Minimally Invasive Dentistry Combined with Laser Gingival Plastic Surgery: Maximize Your Aesthetic Results

In order to design the optimal outcome for a patient during aesthetic enhancement, the restorative dentist must seek to create a symmetrical and harmonious relationship between the lips, the gingival architecture and the positions of the natural dentate forms. In the author’s experience, the WaterLase® YSGG laser (BIOLASE Technology, Inc.; Irvine, Calif.) has been a useful adjunct for performing aesthetic surgical crown lengthening procedures. This article will highlight the associated biological principles and demonstrate techniques for the application of this laser in closed and open crown lengthening procedures in conjunction with the use of porcelain veneers for aesthetic dental reconstructions.
The Dentogingival Complex
The dentogingival complex consists of a connective tissue attachment, an epithelial attachment (or junctional epithelium) and the gingival sulcus. As described by Spear1 and Kois2, the most critical relationship for biologic health, when the clinician is placing a restoration at or below the free gingival margin (FGM), is the margin location relative to the crest of bone. Kois states that the distance from the FGM to the osseous crest on the facial aspect is 3.0 mm. Interproximally on anterior teeth, this distance is 4.0 mm due to the curvature of the cementoenamel junction. The height of the interdental papilla can also be predictably maintained at 4.0 mm incisal to the osseous crest between anterior teeth with normal root proximity, approximately 2.0 to 3.0 mm at the osseous crest. With these parameters in mind, the clinician must first decide where the restorative margin will be placed. With all-ceramic restorations, if one does not have to block out undesirable dentin colors or core materials, then it may be desirable to place the restorative margin at the free gingival crest or even slightly supragingival. However, if an intracrevicular margin is required for aesthetic reasons, it should be placed no further than 0.5 mm into the gingival sulcus to avoid adverse biologic responses due to encroachment upon the attachment apparatus. Kois and Coslet, et al.3 also describe a variation in biologic width that compares the distance from the alveolar crest to the FGM and divide this into three categories: normal crest, high crest and low crest. In simplified terms, normal-crest patients (about 70%) have approximately a 2.0 mm combined epithelial and connective tissue attachment and 1.0 mm average sulcus depth. If the sulcus depth is greater than 1.0 mm, the free gingival excess can be safely resected and upon healing will result in a dentogingival complex measuring 3.0 mm on the facial aspect. Patients with a high crest often have a shallower sulcus depth and a combined epithelial and connective tissue attachment of less than 2.0 mm. These patients have relatively stable FGM positions and are not prone to recession upon manipulation of the tissues. Low-crest patients often have normal sulcus depth (1.0 mm to 3.0 mm) and a combined epithelial and connective tissue attachment that is less than 2.0 mm. These patients are highly prone to recession and must be treatment planned accordingly. The FGM of low-crest patients will tend to apically reposition and turn into a normal-crest situation after gingival retraction or surgery. Therefore, the most important factor in achieving post-restorative gingival health and stability is the position of the restorative margin relative to the bony crest, not the preoperative health and/or the position of the gingival tissues.
If diastemata are present, the interproximal margin of the preparation should be carried lingually to the linguoproximal line angle and be placed slightly intracrevicularly in the proximal area to help “squeeze” the gingival papilla.
Smile Design and Tooth Dimension
Several parameters must be considered when designing an aesthetic smile. These include the width-to-length ratio of the maxillary central incisors; the mesiodistal proportional width of the maxillary anterior teeth; the position of the maxillary central incisors in the face (i.e., the E position); and the relative gingival-zenith positions along with the height of contour. The width of the average maxillary central incisor has been measured at approximately 10.0 mm. Utilizing the Golden Proportion as a guideline, one can arrive at an appropriate measurement for the width and length of the central incisor. Because the width-to-length ratio of an aesthetic maxillary central incisor is 75% to 80%, a 10.0 mm central incisor, if it is proportionally correct, should measure 7.5 to 8.0 mm mesiodistally. The E position (when a patient says E as a long vowel) shows the relative amount of maxillary tooth display. In the E position, it is aesthetically desirable for a patient to show 50% to 70% of the maxillary incisor teeth. Finally, the height of the gingival tissues over the maxillary central incisors should be slightly higher (1.0 mm apically) than the height of the tissue over the maxillary lateral incisors.
The height of the maxillary canines should be at the same level apically as the central incisors, or slightly more apical. The gingival zeniths should be located at the distolabial line angles, thus creating a “raised eyebrow” over the central incisors.
