Digital Imaging: An Important Visual Aid in Treatment Planning and Case Acceptance
Photographic imaging has been available in dentistry for many years. Typically, it has been used for full-smile makeover simulations. Full-smile simulations can be very difficult and time consuming, however, and can often create unrealistic expectations or outcomes. This challenge, added to the expense of investing in traditional dental imaging software, leads many clinicians to completely avoid the use of digital imaging in their practice.
For anterior cases, digital imaging can and should play a vital role in patient education and decision-making. In fact, in situations where a few teeth are being treated, its use may be even more important than for full-smile restorations.
This case study will demonstrate how digital imaging can be used to communicate different treatment possibilities and assist in patient treatment acceptance. It will also detail the clinical technique used for achieving the patient’s desired final result (Figs. 1, 2).
Case Presentation
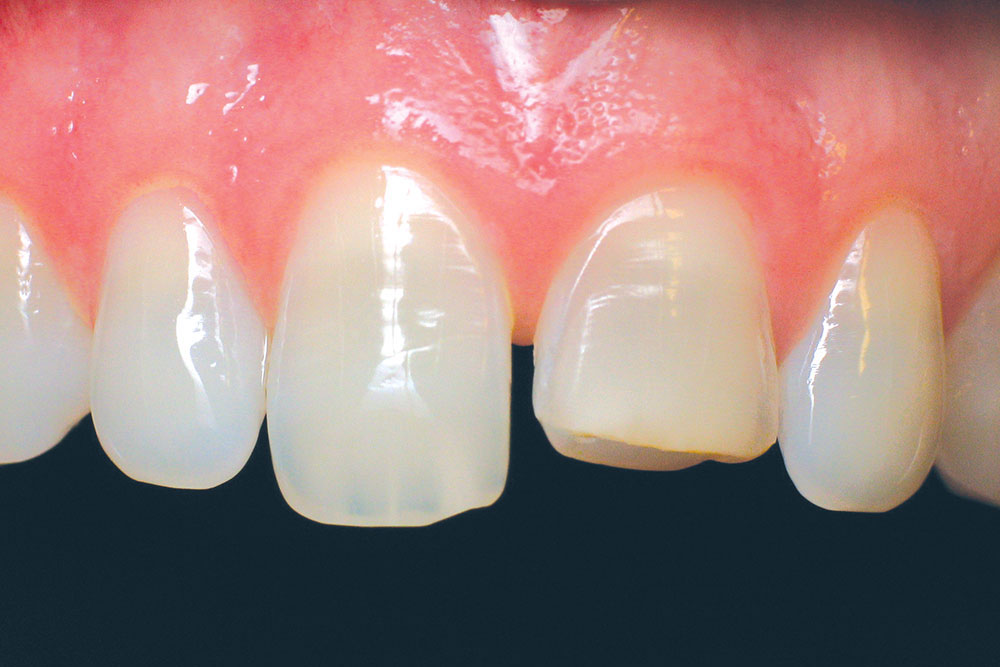
A 34-year-old male presented to our office for cosmetic consultation at the urging of his girlfriend. His major concern was to fix the chip on the mesial-incisal corner of tooth #8 and a broken tooth #9 (Figs. 3, 4). During our consultation, I inquired about his overall treatment goals. He said he wasn’t sure what he wanted and that he hadn’t given the matter much thought.
This particular case was not cut and dry, and there were multiple treatment options and things to consider. Do we close the diastema or leave it open? Do we keep the centrals at the current length or shorten them? Do we use direct composite in-office or send the case out to the lab for porcelain restorations? Does the patient want teeth whitening? These were all appropriate options, and the suitable treatment depended on the patient’s desires. Deciding on these factors would not only impact the cosmetic outcome, but also influence the clinical treatment.
At this point, I decided visual communication using digital imaging would simplify the decision-making process. Using Adobe® Photoshop® Elements (Adobe Systems; San Jose, Calif.), an off-the-shelf photo manipulation software, I completed several simulations of the various treatment options. The first simulation showed repairs made to teeth #8 and #9 using direct bonding, leaving the diastema in place (Figs. 5, 6). The second simulation showed porcelain veneers being used to repair teeth #8 and #9 and close the diastema (Figs. 7, 8). The final simulation showed the patient what his teeth would look like if he whitened them (Fig. 9).
After seeing all treatment possibilities, the patient decided to whiten his teeth followed by having porcelain veneers placed on teeth #8 and #9 that would close the diastema. The patient whitened his teeth for about two weeks and then allowed two weeks for rebound (Fig. 10).
Clinical Technique
The decision was made to utilize feldspathic porcelain veneers. Feldspathic veneers require only 0.5 mm of facial reduction and 1 mm of incisal reduction for adequate strength and beauty. Feldspathic veneers are layered and allow the characterizations and color to be built deep within the restoration. This combination yields a conservative, yet vital, result.
After achieving adequate anesthesia, the teeth were prepared using the “connect-the-dots” approach. First, a 0.5 mm depth-cutting bur (LVS1 [Brasseler USA; Savannah, Ga.]) was used to ensure minimum thickness on the facial surface (Fig. 11), and incisal depth cuts were placed to ensure minimal incisal reduction (Fig. 12). Incisal depth cuts were not necessary on tooth #9 because it was being lengthened.
Next, preparations were made for closing the diastema. When closing a diastema, the preparation margins must be placed subgingival interproximally and carried to the lingual to allow for a proper emergence profile. A two-grit diamond bur (LVS3 [Brasseler USA]) was used for final margination (Fig. 13).
Porcelain restorations require rounded preparations that are free of sharp angles and unsupported enamel. A coarse polishing disk (EP2 [Brasseler USA]) was used to round all line angles and sharp edges to ensure a smooth final preparation (Fig. 14).
For anterior cases, digital imaging can and should play a vital role in patient education and decision-making. In fact, in situations where a few teeth are being treated, its use may be even more important than for full-smile restorations.
Retraction cord was used to gently displace the soft tissue to assist in capturing the final preparation details (Fig. 15). Impressions were then taken and sent to the laboratory along with digital pictures to communicate tooth length, form, color and characteristics.
Once the restorations were received from the lab, they were verified on the solid models and then tried in the mouth with appropriate try-in gels (Fig. 16). After receiving patient approval, the restorations were bonded into place using the total-etch technique. The final result successfully accomplished the treatment goals of closing the diastema, correcting the fractures and looking natural (Figs. 17, 18).
Conclusion
Digital imaging is a powerful tool for helping patients decide which treatment option is best for them when multiple alternatives exist. It allows the dentist to visually communicate realistic results to the patient and involves the patient in the treatment decision-making process. Giving patients an active role in their treatment breaks down barriers between clinicians and their patients, leading to increased treatment acceptance.
By using an off-the-shelf digital imaging solution, the clinician can significantly lower the cost of adding this technology to their practice. This type of software is widely available, and many community colleges conveniently offer inexpensive user training courses.
Dr. Tarun Agarwal maintains a full-time private practice in Raleigh, North Carolina, emphasizing esthetic, restorative and implant dentistry. Contact him via email at dra@raleighdentalarts.com or visit raleighdentalarts.com.