Case Study: Immediate Placement of a Narrow-Diameter Implant Into an Extraction Site Following Failed Endodontic Treatment
Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Dental practitioners will inevitably encounter patients who have received previous endodontic treatment that is failing. Success rates for endodontic treatment have been reported at 77.8 percent after two years, 71.8 percent after four years, and 62.9 percent after six years.1 In cases of failed root canal treatment accompanied by a periapical lesion, reported success rates for further endodontic therapy have ranged from 27.8 to 80 percent.2,3 In many of these cases, depending on the lesion size and the reason for failure, the best treatment option is to extract the tooth and replace it with an implant.
In this case study, there was clinical presentation of a short root, a large endodontic post, Class I mobility and a large periapical lesion. Conventional retreatment was not feasible due to the post, and implant therapy is a more successful mode of treatment than periapical surgery in cases of persistent periapical lesions or failed root canal treatment.4,5 In light of this, the next decision to make was whether immediate or delayed implant placement was indicated after extracting the tooth and grafting the site.6
Implant therapy is a more successful mode of treatment than periapical surgery in cases of persistent periapical lesions or failed root canal treatment.
EXAMINATION AND CASE DISCUSSION
The patient presented with chief complaints of discomfort and a “pimple” that had formed above the maxillary left lateral incisor (Figs. 1a, 1b). Upon intraoral examination, the patient exhibited a small fistula apically in the area of tooth #10. Radiographic evaluation revealed that the tooth had received endodontic treatment, including a post and core procedure and a PFM restoration. A large periapical lesion approximately 7 mm in diameter was noted (Fig. 2).
The following treatment options were discussed with the patient:
1. Endodontic retreatment of the tooth and fabrication of a new crown.
2. Extraction of the tooth and restoration of the edentulous space with a removable partial appliance.
3. Extraction of the tooth and restoration with a fixed bridge.
4. Extraction of the tooth followed by immediate or delayed placement of an implant.
The patient selected option No. 4 and was advised that, following tooth extraction, the decision of whether to proceed with immediate or delayed implant placement would depend on the size of the resultant lesion and the ability to gain sufficient primary stability.
SURGICAL PHASE
The patient was started on amoxicillin three days prior to surgery and would continue for seven days after. Profound anesthesia was attained utilizing a labial and palatal infiltrate of 4 percent Septocaine® (Septodont; Lancaster, Pa.). Because it was unknown whether an implant could be placed at the time of surgery, a conservative flapless approach was utilized. To preserve soft tissue and facilitate an atraumatic extraction, a Spade Proximator™ (Karl Schumacher; Linden, N.J.) was used to loosen and separate the root from the PDL fibers (Fig. 3). A pair of sharp-beaked forceps was used to remove the tooth while preserving the hard- and soft-tissue architecture (Fig. 4).
A serrated curette was used to degranulate the socket and bony lesion. While excavating cystic tissue from the lesion, a large labial defect was identified. In light of this finding, the decision was made to carry out a full-thickness periodontal flap. To minimize any potential cosmetic issues, a sulcular incision with a release along the distal line angle of tooth #11 was performed. After flap reflection, the size of the lesion was evaluated.