Laser-Assisted Crown Lengthening
Use of the WaterLase YSGG laser for gingival and bony recontouring has had a tremendous impact on the way periodontal surgery is performed. Because the laser cuts only at the end of the tip, the user has effective control of both soft- and hard-tissue resection. Using the YSGG with a tapered tip allows the operator to make scalloped gingivectomies with surgical precision and no bleeding. When using traditional rotary instruments to perform osseous resection, there is always a risk that their rotation will damage adjacent root surfaces. Additionally, because the surgical laser wound is less traumatic, there is less chance of bony damage due to frictional heat, which is always a problem when using rotary instrumentation without proper irrigation. This minimally invasive technology translates into less postoperative discomfort and quicker healing.
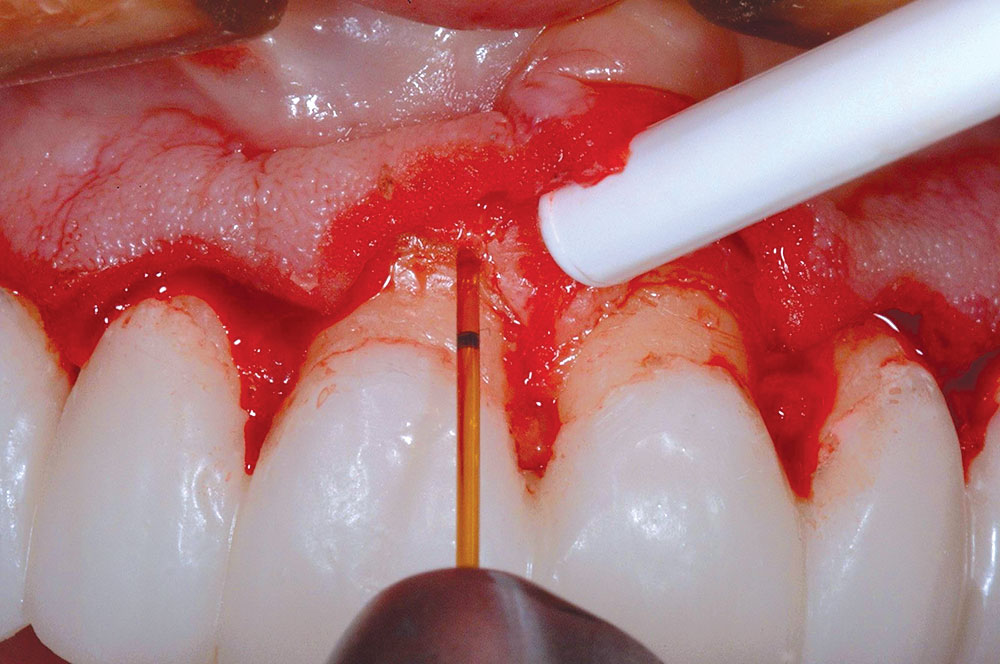
The Open Technique
For an aesthetic gingival display, it is critical that symmetry (right and left) exists as it relates to cervicoincisal tooth height and gingival zenith positions. Patients that exhibit asymmetrical gingival levels, or those with greater than 3.0 mm of maxillary gingival display, or both, may be candidates for surgical gingival and/or alveolar bone repositioning to improve their aesthetics. Typically, these patient types have adequate amounts of attached gingiva so that after the resective procedure the mucogingival junction will not be encroached upon. If adequate amounts of free gingiva exist, minor asymmetries can be corrected with gingivectomy or gingivoplasty alone. A minimum sulcus depth of 1.0 mm must always remain after any tissue resection unless the alveolar bony crest is also repositioned in the apical direction as well. To give the appearance of spatially moving teeth in the cervical direction to alleviate excessive gingival display or asymmetry, often an osseous correction must be performed in conjunction with soft-tissue resection because of sulcus depth violation. As previously stated, the finished maxillary central incisors should be 10.0 to 12.0 mm in length. While the incisal edges can be shortened when adequate freeway space exists posteriorly, the amount depends on the patient’s pattern of disclusion. The shortened incisal edges must still disclude the posterior teeth in all eccentric movements to maintain occlusal harmony. A tissue markercan be used to plan the soft-tissue surgery (Figs. 1, 2). Following the guidelines for aesthetic tissue levels, the perceived final gingival level is traced, thus creating the heights of contour at the distolabial line angles. The YSGG laser is used to remove the gingival tissue and to create symmetry according to the proposed surgical plan. The preparation margins are then adjusted to the corrected FGM. As the biologic width will be encroached upon, it is important that the same amount of bone be removed to recreate normal biologic parameters. An intracellular internal bevel incision is made, and a full-thickness mucoperiosteal flap is elevated. The alveolar crest correction is made using the YSGG laser and either a Z-14 600-μm or a 9 mm 600-μm tip. Because the laser only cuts at the tip, it is set against the side of the root, parallel with the long axis of the tooth (Fig. 3). This ensures that the dentin/cementum surface is never damaged. A black marker can be used to place a line at a point 3.0 mm from end of the tip. This is used as a guide to apically position the bone 3.0 mm from the restorative margin. Only the alveolar bone will be ablated by the laser-energized water. The root surface is then planed using a back-action chisel. The alveolar architecture should thus mimic the restorative margin 3.0 mm apically, allowing for biologic width restoration to a normal crest position. (The interproximal bone on facial aesthetic correction cases is not altered.) The flap is then sutured back using 3-0 silk and an interrupted suture technique. At the delivery appointment, the heights of the gingival zeniths above the maxillary central incisors are adjusted apically using a closed crown lengthening technique. The definitive restorations are shown three years after corrective gingival and bony surgery with the YSGG laser (Fig. 4).
