Dental CE
- Free online CE course by Suzanne R. Mericle, DMD: “Incorporating Dental Sleep Medicine Into Your Practice”
Snoring and Sleep Apnea Article
- Randy Clare, Glidewell: “Thick Neck? Snoring? Think Sleep Apnea”
800-854-7256 USA
Snoring affects the health of the mother-to-be and baby. Learn how dentists can help.

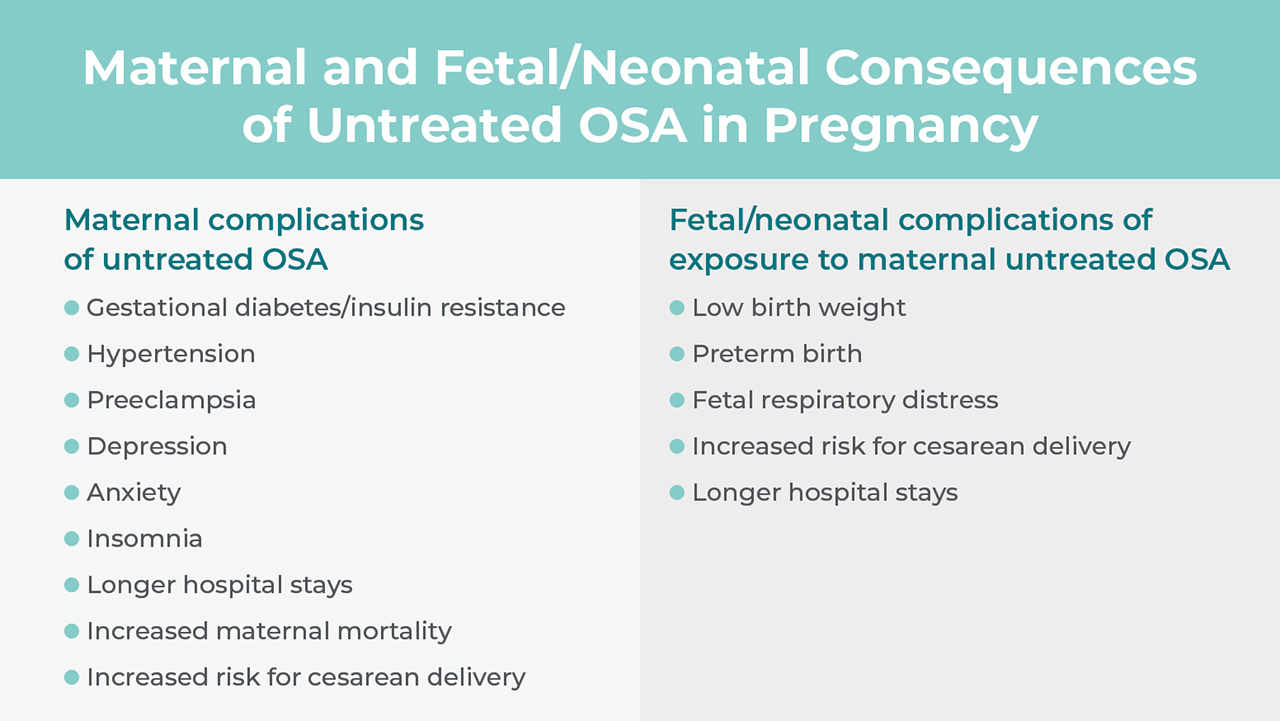
Snoring is the most obvious symptom of sleep-disordered breathing (SDB), and snoring and obstructive sleep apnea (OSA) during pregnancy are very common issues, particularly in the third trimester. Recent studies have shown that babies born to mothers suffering from SDB tend to be smaller for their gestational age when compared with children born to mothers who do not snore. Research has also shown that expectant mothers who snore are sleepier during the day and more likely to have cesarean sections compared to non-snoring expectant mothers.
Source: Rizvi S, Awwad M, Choudhry N, Khan SS. Obstructive sleep apnea in pregnancy. Psychiatric Annals. 2019;49(12):524-8.
Dr. Safia S. Khan and a research team from the University of Texas (UT) Southwestern Medical Center found that women who have OSA and related comorbid conditions such as preeclampsia, hypertension and gestational diabetes suffer five times greater risk of mortality prior to discharge from the hospital when compared with women who do not have OSA. These risks carry over to increased risk of anesthesia complications associated with OSA. There is evidence of increased risk of postoperative hypoxemia, hypercapnia and sudden death. The increased risk of cesarean section in this population makes this an important consideration.
