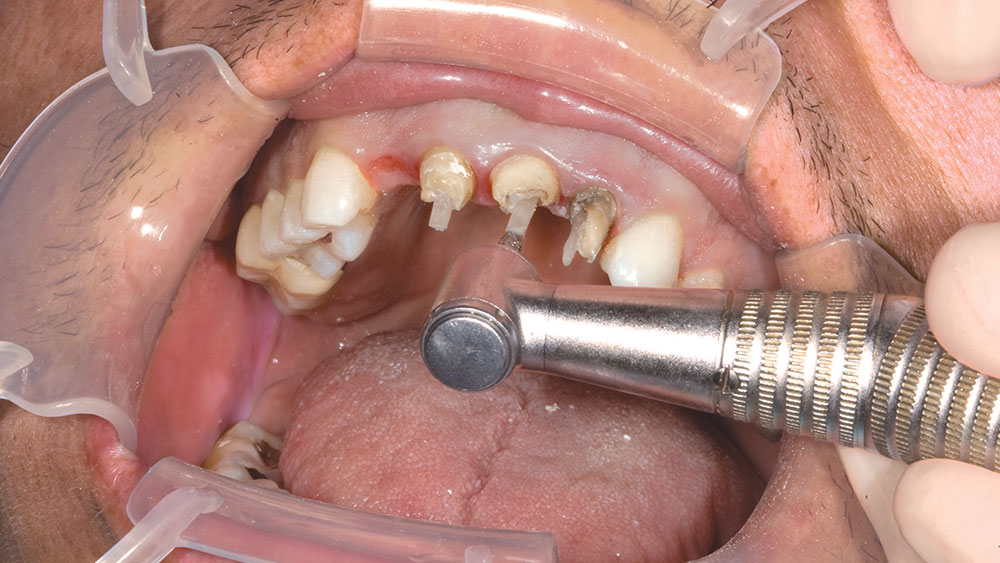
A Unique, Simplified Approach to Post/Buildup Placement with Lab-Fabricated BioTemps®
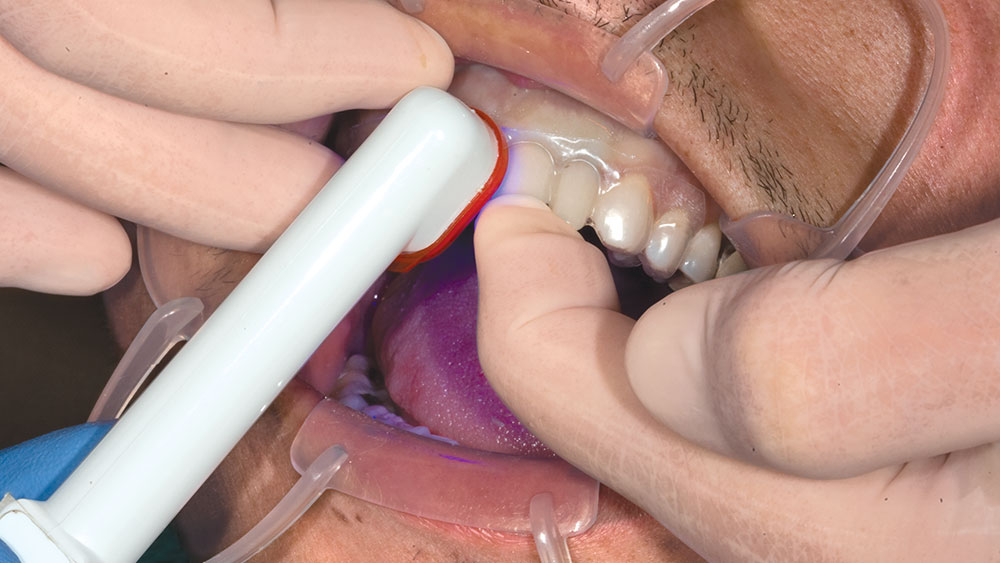
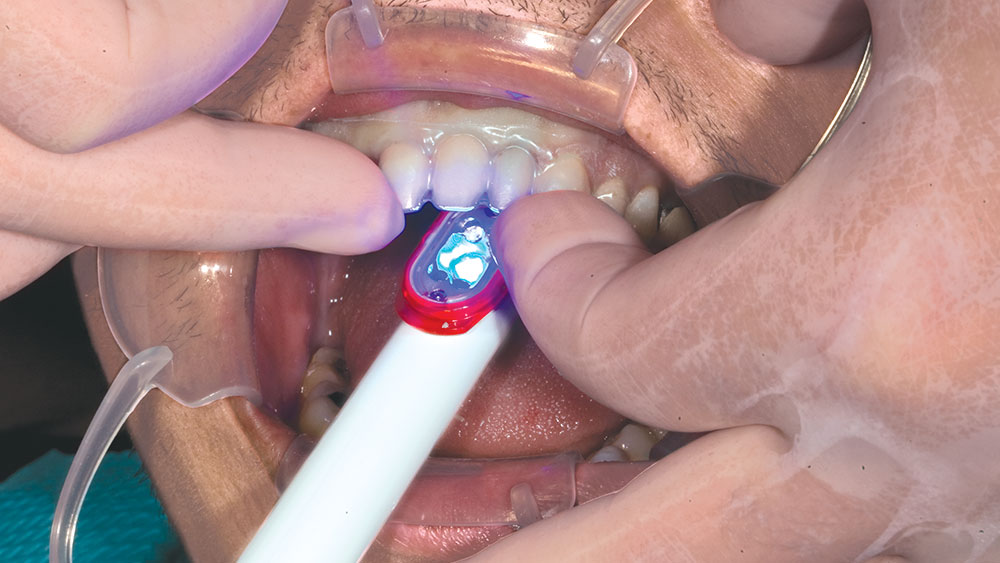
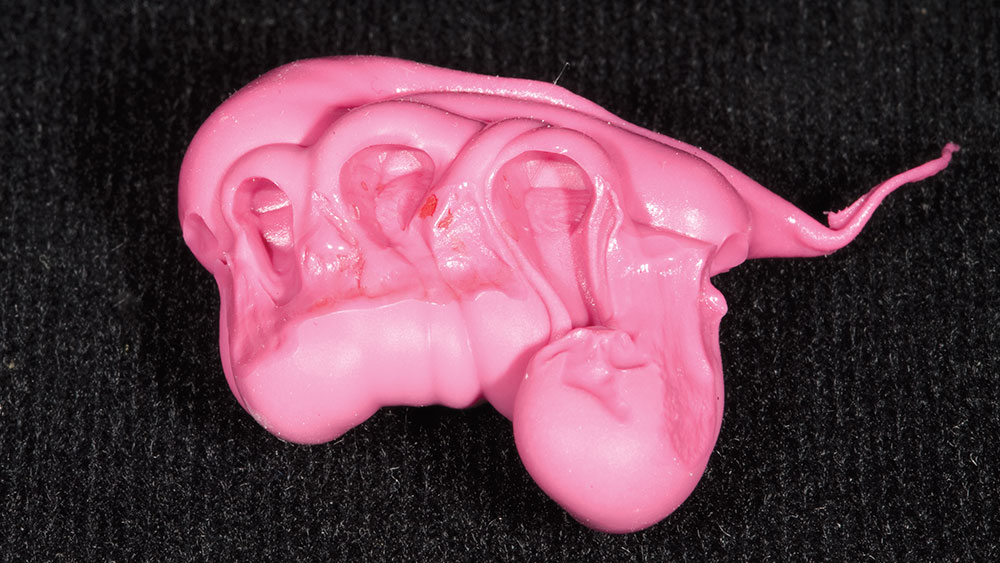
The following presents a fairly straightforward anterior crown & bridge case. However, I wanted to share this case with you because of a technique I use during post and core fabrication, which simplifies the procedure — and that valuable technique is called BioTemps®. I use BioTemps for these types of anterior crown & bridge cases because I can use the lab’s prepped model to shape the tooth preparations. Doing so ensures the BioTemps fall into place with minimum effort. If you have ever seen a BioTemps prepped model, you know that the preps are nearly flawless with approximately 1 mm of stone removed for the preparation. By the time I have replicated these preps with the buildup material and finished shaping them, I have removed the proper amount of material for the final restorations.
Contact Dr. DiTolla at mditolla@glidewelldental.com or call 888-303-4221.
RelyX Fiber Posts and RelyX Unicem are a trademark of 3M ESPE.
OptiBond Solo is a registered trademark of Kerr Corporation.