Complete degranulation was performed first with a curette and finished with a No. 8 round bur on a slow-speed handpiece. It is crucial to success to make sure that all potentially bacteria-infected bone is removed. If bacteria from the periapical lesion has the opportunity to colonize the new implant site, the outcome can be compromised, with enterococcus faecalis as a common culprit in these types of cases.7
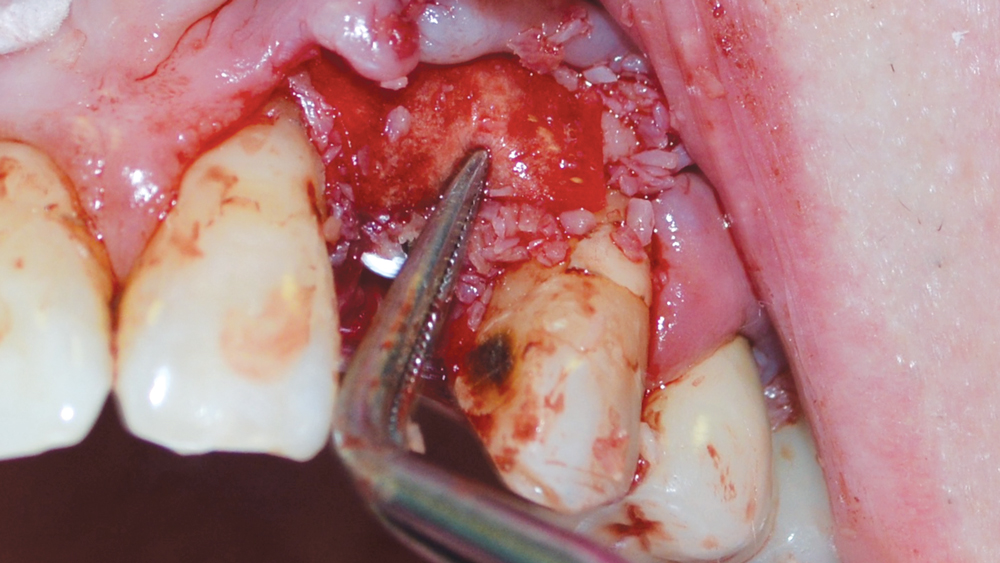
Once healthy, bleeding bone was exposed, the lesion left only a 5 mm bridge of bone labially at the crest (Fig. 5). However, sufficient bone was evident to facilitate immediate implant placement with the proper selection and use of allograft material, a collagen membrane and a 3.0-mm–diameter implant.
A high-speed handpiece with a long surgical carbide fissure bur was used to enter the palatal aspect of the lamina dura at about 3/4 of the depth of the socket. Once a purchase point was established, a 1.5 mm twist drill was used to create an osteotomy at the proper trajectory (Fig. 6). The pilot hole was opened up with a 2.4/1.5 mm twist drill, and a 2.8/2.4 mm x 13 mm twist drill established the final trajectory and osteotomy depth. This facilitated positioning for the implant beyond the apex of the socket, with the platform slightly subcrestal (Fig. 7). The full-thickness flap allowed visualization of the final osteotomy within the labial defect (Fig. 8).
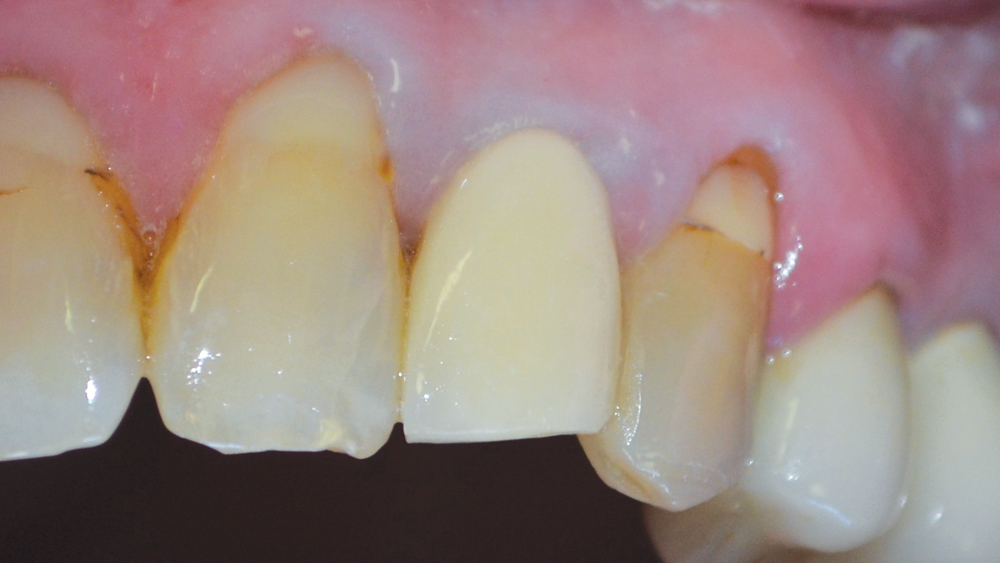

Figures 1a, 1b: Facial and occlusal views of the preoperative condition of the patient, who had received prior endodontic treatment for tooth #10 that was failing.
