Solving Major Challenges Facing the Profession

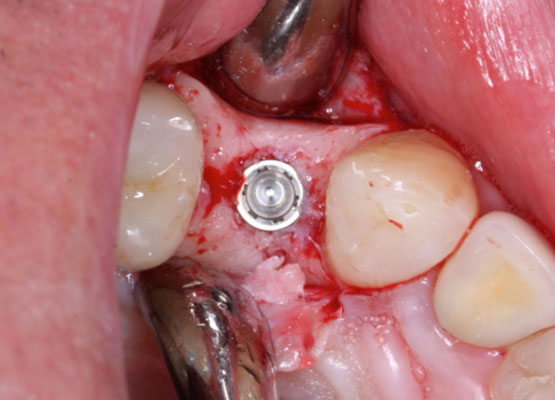
Dentistry has had astounding achievements over the past several decades. The profession has been praised for its preventive orientation and the obvious success achieved by using preventive concepts. It is possible with patient cooperation and by using several well-known preventive concepts to nearly totally prevent dental caries (Fig. 1). Newly developed dental techniques, materials and devices have made dental treatment and follow-up much easier than in the past. The introduction of implants has revolutionized the replacement and restoration of missing teeth (Figs. 2a–2c).
Digitization of many concepts and the introduction of numerous new technologies are present in every area of dentistry, making diagnosis and treatment easier, faster and often better than in the past. However, the same three major disease conditions — dental caries, periodontal disease, and pathologic occlusal conditions — are still present, and they comprise a significant part of the need for overall oral health care. The need and demand for oral disease prevention and treatment is not going away, and some important challenges threaten the ability of the profession to face these issues.
As I speak to thousands of dentists annually, they often comment on their challenges, frustrations and concerns.
This article is a candid statement of some of the major current issues facing the profession as expressed by these dentists with whom I have frequent contact. The issues are not new; they have been observable for some time. However, the urgency for solutions is new, as the grassroots dental profession is undeniably impatient with the apparent lack of resolutions to the situations. In my opinion, these challenges need immediate attention by industry leadership and dental educators.
THIRD-PARTY PAYMENT ORGANIZATIONS
Undeniably, there are some positive characteristics of third-party payers. Some groups of patients can receive oral care that they otherwise would not have been able to afford (Figs. 3a, 3b). Specific third-party payers have contributed heavily to dental education and research, and their presence and their altruism have brought observable attention to oral health.
However, wherever I meet with dentists, third-party payment companies receive more vehement negative discussion than any other topic. The dentist complaints are well known and expressed routinely. A few of the most common complaints are:
Wherever I meet with dentists, third-party payment companies receive more vehement negative discussion than any other topic.
- Some payment plans do not even compensate procedures enough to cover office expenses.
- Often inexperienced and uneducated insurance-company employees dictate treatment to dentists.
- Allegations of dentist dishonesty are leveled at dentists from the third-party payers.
- Although quality of care varies considerably among dentists, it is not acknowledged by some companies (Figs. 4a–5b).
- Dentists are frustrated with being told what they can charge patients regardless of the quality they produce or the difficulty of a procedure or patient. A Class II resin is not a Class II resin (Figs. 6a, 6b), and a denture is not a denture; yet dentists receive the same payment.
The list of dentist complaints regarding third-party payment companies could comprise an entire book.
There is another significant third-party challenge that appears to be a growing trend. The American Dental Association reports that the typical overhead costs for general dentists are about 61% of their gross revenue. This is a large percentage of gross dentist revenue that cannot be reduced significantly without sacrificing the quality of prevention and treatment.
However, in recent months some third-party payers have reduced their payments for oral procedures. While overhead expenses remain the same, payments for procedures are being reduced, and the net income to dentists is proportionately reduced. Dentists have no alternative other than to find ways to reduce costs to maintain sufficient net income, and reduction of oral-care quality is unfortunately the result. Although the ability of third-party payers to change their policies at will is obvious, dentists have little or no ability to adapt to the changes.
What should be done?
Dental association leaders and practitioner organizations must establish immediate candid communication with third-party payers, and they must work together to overcome the obvious challenges the companies are clearly producing. It is apparent that the third-party situation is in an explosive state. This topic is by far the most irritating and negative situation in the profession. It needs immediate attention, and equitable solutions must be found. If this is not done soon, a grassroots practitioner rebellion, already stirring, will occur.
CORPORATE DENTISTRY ORGANIZATIONS
These organizations have existed for many years, but they have expanded rapidly recently. The quality and goals of the organizations vary immensely. Some are clearly money oriented. Others are the opposite. There are highly organized companies with their own educational programs for their doctors, functional quality control programs, and up-to-date equipment and facilities. Those organizations that are trying hard to improve the reputation of corporate dentistry are to be congratulated.
