Source: Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2017 [internet]. 2018 Dec [cited 2021 Oct 21].
Headache and Migraine Dental Therapy Explained
Learn how to treat patients in your practice who present with recurring headaches.
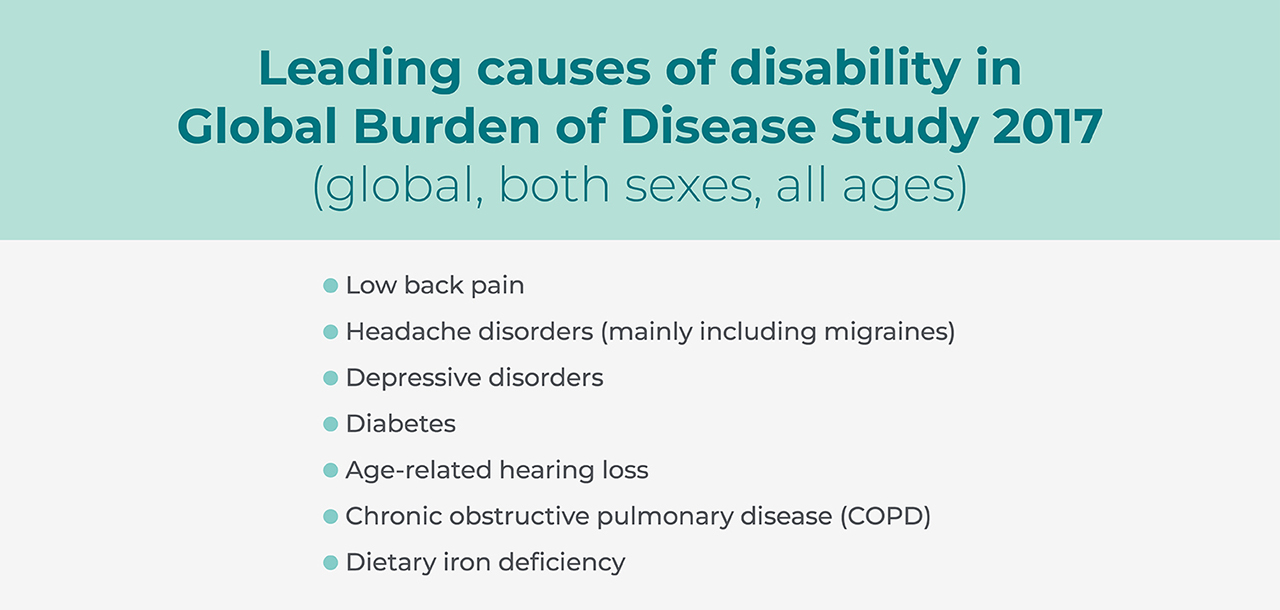
A 2018 report by The Lancet found that almost three billion individuals were estimated to have had a migraine or tension-type headache in 2016. Similarly, the National Institute of Health has shown that untreated migraines account for one of the top 20 causes of disability worldwide, and The Journal of Headache and Pain has identified migraines as the leading cause of disability for people under 50. This analytical data has transformed clinicians’ understanding of the impact of headache and migraine treatments around the globe.
For a disorder so prevalent among billions of people, the lack of care received for headaches and migraines is astonishingly low. The Eurolight report data depicts an alarming trend among 1,175 participating patients in 10 countries reporting migraines on more than five days per month. Only 20% had consulted a health care professional. In most countries, less than 10% were receiving acute treatment, and an even smaller number were receiving preventive treatment.
Our understanding of how to classify headaches and migraines is incomplete and varies from clinician to clinician. In this article, I will define the various symptoms and definitions of headaches, the impact of chronic pain, and the dental treatment for chronic tension headaches and migraines.
