Case Report: The Creation of a Soft Tissue Emergence Profile with a Long-Term Ribbond®-THM Provisional

There is an ever-increasing body of dental research literature evaluating the use of fibers to reinforce the clinical performance of dental composites and acrylics. Teeth restored with fiber posts show a significantly higher resistance to fracture than titanium1 and stainless steel posts.2 Teeth restored with fiber posts are significantly stronger in static and fatigue fracture testing than teeth restored with metallic posts,3 resulting from an elastic modulus that more closely approaches dentin, producing less concentrated stress on the root.4 Similarly, custom fiber-reinforced posts (Ribbond® [Ribbond; Seattle, Wash.]) fabricated directly into the root canal space with composite show that polyethylene fiber-reinforced posts with composite cores demonstrate high survival rates and can be recommended for use.5,6 Additionally, the insertion of Ribbond inside the cavity has a positive effect on fracture strength of endodontically treated molar teeth with MOD cavity preparation and cuspal fracture,7 as well as the ability to reinforce severely compromised teeth which have been endodontically treated.8
The use of fiber reinforcement has distinct advantages in traditional composite restorative techniques. The use of fiber under composite restorations can save the tooth structure by changing fracture lines if cusp failure should occur9 and significantly increases fracture strength of MOD composite restorations, especially if placed in a buccal to lingual direction.10 The fatigue strengths of particulate filler composite resins is 49–57 MPa, and those of fiber-reinforced composites is 90–209 MPa, with the strain of UHMWPE (ultra-high molecular weight polyethylene, i.e., Ribbond) being the highest.11 Strain energy absorption can be increased 433% over unreinforced composite, with the leno-weave reinforced composite having the highest consistency due to the details of its architecture, which restricts fabric shearing and movement during placement.12 Polyethylene reinforcing fiber, when used in combination with a flowable resin in high C-factor cavity preparations, results in stable bond strengths and an increase in the microtensile bond strength to the dentin floor.13 Another significant advantage of using fiber reinforcement in traditional Class II composite resins is the significant decrease in gingival microleakage.14
Strassler has written extensively on the benefits of fiber-reinforcing material with dental resins and has used fiber reinforcing in single-tooth replacement techniques,15 single visit, natural tooth pontic bridges16 and periodontal splinting with thin-high-modulus polyethylene ribbon.17 The high molecular weight polyethylene has a high wear resistance and high impact strength,18 with its plasma treatment resulting in chemical integration with composite resins.19 With a locked-stitched lenoweave, the fibers maintain their orientation when adapted to the tooth structure or integrated into temporization and do not unravel when cut.20 The addition of fibers to provisional resins increases the fracture toughness and flexural strength,21 with the clinical implication of a reduced incidence of fixed provisional restoration failure22 due to enhanced fracture resistance.23 Additional strengthening of the connector areas can be achieved through the use of a fiber-reinforcing material such as Ribbond®-THM (Ribbond).24 Polyethylene fiber-reinforced composite bridges can be considered as a permanent treatment due to their strength25,26 with selection of appropriate fiber reinforcement and placement of the fibers allowing long-term clinical success.27
Case Presentation
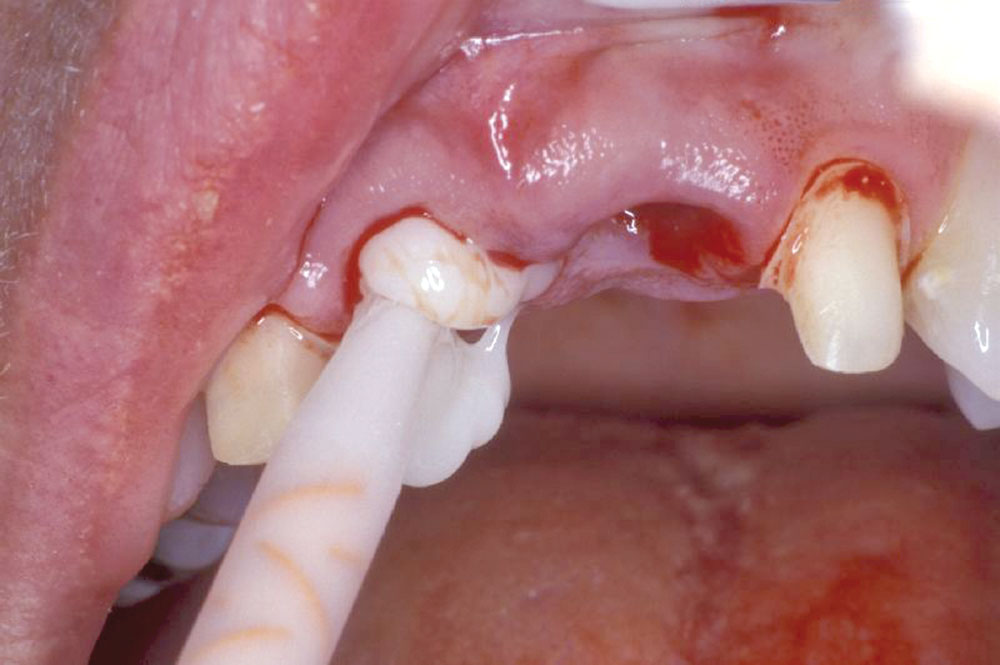
A 55-year-old patient presented to the practice with two failing upper centrals (Fig. 1). Tooth #8 had a vertical fracture and tooth #9 had a failing root canal treatment. Upon presentation of the various options to restore the area, the patient opted for placement of a 4-unit fixed bridge. The centrals were atraumatically extracted with minimal trauma to the soft tissues and alveolar process (Fig. 2). The lateral incisors were minimally prepared for the initial long-term temporization so that the gingival tissues would have an opportunity to stabilize.