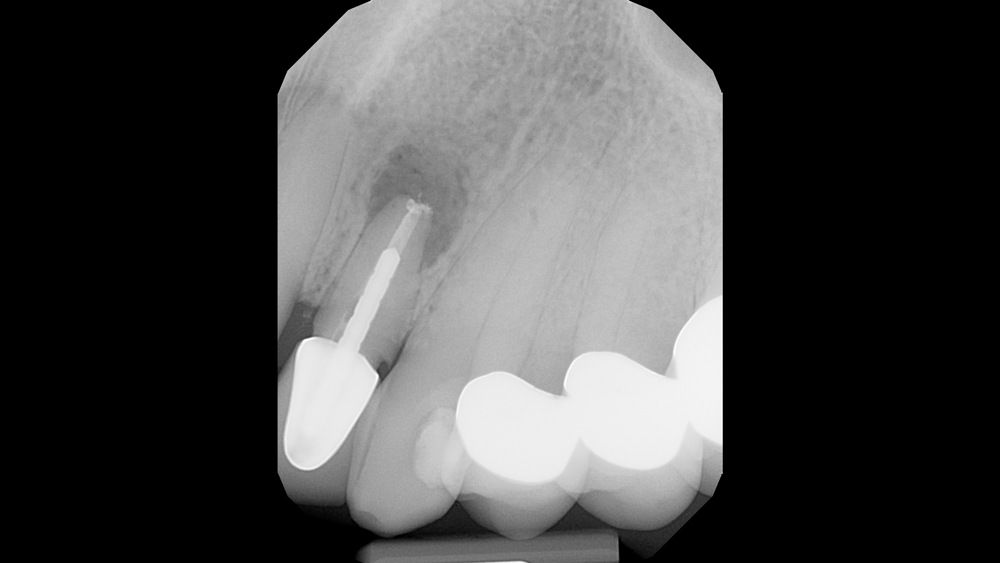
Figure 2: Radiographic examination exhibited a large periapical lesion above tooth #10.

Figure 3: A Spade Proximator was used to create space between the tooth root and the socket.

Figure 4: The tooth was extracted atraumatically with sharp-beaked forceps.
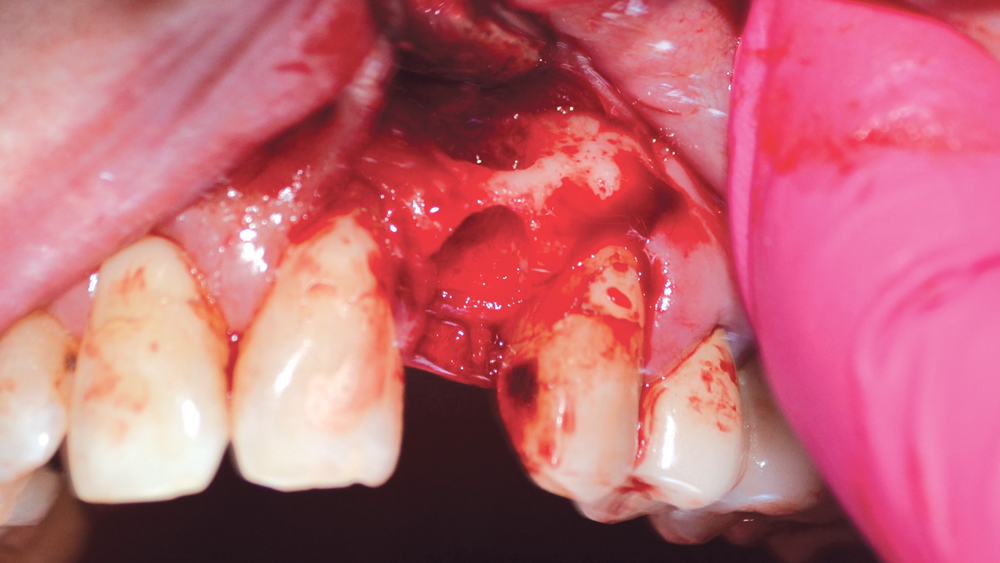
Figure 5: Periapical lesion following debridement. The site was deemed suitable for immediate implantation with the aid of cortico/cancellous allograft and a resorbable collagen membrane.