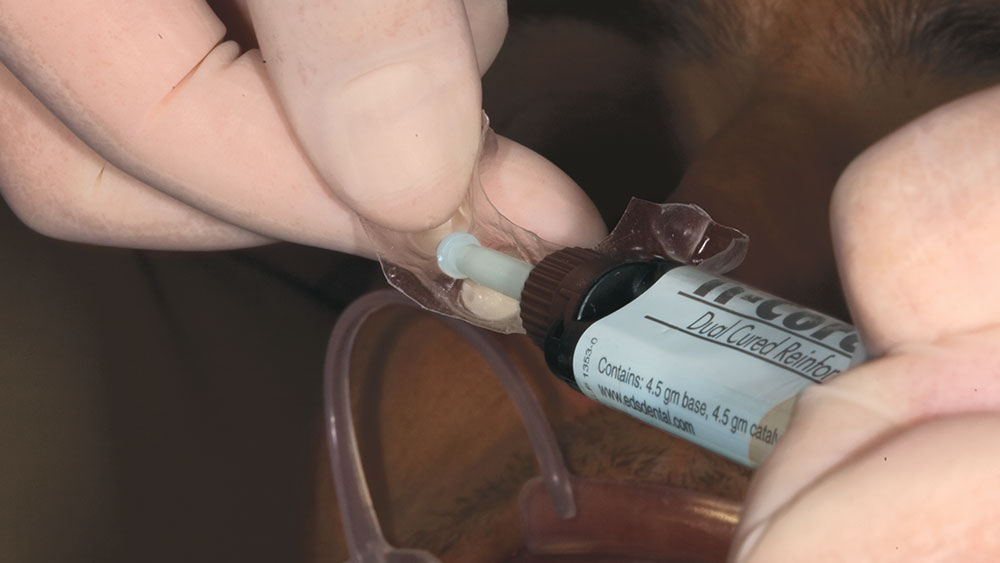
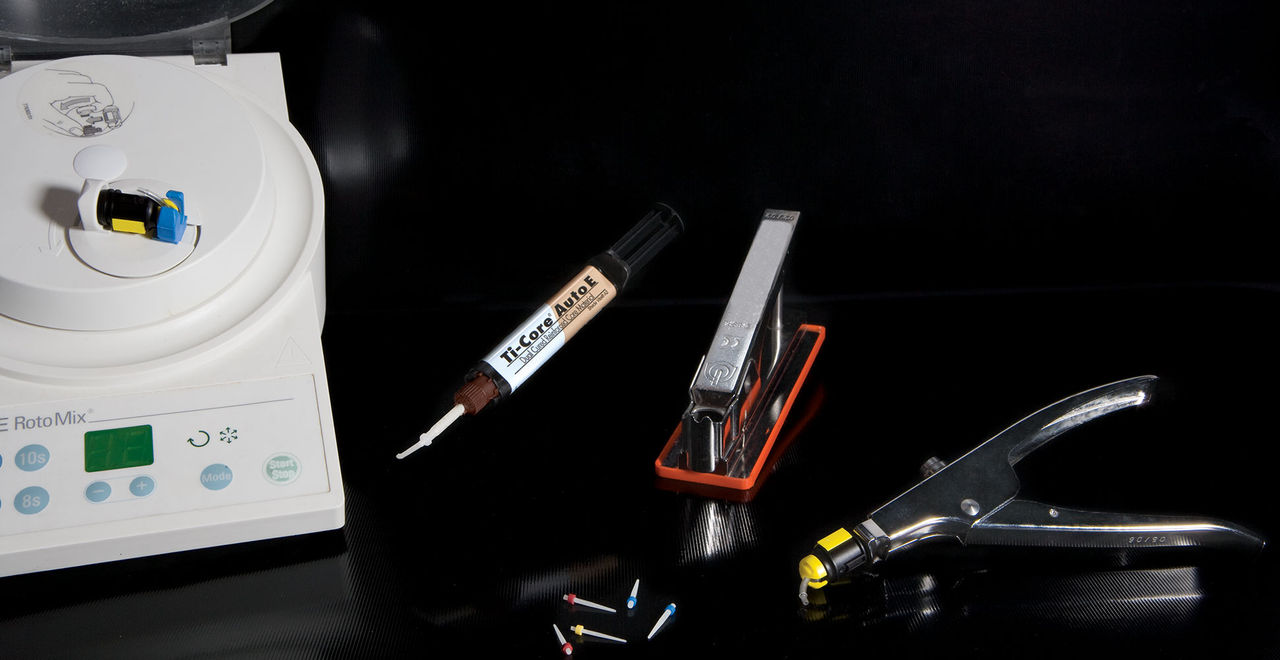
Ti-Core Natural is a registered trademark of Essential Dental Systems, Inc.
Ultrapak #00 cord and #2E cord are a registered trademark of Ultradent Products, Inc.
Tooth & Gums Tonic is a registered trademark of Dental Herb Company.
Captek is a trademark of Precious Chemicals, Inc.