Screening for SDB is typically not comprehensive or widespread due to a lack of validated screening tools, lack of provider awareness and the need for a deeper understanding of sleep-disordered breathing during pregnancy. Screening for sleep-disordered breathing relies on a diagnosis made with questionnaires like the Berlin Questionnaire and the Epworth Sleepiness Scale. These questionnaires have been validated with elderly populations who are predominantly male, middle aged and non-pregnant. In order to establish accurate diagnosis and therapy of sleep-disordered breathing for pregnant women, screening questionnaires need to be reexamined for efficacy in younger, female and pregnant populations.
Also, patient education designed to improve the patient’s sleep quality awareness should be introduced early in pregnancy so that the patient can be aware of the signs and symptoms of clinically important changes in sleep patterns and complaints of daytime fatigue, morning headaches, and mood changes. These symptoms are very different from the most-often-cited symptoms of OSA in non-pregnant populations, which include snoring, witnessed apneas and nocturnal gasping.
 Screening and education should be introduced early in pregnancy to help improve the patient’s sleep quality.
Screening and education should be introduced early in pregnancy to help improve the patient’s sleep quality.
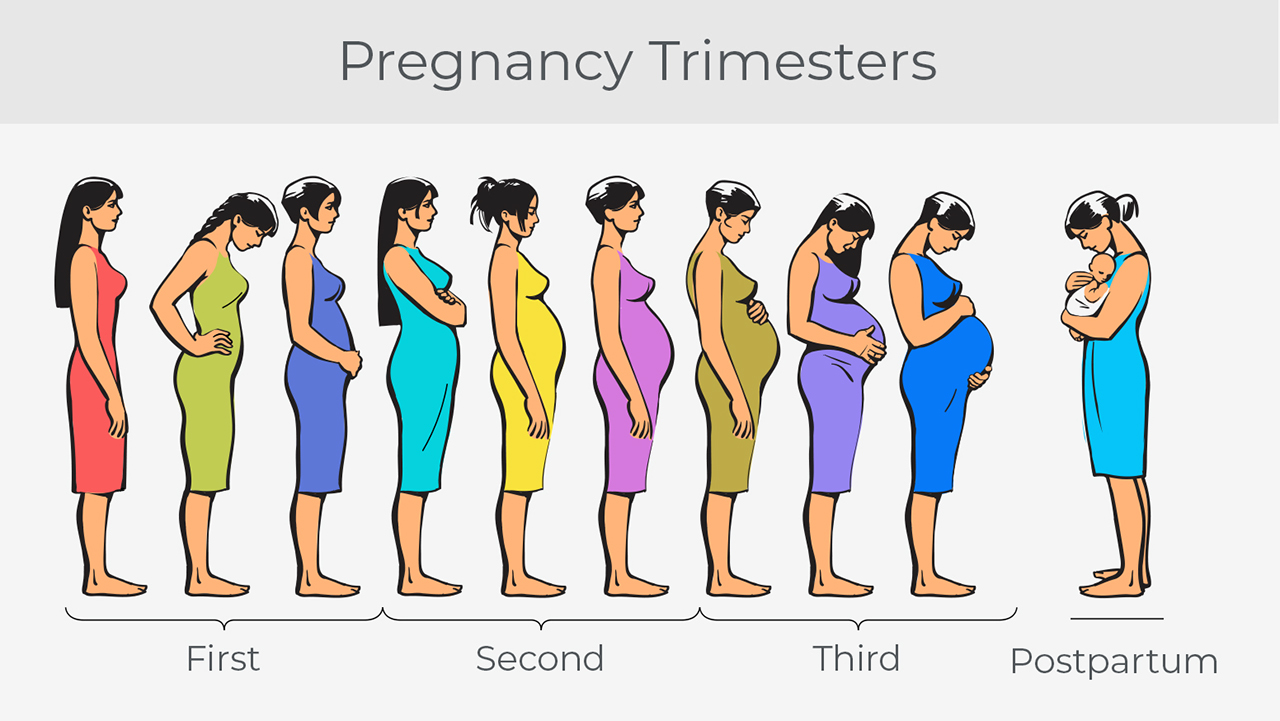
Screening is critical to establish a diagnosis and begin treatment as early as possible. Each trimester lasts 12–14 weeks. As pregnancy progresses, the patient experiences rapid changes in hormone levels. Increased levels of estrogen and progesterone induce capillary engorgement, hypersecretion and mucosal edema of the upper airway. This narrowing of the upper airway begins in the second trimester.