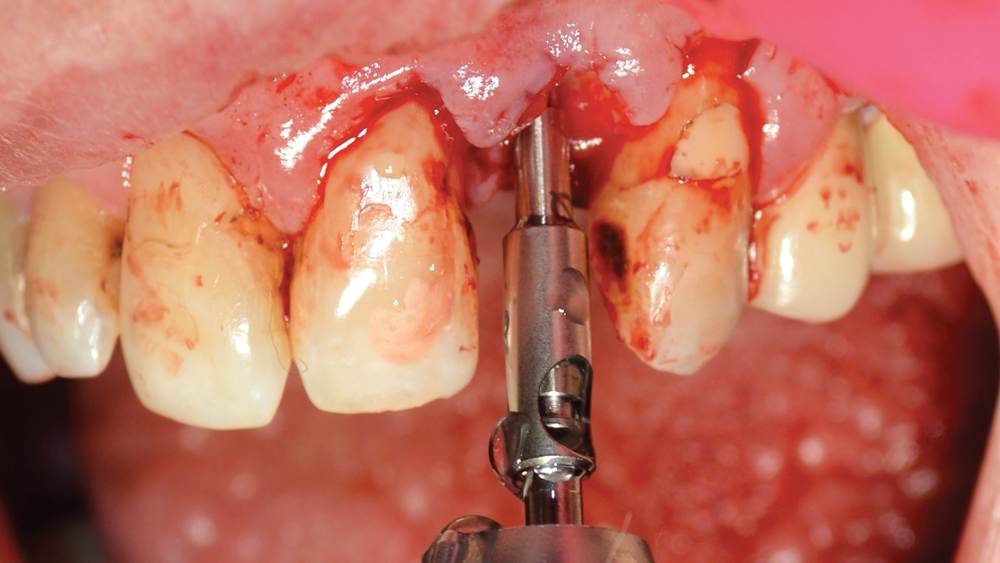
Figure 6: A 1.5 mm twist drill was used to create the pilot hole for the implant osteotomy.
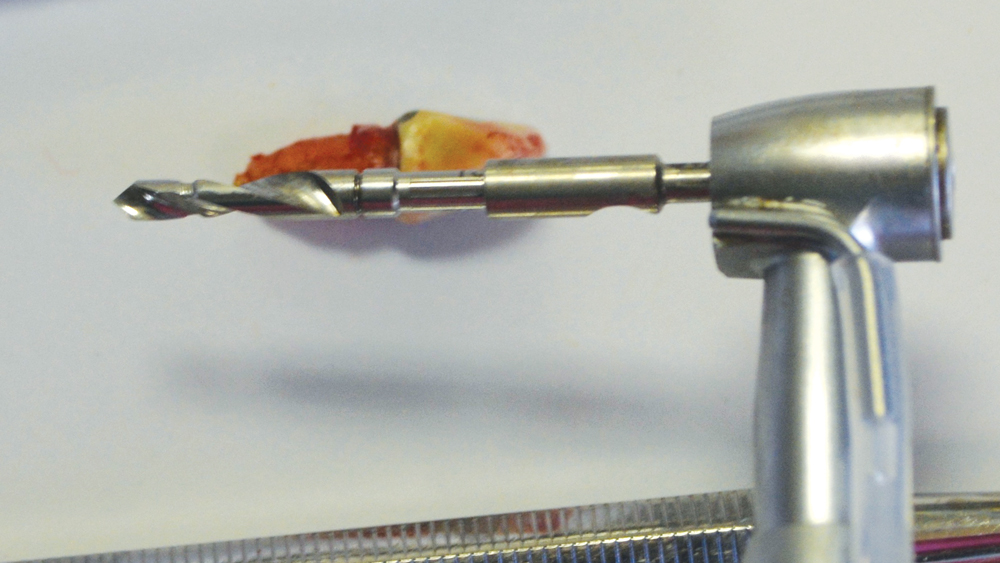
Figure 7: The 2.8/2.4 mm x 13 mm twist drill illustrates the depth of the final osteotomy in comparison with the extracted tooth.