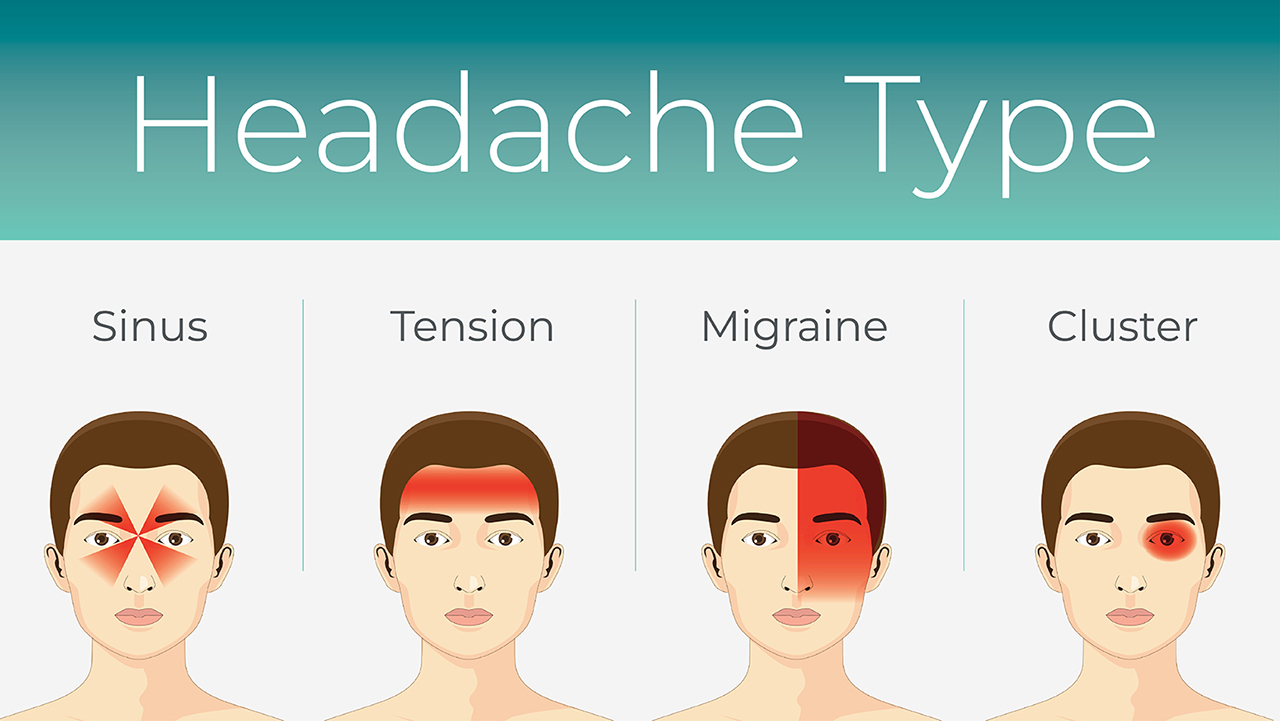
Sinus Headaches
Sinus headaches can be extremely painful and debilitating. Patients often report that sinus headaches follow long periods of nasal congestion due to allergies or colds. Some common symptoms include:
- Pain, pressure, and fullness in the cheeks, brow or forehead
- Worsening pain when bending forward or lying down
- Stuffy nose
- Fatigue
- Achy feeling in the upper teeth
Should these symptoms worsen, professional help should be sought. For example, if the patient has headache symptoms that occur more than 15 days a month, requires frequent over-the-counter pain medicine, or misses school or work, they should reach out to their health care provider.
Treatment options include home remedies like ginger, which contains organic anti-inflammatory compounds that reduce swelling in the sinuses during a sinus headache and can be helpful for sinus headaches that are coupled with a sore throat or cough. Flushing the nasal passages with a saline solution or warm water can help clear blockages and provide an anti-inflammatory effect. This can be done with a simple, gravity-fed nasal wash system or a saltwater spray that serves as an anti-inflammatory agent. Lastly, a warm compress or steam from a hot shower can help nasal inflammation and encourage nasal passage drainage.