Young dental graduates have education debts of $200,000–$400,000. The breadth of knowledge in dentistry has made dental educators spend fewer hours on many of the concepts and techniques that were taught more in-depth in the past. The result is that many new graduates need clinical experience. Corporate dentistry organizations provide experience for these dentists, as well as a location for many mature dentists who favor this type of practice.
Many solo practicing dentists are concerned about the growing presence of corporate dentistry. The ability of corporations to purchase supplies and equipment in quantity reduces their overhead costs, can lower fees for patients, and increases competition for solo practitioners.
What should be done?
As with almost any concept or topic, good and not-so-good characteristics are observable in corporate dentistry. There are great corporate companies as well as companies that need to change for the better. The Association of Dental Support Organizations has made suggestions directing corporate dentistry companies to have standards that ensure high-quality dentistry and ethical policies. Corporate dental practice organizations should abide by those recommendations. They should also ensure that their members integrate with private dentists in their communities, and that they are involved in organized dentistry at all levels.
OVERPRODUCTION OF DENTISTS AND DENTAL HYGIENISTS
I seldom speak in a U.S. dental community where the dentists claim they do not have an adequate quantity of dentists or dental hygienists. Yet we see a continuing movement by some groups to not only produce more dentists, but also initiate the concept of so-called midlevel practitioners. Additionally, many new dental schools have been started in recent years, and more are in the planning stages. Some of these new schools are producing dentists in geographic areas that do not need more dentists, thus increasing the problems of already-struggling dentists. What is the result when an overabundance of dentists or dental hygienists is produced in a community? Competition abounds. Referrals to specialists are reduced. Many general dentists accomplish clinical tasks that could be better done by specialists. Advertising increases. Quality of care is sacrificed. Some dentists go bankrupt!
Do dentists in saturated areas go to areas of need, which is the goal of some who support overproduction of dentists or development of midlevel practitioners? Any practicing dentist recognizes that this does not happen. Generally, dentists and hygienists stay in the areas in which they want to live. History has proven that point.
What should be done?
The American Dental Association has the responsibility to help provide adequate and qualified dental manpower across the U.S. However, it also has the responsibility to its members to help provide a realistic and needed quantity of dentists for specific geographic areas. Although this is an idealistic suggestion, the ADA dental education accrediting council should make strong suggestions to those attempting to start schools in saturated areas to not do so.
Areas of need are a public health challenge. State or national funds should be appropriated to build clinics and hire dentists and dental hygienists for areas of need.
Another suggestion is to require at least one year of service for all new graduate dentists and hygienists in state or federal clinics in areas of need. After personal long deliberation and frustration on this topic, I do not see any other solutions.
CLINICAL TEACHING AND LEARNING IN DENTAL SCHOOLS
After decades of teaching “hands-on” courses for new graduates and dentists of all ages, I currently see a wide disparity in the clinical ability of new graduates from schools in the U.S. (Figs. 7, 8). Some have good beginning clinical skills, while others appear to be woefully underprepared. In my clinical courses, I can easily identify the schools of the underprepared graduates.
As a previous full-time dental educator and administrator for many years, I fully understand the difficulty of elevating all graduating students to an acceptable beginning competency level. I also understand the need to include the many topics now necessary in dental curricula that were not previously necessary.
What should be done?
The administrators of dental schools should be competent clinicians who understand current dental practice and know the necessity for quality clinical services. Also, as a requisite but secondary characteristic, administrators should have an understanding and respect for the presence of dental research in their schools. Both clinical expertise and research knowledge are necessary. I see some current administrators of dental schools who are competent researchers but who do not understand or respect clinical practice.
Research can bring grant money into schools, and for that reason it is in vogue for schools to hire administrators who are researchers. As a clinician, researcher and educator for several decades, I contend that research in dental schools should support clinical teaching. It should not dominate the dental school curriculum. Broadly based clinician/researcher administrators know that acquiring physical skills, such as clinical dentistry, requires knowledgeable clinical teachers and significant student repetition of the skills to achieve competency.
SUMMARY
Dentistry ranks as the No. 1 occupation in the 2015 Best Jobs analysis by U.S. News & World Report.1 Most dentists love their profession. However, there are significant challenges that must be overcome for the profession to remain in high esteem and to attract high-quality students. The topics I have indicated that need attention are only a few that are readily apparent. Solutions to each of these issues require proactive thought and action. The challenges will not solve themselves. Undoubtedly, the suggestions I have made in this article could be added upon by each of you reading it.
There are significant challenges that must be overcome for the profession to remain in high esteem and to attract high-quality students.
Stay in Touch with Dr. Christensen Online
Visit Gordon on Facebook at facebook.com/GordonJ.Christensen, follow him on Twitter @GoJChristensen, or go to pccdental.com for the latest news on CE courses, clinical video demonstrations and practice management tips.
References
- ^100 Best Jobs of 2015. U.S. News & World Report. http://money.usnews.com/careers/best-jobs/rankings/the-100-best-jobs. Accessed April 14, 2015.