The Closed Technique
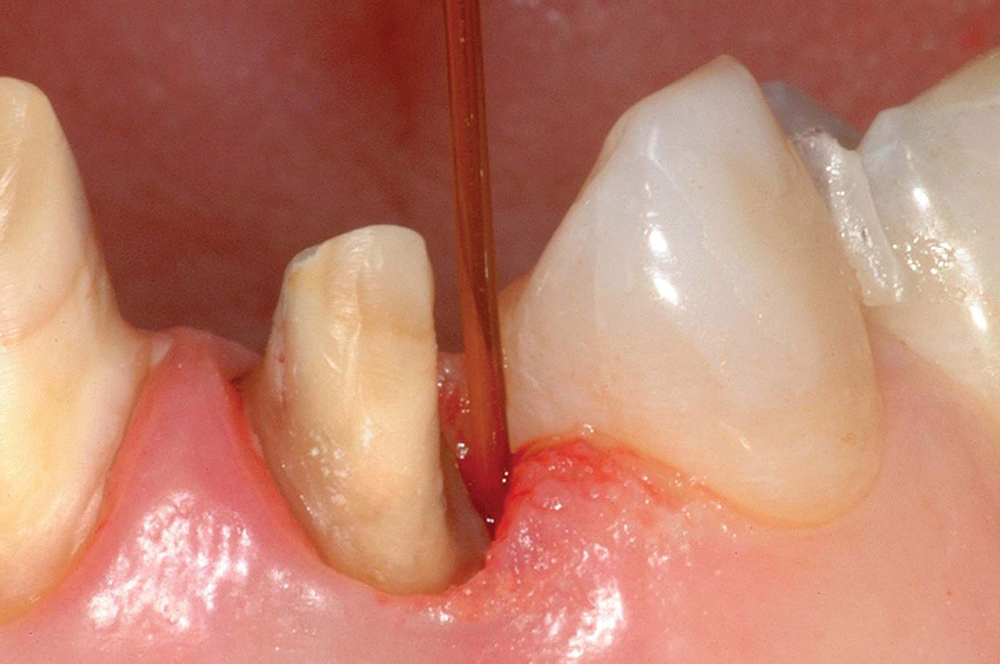
For minor, localized biological width and/or aesthetic gingival zenith corrections, the YSGG laser can be used in lieu of a flap procedure to make the correction and complete the restorative process. This can be done without the necessary healing time required for open crown lengthening surgeries. Patients with normal or thick biotypes (i.e., normal to thick keratinization) are good candidates for this procedure. The soft tissue is resected using a 400-μm tapered tip on facial areas or a 600-μm tip in proximal areas, creating the new apical position and scallop of the FGM. The osseous crest is sounded using a periodontal probe to determine the distance from the free gingival crest. Using a 9 mm 600-μm tip, the laser is then used to remove bone, holding the tip adjacent to the tooth and “walking” the tip across the affected area using a “sewing machine” (up and down) movement to a 3.0 mm depth (Figs. 5, 6). After establishing the corrected crestal level, the bone is “smoothed” by setting the laser at 50 pulses per second and moving the tip in a horizontal direction over the crestal bone. It is important to note that with both of these movements the tip of the laser is in contact with the bony crest. Next, a periodontal probe is used to verify depth by sounding to 3.0 mm. For interproximal biologic width corrections, the tip of the laser can be angled away from the tooth, slightly toward the adjacent root to blend adjacent bone and avoid digging a trench around the tooth. A final impression can then be made and provisional restoration fabricated and cemented to place. The definitive restoration can be seated two to three weeks after the closed crown lengthening procedure. The surgical area will heal by secondary intention around the finished restoration with ideal tooth contours, unlike with an ill-fitting temporary restoration. The criteria for clinical health of the dentogingival complex are a pink color demonstrating the absence of inflammation, re-establishment of a probable gingival sulcus, and the absence of bleeding upon probing (Fig. 7).