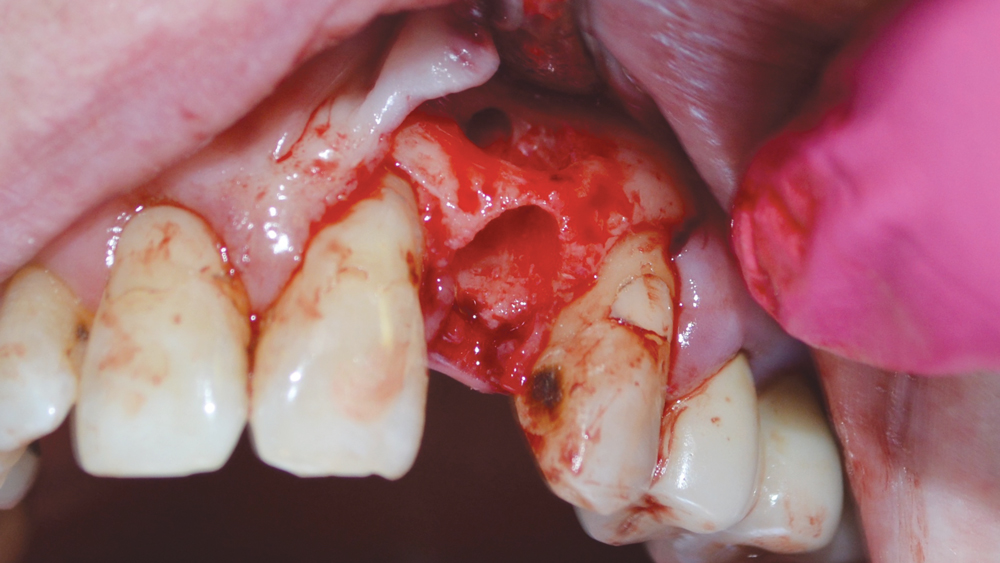
Figure 8: The final depth of the osteotomy extended through the labial defect.

Figure 9: A 3.0 mm Hahn Tapered Implant was selected for its deep, sharp threads and ability to fit within tight anatomical spaces.
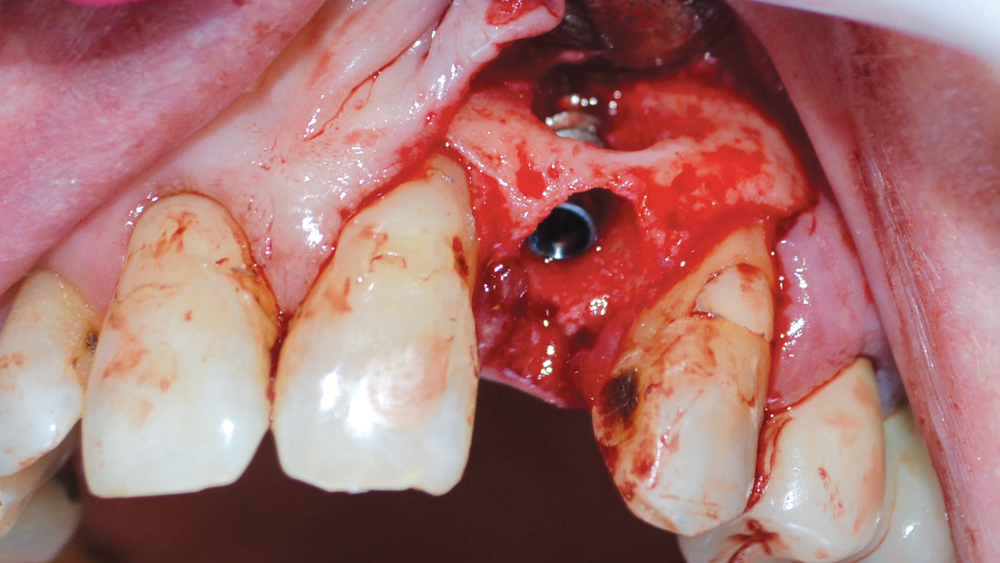
Figure 10: Implant inserted to final position, approximately 5 mm beyond the defect and 1 mm subcrestal.