Up to 40% of women report pregnancy rhinitis with nasal congestion and difficulty breathing. This condition, along with fetal movement, heartburn, generalized discomfort and leg cramps, disrupts sleep in pregnancy. Pregnancy-associated weight gain and fluid retention can lead to airway edema and increased airway resistance, which can result in snoring and obstructive sleep apnea. The increase in body mass index (BMI) associated with pregnancy increases the prevalence of snoring and obstructive sleep apnea.
A recent study showed that 15%–20% of obese pregnant women have OSA. As of 2014, half of all pregnant women in the U.S. were overweight or obese. The most modifiable causes of sleep-disordered breathing are weight gain and obesity. It is clear that women, particularly during pregnancy, have a different physiological reaction to narrowing of the airway during sleep than men do and the resulting under-diagnosis of women’s sleep-disordered breathing is a significant health issue.
In the U.S., sleep-disordered breathing is diagnosed by a physician and then treated with continuous positive airway pressure (CPAP) or oral appliance therapy (OAT) based on apnea-hypopnea index (AHI). Most women with SDB suffer from partial prolonged upper airway obstruction, which presents as snoring or mild apnea. These patients often go undiagnosed or, worse, are diagnosed with sleep-disordered breathing but do not qualify for sleep therapy because their condition does not fit the strict qualification guidelines for CPAP/OAT treatment.
It is important that we understand the nuance that exists in the conditions that make up sleep-disordered breathing as related to gender. Qualification for therapy may require a second look at women’s sleep therapy qualification, particularly during pregnancy. The mechanism for providing OSA therapy is very specific and designed to deliver care for a chronic condition with a long time horizon. Most pregnant women who require CPAP or OAT treatment during pregnancy will discontinue treatment once their BMI and hormones return to pre-pregnancy levels.
 Example of treatment with continuous positive airway pressure (CPAP).
Example of treatment with continuous positive airway pressure (CPAP).
The standard of care with CPAP is not designed for short-term use. CPAP therapy is typically initiated with a 12-week trial period (one trimester) to establish that the patient is successfully treated and compliant with CPAP. Once the patient has achieved consistent compliance, long-term therapy with CPAP is approved. For example, the United Healthcare guideline includes the following:
“An initial 12-week period of CPAP is covered in adult patients with OSA if either of the following criterion using the AHI or RDI [respiratory disturbance index] are met:
a. AHI or RDI greater than or equal to 15 events per hour, or
b. AHI or RDI greater than or equal to 5 events and less than or equal to 14 events per hour with documented symptoms of excessive daytime sleepiness, impaired cognition, mood disorders or insomnia, or documented hypertension, ischemic heart disease, or history of stroke.”
Oral appliance therapy can be administered quickly and easily by a trained dentist. This care is recommended by the American Academy of Sleep Medicine (AASM) for patients with a primary complaint of snoring or mild to moderate sleep apnea.
Oral appliances are custom-fit dental mouthpieces that are made by a dentist. The most popular design, a mandibular advancement device (MAD), engages the upper and lower teeth and, using adjustment arms, positions the jaw slightly forward during sleep. This forward position serves to put tension on the muscles and ligaments of the airway to keep them from collapsing and causing the snoring sound. For example, the adjustment arms of the Silent Nite® Sleep Appliance (see below) work like a hinge to improve patient comfort. This MAD allows the patient to talk, drink water and take medication if necessary. When the patient is wearing the oral appliance, it is not readily visible to the bed partner.
 A mandibular advancement device, such as the Silent Nite Sleep Appliance, treats snoring and sleep apnea quickly and effectively.
A mandibular advancement device, such as the Silent Nite Sleep Appliance, treats snoring and sleep apnea quickly and effectively.
During pregnancy, snoring and OSA are health risks for the mother-to-be and baby. Awareness of the issue is on the rise; however, screening is still not advanced enough to deliver unambiguous screening results in pregnant patient populations. Therapy options include CPAP and an oral appliance. Although a definitive diagnosis of OSA requires a sleep test in the home or hospital sleep lab, dentists may provide provisional mandibular advancement device (PMAD) therapy to address the immediate need for short-term care.
Increased body mass and hormone changes in pregnancy resolve postpartum. Therefore, long-term care with CPAP or an oral appliance may not be necessary. Care should be taken to identify these patients early through prenatal sleep education and screening. Simple treatment with an oral appliance for the duration of the pregnancy is an inexpensive, reversible option to support the airway during this crucial time.
To discover the simple, three-step process to screen and treat patients for snoring and sleep apnea, visit glidewell.com/pmad.
Dental CE
Snoring and Sleep Apnea Article
Send blog-related questions and suggestions to hello@glidewell.com.