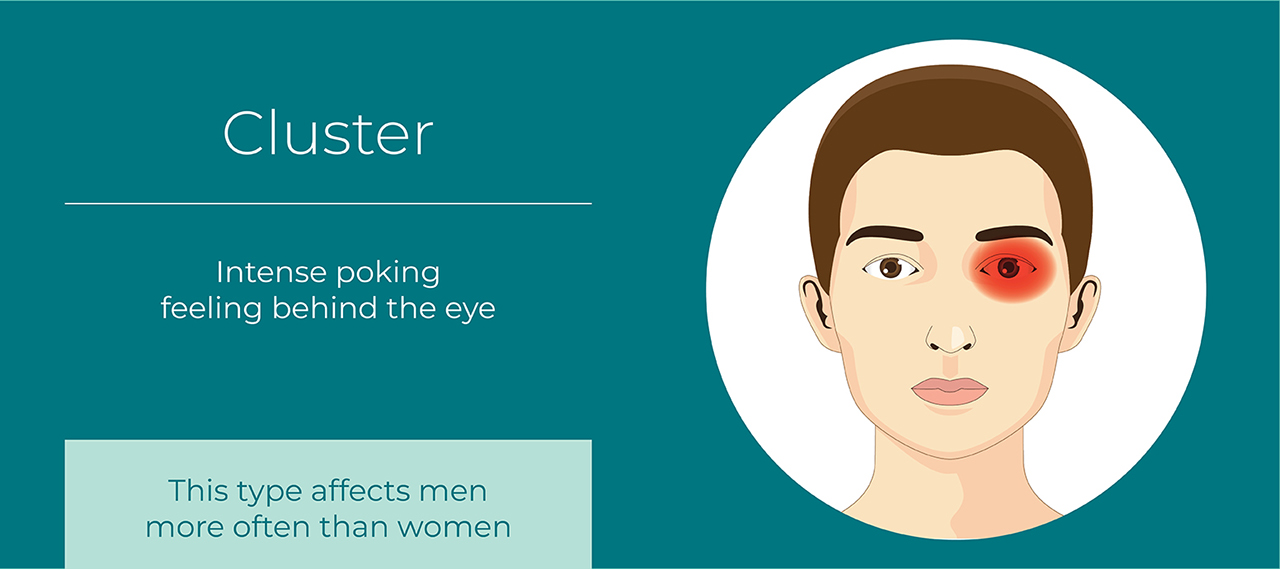
Cluster Headaches
Cluster headaches, which occur in cyclical patterns or cluster periods, are one of the most painful types of headache. A cluster headache can wake a patient up in the middle of the night with intense pain in or around one eye. Bouts of frequent attacks (15–30 per day, lasting 15–30 minutes), known as cluster periods, can continue from weeks to months, usually followed by remission periods when the headaches stop. During remission, no headaches occur for months and sometimes even years. Common signs and symptoms during a cluster headache include:
- Excruciating pain that is generally situated in, behind or around one eye, but may radiate to other areas of the face, head and neck
- Restlessness
- Excessive tearing
- Redness or swelling of the eye and stuffy or runny nose on the affected side
- Forehead or facial sweating on the affected side
- Pale skin or flushing of the face
- Drooping eyelid on the affected side
Fortunately, cluster headaches are rare and not life-threatening. Treatments can make cluster headache attacks shorter and less severe. In addition, medications can reduce the number of cluster headaches. People with cluster headaches, unlike those with migraines, are likely to pace or sit and rock back and forth. Some migraine-like symptoms — including sensitivity to light and sound — can occur with a cluster headache, though usually on one side.
Patients should see a doctor if they have just started to have cluster headaches in order to rule out other disorders and to find the most effective treatment. Headache pain, even when severe, usually isn't the result of an underlying disease. But headaches can occasionally indicate a serious underlying medical condition, such as a brain tumor or rupture of a weakened blood vessel. Additionally, if a patient has a history of headaches, they should see their doctor if the pattern changes or the headaches suddenly feel different.
Although there is no cure for cluster headaches, there are some fast-acting treatments that headache physicians may prescribe, including oxygen, local anesthetics and certain triptan medications. Potential preventive measures include using calcium channel blockers or corticosteroids.
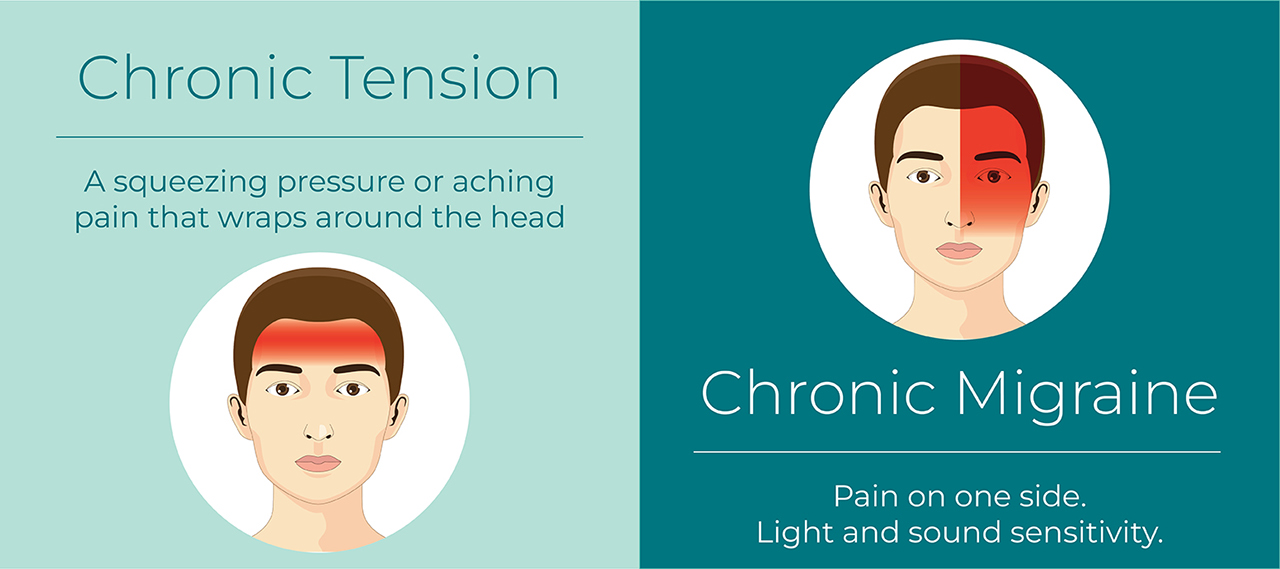
Tension Headaches and Migraines
Tension-type headaches can be difficult to distinguish from migraines. Unlike some forms of migraines, tension-type headaches are not usually associated with visual disturbances, nausea or vomiting. Although physical activity typically aggravates migraine pain, it does not make tension-type headache pain worse. An increased sensitivity to either light or sound can occur with a tension-type headache, but this symptom is not common. More common symptoms include:
- Dull, aching head pain
- Sensation of tightness or pressure across the forehead or on the sides and back of the head
- Tenderness in the scalp, neck and shoulder muscles
There are two main categories of tension-type headaches: episodic and chronic. Episodic tension-type headaches can last from 30 minutes to a week. Frequent episodic tension-type headaches occur less than 15 days a month for at least three months. If headaches occur 15 or more days a month for at least three months, they are considered chronic.