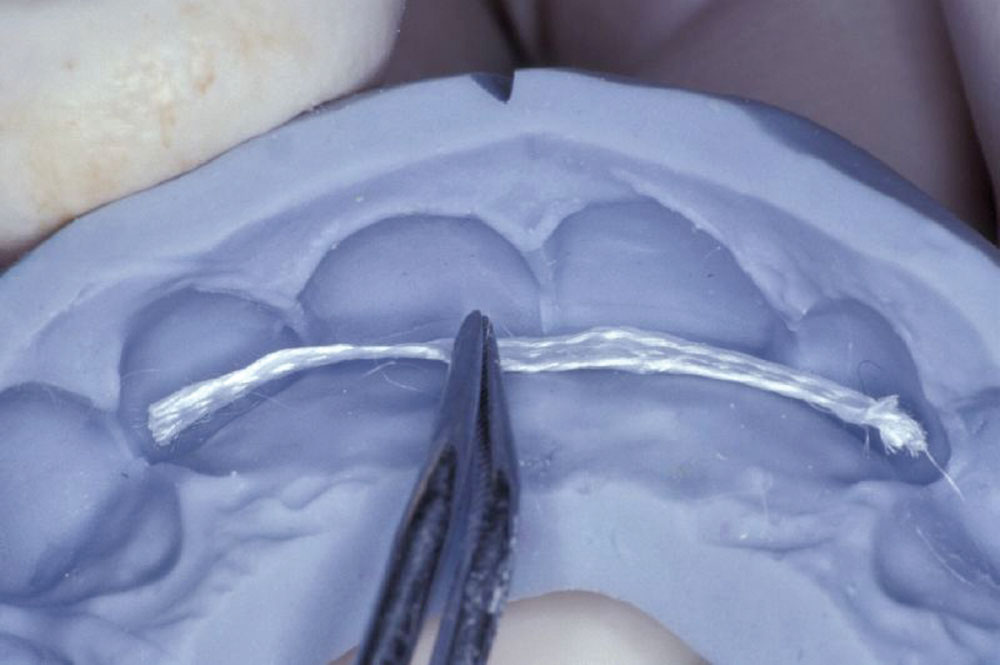
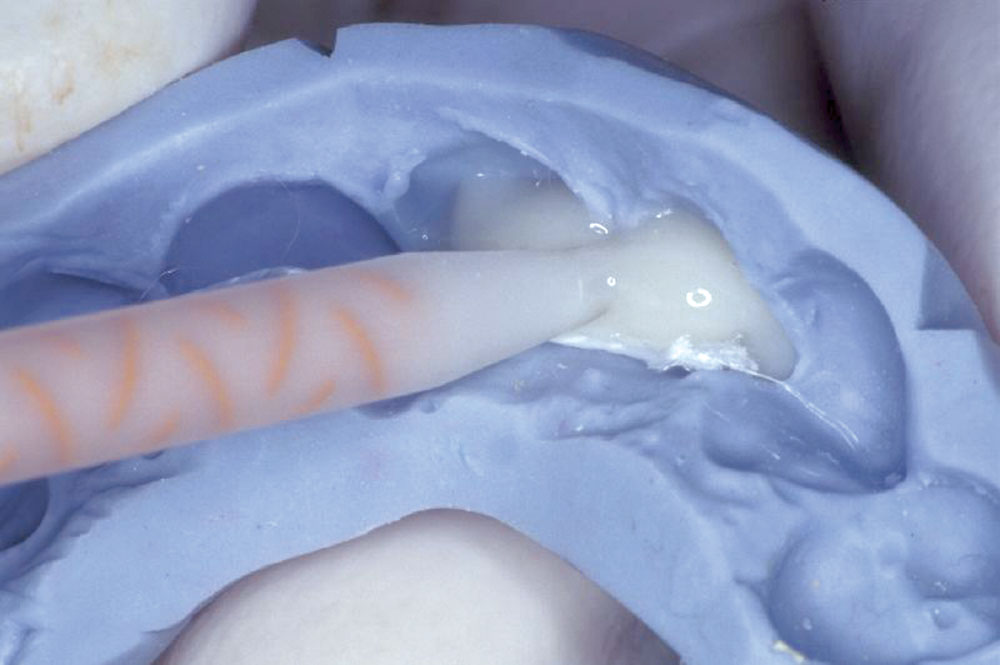
Utilizing a previously fabricated polyvinyl siloxane matrix, an appropriate length of Ribbond-THM (thinner higher modulus) was cut to extend from lateral to lateral incisor (Fig. 3). The Ribbond-THM was wetted using unfilled bonding adhesive, the excess blotted off with a lint-free gauze and the saturated Ribbond was placed onto the lingual surface of the PVS matrix, followed by injection of Temptation® (Clinician’s Choice; New Milford, Conn.) (Fig. 4). A small amount of Temptation was also placed into the extraction sockets (Fig. 5), and the PVS matrix was seated intraorally (Fig. 6).
After polymerization was complete, the matrix was removed, and the temporary bridge was removed from the matrix (Fig. 7). To create the desired soft tissue emergence profile (ovate pontic form) for the final restoration, the temporary bridge was fabricated to extend 3 mm below the free margin of the gingival tissue. The over-extension was removed (Fig. 8), and both pontics were shaped and contoured to measure exactly 3 mm from the marked position of the free margin with flowable composite (Figs. 9, 10).
Initial shaping of the temporary bridge was followed by the application of Tempglaze™ (Clinician’s Choice), which was cured with a broad spectrum curing light for 30 seconds per unit (Fig. 11). The temporary was cemented with Cling2® (Clinician’s Choice), and all temporary cement was removed (Fig. 12). After 10 weeks, the soft tissue showed excellent tissue contours, which will allow for natural-looking emergence profiles for the #8 and #9 pontics (Fig. 13).
Three additional clinical cases are presented in photo format only, to show the type of tissue response that can be created with this technique (Figs. 14–19).