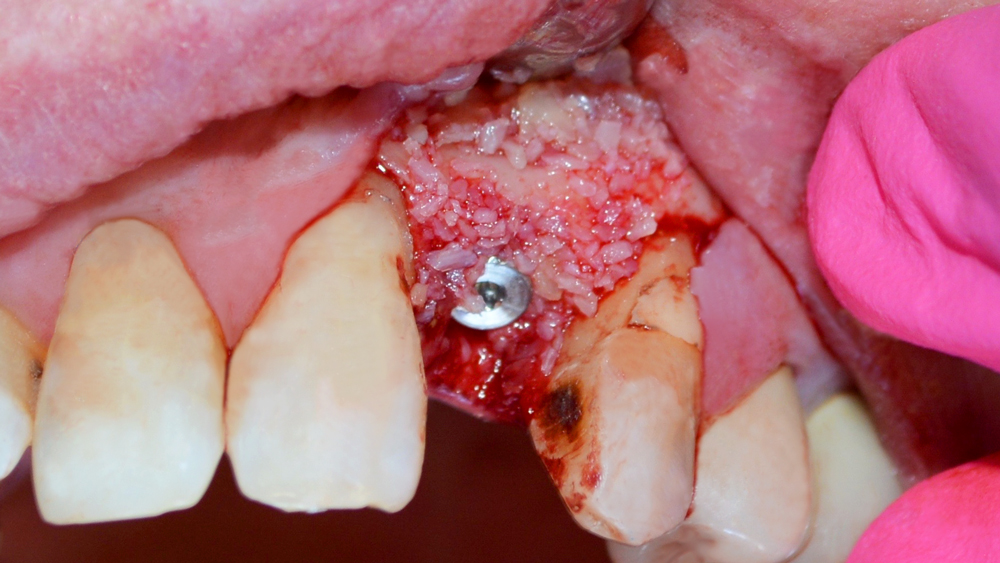
Figure 11: The labial defect and gaps around the implant and within the extraction socket were filled with Newport Biologics Mineralized Cortico/Cancellous Allograft Blend.
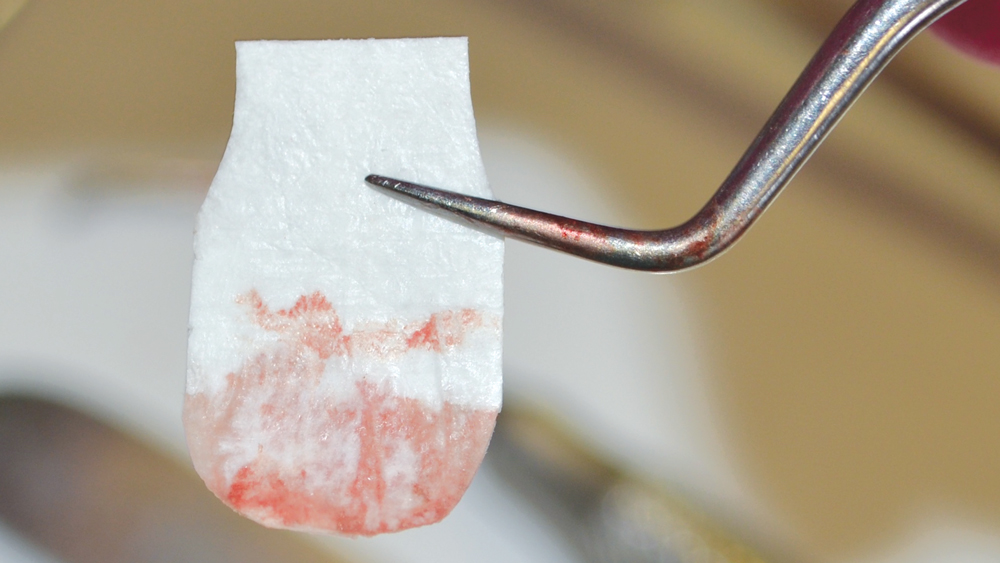
Figures 12a, 12b: A Newport Biologics 4-6 month collagen membrane was used to cover the grafting material and guide bone regeneration during the healing phase.