Migraines with aura (also called “classic migraines”) are recurring headaches that strike after or at the same time as sensory disturbances, which are called “aura.” These disturbances can include flashes of light, blind spots, vision changes, or tingling in the hands or face. Treatments for migraines with aura and migraines without aura (also called “common migraines”) are usually the same. You can try to prevent migraines with aura with the same medications and self-care measures used to prevent other types of migraines.
Migraine aura symptoms include temporary visual or other disturbances that usually strike before the more painful migraine symptoms — such as intense head pain, nausea, and sensitivity to light and sound — begin to occur. Aura usually occurs within an hour before head pain begins and generally lasts less than 60 minutes. Sometimes migraine aura occurs without an accompanying headache, especially in people aged 50 and older. Most people who have migraine with aura develop temporary visual signs and symptoms, which can interfere with the field of vision. These might include blind spots (scotomas), zigzag lines that gradually float across their field of vision, shimmering spots or stars, changes in vision or vision loss, or flashes of light.
If tension-type headaches disrupts a patient’s life, or if they need to take medication for their headaches more than twice a week, a patient should seek professional help. Even if a patient has a history of headaches, they should still see their doctor if the pattern changes or the headaches suddenly feel different.
Thankfully, dental offices can prescribe a preventive treatment for the pervasive symptoms of tension-type headaches and migraines that are related to jaw clenching. The NTI-tss Plus® is a simple anterior point-stop discluding device that reduces the maximum clenching power of the muscles of mastication by approximately 70%. The nociceptive input produced by the over-activity of these muscles, specifically the temporalis, has been found to be a significant contributor to tension headaches and migraines. It is indicated for patients who experience possible symptoms of tension-type headaches, migraines, TMD, tooth wear from clenching, or muscle pain associated with parafunction.

The NTI-tss Plus therapeutic protocol has proven to be an effective pathway to treating and preventing migraines. In one study, its efficacy was demonstrated to be comparable to widely prescribed pharmacological treatments without unwanted side effects. In an FDA clinical trial, 82% of individuals diagnosed with migraines experienced a 77% reduction in migraine events when using the NTI-tss Plus. Given this information, the NTI-tss Plus is likely underutilized by the migraine population and can be an excellent adjunctive treatment supplied by the dental provider.
Conclusion
While sinus headaches and cluster headaches require different forms of treatment and prevention prescribed by a headache physician, tension-type headaches and migraines related to parafunction can be treated directly by any dental physician. Having the ability to get patients out of debilitating pain is an incredible opportunity to help others and grow your practice. With the NTI-tss Plus and the NTI OmniSplint®, dental clinicians can do just that.
NTI-tss Plus is a registered trademark of Boyd Research, Inc. NTI OmniSplint is a registered trademark of James Boyd.
More to Know
Send blog-related questions and suggestions to hello@glidewell.com.