Dr. Len Boksman formerly was director of clinical affairs for Clinical Research Dental and Clinician’s Choice. He currently does freelance consulting and lecturing for the general practitioner. He can be reached at lenboksman@rogers.blackberry.net.
Dr. Robert Margeas is an adjunct professor in the department of operative dentistry at the University of Iowa and a clinical instructor at the Center for Excellence® in Chicago, Illinois. He maintains a private practice devoted to esthetic dentistry in Des Moines, Iowa.
References
- ^Amenisalehi E. Strength of incisors restored by metallic, fiber and ceramic posts. J Dent Res. 2005;84 (Spec Issue B), African and Middle East section (www.dentalresearch.org).
- ^Barjau-Escribano A, Sanho-Bru JL, Forner-Navarro L, Rodríguez-Cervantes PJ, Pérez- Gónzález A, Sánchez-Marín FT. Influence of prefabricated post material on restored teeth: fracture strength and stress distribution. Oper Dent. 2006 Jan-Feb;31(1):47-54.
- ^Hayashi M, Sugeta A, Takahashi Y, Imazato S, Ebisu S. Static and fatigue fracture resistance of pulpless teeth restored with post-cores. Dent Mater J. 2008 Sep; 24(9):1178-86.
- ^Nakamura T, Ohyama T, Waki T, Kinuta S, Wakabayashi K, Mutobe Y, Takano N, Yatani H. Stress analysis of endodontically treated anterior teeth restored with different types of post material. Dent Mater J. 2006 Mar;25(1):145-50.
- ^Piovesan EM, Demarco FF, Cenci MS, Pereira-Cenci T. Survival rates of endodontically treated teeth restored with fiber-reinforced custom posts and cores: a 97-month study. Int J Prosthodont. 2007 Nov-Dec;20(6):633-9.
- ^Bae JM, Kim MJ, Jung WC, Son DK. Evaluation of the mechanical properties of experimental fiber-reinforced composite posts. Abstract #2686 IADR/AADR/CADR 85th General Session 2007 http://iadr.confex.com/iadr/2007orleans/techprogram/abstract_91891.htm.