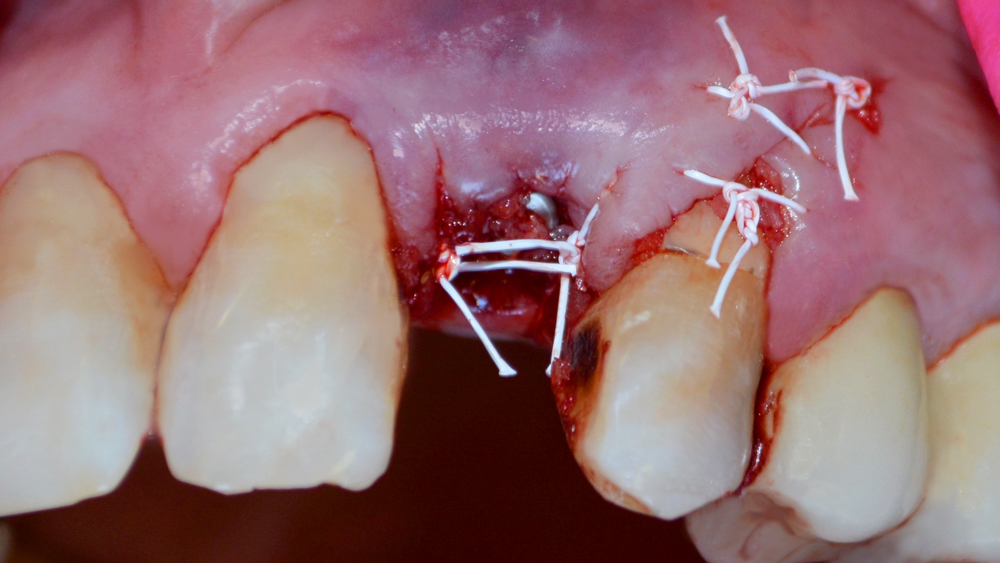
Figure 13: A PTFE suture was used for final closure of the surgical site.
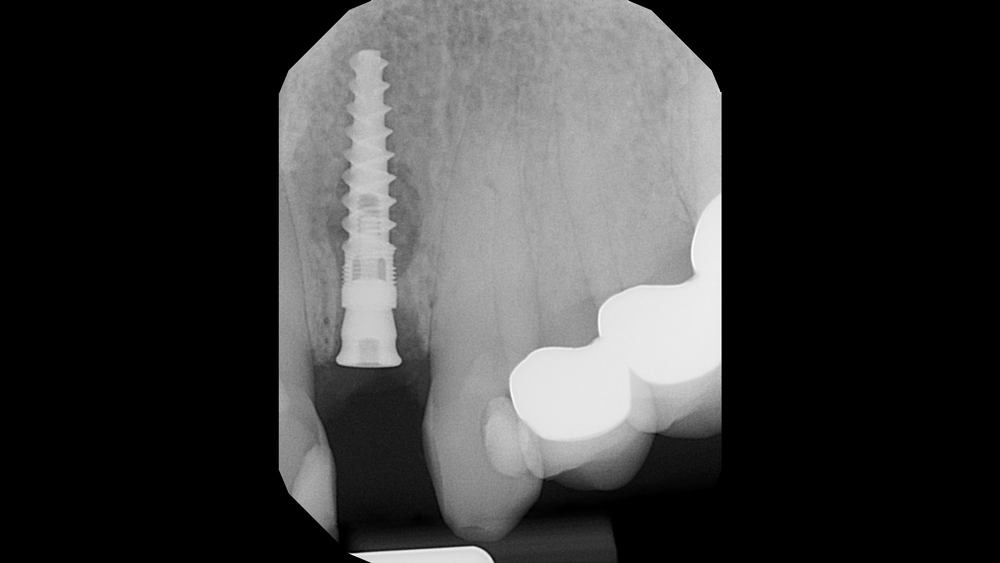
Figure 14: Radiograph shows 3-mm-tall healing abutment in place and final positioning of Hahn Tapered Implant.
