy is to go see a dentist. It’ll take time for this position paper to reach doctors and dentists, but it’s going to happen.
MD: You see a lot of talk in the dental journals about growth centers. I have a feeling you’ll tell me this is a great growth center for a general dental practice.
MA: I believe that, yes, in 10 years it’s going to be one of the major growth centers because the baby boomers will have gotten their veneers and crowns, and then dentists won’t know what to do.
MD: I imagine you really enjoy deriving 50% of your income without having to touch a handpiece or a drill.
MA: It’s definitely pretty cool!
Silent Nite is a registered trademark of Glidewell Laboratories.
TAP is a registered trademark of Airway Management Inc.