Tooth Preparation for Porcelain Veneers
The amount of tooth reduction required depends on the specific clinical situation. In general, 0.5 to 0.7 mm of tooth reduction is needed. If changes in tooth position are required, some areas of the tooth may be prepared more, others less. It is recommended first to contour the teeth to ideal position using a cylindrical diamond, and then to use depth cutters to remove a uniform amount of tooth structure to compensate for the thickness of the restoration. In extreme situations, if the dental pulp is encroached upon, root canal therapy is recommended rather than choosing to overcontour the final restoration. In cases where a low value (dark) preoperative tooth color is to be changed to a high value (light) color, more tooth structure should be removed (1.0 to 1.5 mm) to create enough space for opacious dentin and/or opaquers to block out the underlying darkness. In general, indirect labial veneers are so thin that the underlying tooth color and luting cement may influence the final shade of the restoration. For some patients, preoperative tooth whitening may be indicated to increase the value of the underlying tooth structure, allowing for less tooth structure to be removed during the preparation process. Gingival margins should be placed at the gingival crest, or slightly above. The interproximal margins should be carried into the lingual portion of the contact area. If diastemata are present, the interproximal margin of the preparation should be carried lingually to the linguoproximal line angle and be placed slightly intracrevicularly in the proximal area to help “squeeze” the gingival papilla. Also, when closing spaces, it is important to prepare the gingival margins far enough into the proximal areas so that the restoration margins are not visible from a three-fourths or oblique view, when the patient turns the head to the side. After the preparations are finished, it is recommended to use a fine finishing diamond to make the preparations as smooth as possible. An Enhance® point (DENTSPLY Caulk; Milford, Del.) can also be used to round and smooth the corners and line angles. Fine sandpaper strips can be used interproximally to smooth interproximal enamel surfaces without compromising the proximal contact (Figs. 8–10).
“Minimally invasive”; also applies to a standard of restorative excellence that allows a case to have aesthetic and functional longevity, so that the teeth are not continually assaulted and ”reprepped to death”.
The Definitive Aesthetic Restoration
One key to optimal aesthetics is the creation of the correct gingival and bony architecture in order to properly “frame” the teeth. This concept, combined with naturallooking ceramic restorations that are the minimal thickness required for structural strength and aesthetic beauty, results in an outcome that is truly magnificent while being minimally invasive. Shavell4 once said, “Many teeth are sacrificed on the altar of ‘false’ conservatism.” Is it really more conservative (minimally invasive) to use a no-prep technique, creating overcontoured teeth and the potentially negative periodontal ramifications? On the other hand, it is definitely not necessary to over-reduce teeth with no apparent rhyme or reason as a short-cut approach to restorative dentistry.
Conclusion
Each case must be evaluated for the aesthetic end result (shade) and amount of tooth reduction necessary to create aesthetic contours and occlusal (functional) harmony. “Minimally invasive” also applies to a standard of restorative excellence that allows a case to have aesthetic and functional longevity, so that the teeth are not continually assaulted and “reprepped to death.” The use of excellent dental materials, precise technique and steadfast attention to biologic principles allows the restorative dentist to create minimally invasive, naturally aesthetic dental restorations that can withstand the test of time (Figs. 11, 12).
To contact Dr. Robert Lowe, call 704-364-4711, email boblowedds@aol.com or visit destinationsmile.com.
References
- ^Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006 Feb;137(2):160-9.
- ^Kois JC. Altering gingival levels: the restorative connection, part 1: biologic variables. J Esthet Dent. 1994;6(1):3-9.
- ^Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977 Dec;70(3):24-8.
- ^Shavell HM. Extreme occlusal makeover: a morphoaesthetic approach to the dynamics of occlusion. Presented at The Holiday Dental Conference, Charlotte, NC, December 1, 2005.
Reprinted with permission of Dentistry Today. Copyright ©2009 Dentistry Today.