A 3.0 mm x 13 mm Hahn™ Tapered Implant (Glidewell Direct; Irvine, Calif.) was delivered into the osteotomy site using a handpiece at 20 rpm, attaining a final placement torque value of 30 Ncm (Fig. 9). One of the advantages of the Hahn Tapered Implant System is the availability of this narrow-diameter size for situations in which there is limited bone available for implant placement. Approximately 5 mm of the implant engaged bone beyond the defect and made contact with the palatal wall of the socket. Excellent primary stability was achieved due to the thread profile of the implant and its ability to “grab” into the surrounding bone.
Excellent primary stability was achieved due to the thread profile of the implant and its ability to ‘grab’ into the surrounding bone.
The platform of the implant was situated 1 mm below the facial crest to accommodate any potential loss of bone during healing (Fig. 10). The implant’s machined collar is conducive to the growth of bone around the prosthetic platform. A 3.0-mm–tall contoured healing abutment was placed and tightened by hand. The implant was not provisionalized with a temporary restoration in order to limit the application of functional forces on the implant site, where only minimal bone volume was present at the time of placement.
The labial defect and the facial, mesial and distal gaps surrounding the implant were grafted with Newport Biologics™ Mineralized Cortico/Cancellous Allograft Blend (Glidewell Direct), which is ideal for regenerating bone within periodontal defects and extraction sockets (Fig. 11). A Newport Biologics Resorbable Collagen Membrane 4-6 was draped over the defect and tucked subperiosteally (Figs. 12a, 12b). This provides a stable barrier that holds the allograft material in place, forming a scaffold for cell ingrowth. The soft-tissue complex was then repositioned and closed with PTFE suture (Fig. 13). A final radiograph was taken, and an interim removable prosthesis was delivered, taking care not to impinge on the soft tissue or the healing abutment (Fig. 14).
At the 10-day follow-up exam, the patient reported minimal discomfort after the surgery and was very happy with the procedure. We will follow up in one month and plan to restore in four months with an Inclusive® Custom Implant Abutment and an Obsidian® Fused to Metal crown (Glidewell Laboratories; Newport Beach, Calif.).
CONCLUSION
When working with a patient in deciding the best long-term solution for a failing tooth, many factors must be taken into account and sometimes the final treatment direction cannot be determined until the time of surgery. Immediate placement of dental implants in extraction sites is a proven method with a high success rate.8 Even when a large defect is present, in many cases properly selected allograft material and modern implant design allow for predictable bone regeneration while the immediately placed implant integrates and the extraction site heals. When carried out correctly, this type of treatment can shave months off a treatment plan and provide high satisfaction for both the practitioner and patient.
References
- ^ Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009 Jul;35(7):930-7.
- ^ Rahbaran S, Gilthorpe MS, Harrison SD, Gulabivala K. Comparison of clinical outcome of periapical surgery in endodontic and oral surgery units of a teaching dental hospital: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Jun;91(6):700-9.
- ^ Testori T, Capelli M, Milani S, Weinstein RL. Success and failure in periradicular surgery: a longitudinal retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Apr;87(4):493-8.
- ^ Frank AL, Glick DH, Patterson SS, Weine FS. Long-term evaluation of surgically placed amalgam fillings. J Endod. 1992 Aug;18(8):391-8.
- ^ Torabinejad M, Landaez M, Milan M, Sun CX, Henkin J, Al-Ardah A, Kattadiyil M, Bahjri K, Dehom S, Cortez E, White SN. Tooth retention through endodontic microsurgery or tooth replacement using single implants: a systematic review of treatment outcomes. J Endod. 2015 Jan;41(1):1-10.
- ^ Schlesinger C. Immediately Loading Dental Implants: Doing It Right for Long-Term Success. Dentistry Today. 2016 May;35(5):84, 86-9.
- ^ Flanagan D. Implant Placement in Failed Endodontic Sites: A Review. J Oral Implantol. 2016 April;42(2):224-30.
- ^ Lang NP, Pun L, Lau KY, Li KY, Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Implants Res. 2012 Feb;23 Suppl 5:39-66.