- ^Belli S, Cobankara FK, Eraslan O, Eskitascioglu G, Karbhari V. The effect of fiber insertion on fracture resistance of endodontically treated molars with MOD cavity and reattached fractured lingual cusps. J Biomed Mater Res B Appl Biomater. 2006 Oct;79(1):35-41.
- ^Kirzioglu Z, Ertürk MS. Reconstruction and recovery of hemisectioned teeth using direct fiber-reinforced composite resin: case report. J Dent Child (Chic). 2008 Jan-Apr;75(1):95-8.
- ^Yldirim C, Kahveci O, Akman M, Belli S, Eskitascioglu G. Effect of fibre on fracture strength of teeth with MOD cavity. Abstract #0940 IADR/AADR/CADR 85th General Session http://iadr.confex.com/iadr/2007orleans/techprogram/abstract_89686.htm.
- ^Belli S, Erdemir A, Yildirim C. Reinforcement effect of polyethylene fibre in root-filled teeth: comparison of two restoration techniques. Int Endod J. 2006 Feb;39(2):136-42.
- ^Bae JM, Kim KN, Hattori M, Hasegawa K, Yoshinari M, Kawada E, Oda Y. Fatigue strengths of particulate filler composites reinforced with fibers. Dent Mater J. 2004 Jun;23(2):166-74.
- ^Karbhari VM, Strassler H. Effect of fiber architecture on flexural characteristics and fracture of fiber-reinforced dental composites. Dent Mater J. 2007 Aug;23(8):960-8.
- ^Belli S, Dönmez N, Eskitaşcioğlu G. The effect of c-factor and flowable resin or fiber use at the interface on microtensile bond strength to dentin. J Adhes Dent. 2006 Aug;8(4):247-53.
- ^El-Mowafy O, El-Badrawy W, Eltanty A, Abbasi K, Habib N. Gingival microleakage of Class II resin composite restorations with fiber inserts. Oper Dent. 2007 May-Jun;32(3):298-305.
- ^Strassler HE, Taler D, Sensi LG. Fiber reinforcement for one-visit single-tooth replacement. Dent Today. 2007 Jun;26(6):120, 122-5.
- ^Strassler H. Single visit natural tooth pontic bridge with fiber reinforcement ribbon. Tex Dent J. 2007 Jan;124(1):110-3.
- ^Strassler HE, Brown C. Periodontal splinting with a thin high-modulus polyethylene ribbon. Compend Contin Educ Dent. 2001 Aug;22(8):696-700, 702, 704.
- ^Rose RM, Crugnola A, Ries M, Cimino WR, Paul I, Radin EL. On the origins of high in vivo wear rates in polyethylene components of total joint prostheses. Clin Orthop Relat Res. 1979 Nov-Dec;(145):277-86.
- ^Rudo DN, Karbhari VM. Physical behaviors of fiber-reinforcement as applied to tooth stabilization. Dent Clin North Am. 1999 Jan;43(1):7-35.
- ^Strassler HE. Clinical materials review: fiber-reinforcing materials for dental resins. Inside Dentistry. 2008 May;5(4):76-85.
- ^Hamza TA, Rosenstiel SF, Elhosary MM, Ibraheem RM. The effect of fiber reinforcement on the fracture toughness and flexural strength of provisional restorative resins. J Prosthet Dent. 2004 Mar;91(3):258-64.
- ^Ramos V Jr, Runyan DA, Christensen LC. The effect of plasma-treated polyethylene fiber on the fracture strength of polymethyl methacrylate. J Prosthet Dent. 1996 Jul;76(1):94-6.
- ^Pfeiffer P, Grube L. In vitro resistance of reinforced interim fixed partial dentures. J Prosthet Dent. 2003 Feb;89(2):170-4.
- ^Heymann HO. The Carolina bridge: a novel interim all-porcelain bonded prosthesis. J Esthet Restor Dent. 2006;18(2):81-92.
- ^Chafaie A, Portier R. Anterior fiber-reinforced composite resin bridge: a case report. Pediatr Dent. 2004 Nov-Dec;26(6):530-4.
- ^Karakaya S, Gursel M, Ozer F. Replacement of natural teeth using fiber-reinforced restoration: clinical reports. Abstract #0330 IADR 2005 (http://iadr.confex.com/iadr/eur05/techprogram/abstract_68611.htm).
- ^Trushkowsky R. Fiber-reinforced composite bridge and splint. Replacing congenitally missing teeth. NYS Dent J. 2004 May-Jun;70(5):34-8.
Reprinted by permission of Oral Health, December 2008.