One-on-One with Dr. Michael DiTolla: 20 Questions with Dr. Brock Rondeau

There are a few important people I have met in dentistry who have done more than change the way I practice — they have changed the way I look at how a patient’s multiple dental problems may share a common origin. The first time I took Brock’s course I had a hard time believing what he taught me; it was so far from what I learned in dental school. I took the course a second time when I was ready to begin some ortho cases and never looked back after that. Almost 20 years later, I see everything Brock taught me is accurate and effective, and that mothers love two-phase treatment as much as he said they would. Enjoy this interview, and I hope you will consider taking Brock’s course. Even if you don’t want to treat these cases, you owe it to your patients to learn how to diagnose them.
Question 1: I’d like to start by just letting people hear a little bit about your background. I took your comprehensive ortho course 15 years ago and started doing ortho, and you’re still the only general practitioner I know who treats solely orthodontic cases and TMD cases — and now snoring and sleep apnea as well. It’s really interesting to speak with someone who is a GP but has decided to do only ortho. Why don’t you tell us a little about your background and how you got started and how it ended up that you decided to treat only ortho patients.
Dr. Brock Rondeau: A long time ago, I read Napoleon Hill’s book — he’s a billionaire — titled “Think and Grow Rich” (Highroads Media). And in the book, I remember what he said. He said: “Find out what people want and give it to them. If you want to be rich and successful, find out what people want and give it to them.” And I think what happened was, I looked at the profession and saw that there was a lot of mothers coming in with their kids and asking me what we can do with these crooked teeth, these crooked jaws, the problems these kids were having. And then I would refer them out to the orthodontists in my area.
You know, 30 years ago they were not treating kids early. And the orthodontist was telling the mother, “Let’s wait until all their permanent teeth have grown in.” The mothers would say: “Well, that doesn’t sound sensible. You just told me we’ve got to treat cavities when they’re small, and pockets in the gums when they’re small. And now you’re telling me you’re going to wait until my child is 13 to begin treating these problems? He’s got crooked teeth and a problem with self-esteem because he hates how his smile looks.”
Then I took a course in orthodontics. It seemed like a niche I could get into and something I’d be interested in doing as well. And the other thing that really interested me in those days was the fact the staff did all the work! I was really encouraged by that. So, I thought, I can do my general dentistry in one room, I can have a hygienist doing perio in another room, and I can have another hygienist in the other room doing orthodontics — and all I have to do is go in and tell her what to do. So that’s the way the course was sold to me — that the staff does most of the work and you can just be kind of a supervisor. In most orthodontic offices, the staff really does do a large part of the work. The orthodontist or the general dentist does the thinking and the diagnosis, and the staff actually does most of the work. So that appealed to me. Then I got into it and I really did like it. I really liked helping the kids, particularly with the functional issues. These little kids come in with narrow jaws, and I knew that if I didn’t extract or develop the arches that the cuspids were going to come in like fangs. And then if I sent that case to some orthodontist, they would recommend bicuspid extractions. But from the courses I took from Dr. [James A.] McNamara and Dr. [Donald] Woodside, I realized if you expand or develop those arches you can prevent extractions of teeth. So, the mothers were very receptive to that. And then, of course, I took Dr. John Witzig’s courses many years ago, and he showed the use of functional appliances to bring the jaws forward. I thought that was great because the profiles were fantastic — the patients looked great. These little kids would come in with their nose coming through the door five minutes before their chin, and then you put these functional appliances in and the jaw comes forward and the kids look great.
I didn’t realize in those days that functional appliances would have such a significant influence on the temporomandibular joint. We really didn’t even discuss TMJ very much back then. But then, it was kind of funny. I remember a mother once said to me: “You know, my little girl had headaches before you put that appliance in, and that appliance stopped the headaches. Could you put one in for me?” And I said, “These appliances really aren’t for adults, these are for children — growing children.” All the literature said they were for growing children. But again, I had taken courses from Dr. Brendan Stack, who’s probably one of the world’s best on TMJ, and he had shown some cases using adults. So I said, “Well, you know what, Brendan did it so maybe I’ll do it.” I remember telling the mother, “I’m not even going to charge you,” which you never should do, and I said, “I’m going to put this appliance in and see what happens.” And lo and behold it worked! It brought the jaw forward, the condyle came down and forward, it decompressed the joint, and she got rid of her pain. Then I said, “Gee, this really is something,” because what I was taught to do in dental school was push the jaw up and back, and that didn’t work. I was also taught in dental school to use flat plane splints. Well, flat plane splints make the jaw go distally and that’s not good if the jaw is already back too far. So functional appliances seemed to be the answer. I first started doing children with functional appliances, and then gradually built a practice where I now do adult TMD/ortho cases. It’s been quite an evolution.
Anybody getting into this, Mike, I would advise them to gradually add this to their general practice. Don’t try to switch over immediately. Learn your skills. See if you like it. Most of these patients are in your practice already; most of those kids are in your practice because 70% of all children have some form of malocclusion. And — you and I have talked about this previously — mothers really want their kids to be treated and will pay to have their kids treated.
The proper size to the maxillary arch is the key to patients being able to breathe through their nose. Because when you expand the maxilla, you enlarge the nasal cavity transversely. When you expand the maxilla, the palate drops. That makes the nasal cavity larger vertically. When you just expand the maxilla, you are providing the best service possible for any patient. If I could do one thing for every patient, that’s what I would do.
Q2: So, Mom takes her kid to the orthodontist and the orthodontist says, “Well, let’s not do anything until she’s 13 or 14.” And you mentioned Mom would be upset. I think most dentists would say, “Well, I don’t understand why.” But the reason is, for most of these cases, Mom doesn’t want her kid to look “ugly.” And she’s got malocclusions, the teeth are crooked, and this poor kid has to go to school and be made fun of. And it’s really not that Mom is so worried about the ortho aspect of this, per se — she’s more worried about how her child looks, right?
BR: Of course. Self-esteem is a big thing. I was lucky I never had buck teeth. But I see these kids come in with buck teeth and they really are very shy. They’re shy and they don’t have a normal personality and they’re just not like typical children. And the minute you fix that malocclusion and you put a functional appliance in and get that jaw forward, they look like all the other kids and their whole personality changes. It’s just remarkable. Plus, if they did have headaches or earaches or any other TM dysfunction, it brings the jaw forward and you relieve all that. And, you open up the airway. So the kid is breathing better and sleeping better.
It’s interesting — a lot of kids have sleep apnea because of large tonsils and adenoids. You and I talked about that when you took my course 15 years ago. And getting those tonsils and adenoids out has a significant improvement on the child’s ability to learn because the pituitary gland secretes a growth hormone. And if children don’t get to the deep stage of sleep, which they don’t when they have sleep apnea or when they’re snoring, they don’t grow properly. So these kids’ growth is stunted, they wet the bed, and many of them develop ADHD — attention deficit hyperactivity disorder. And again, the medical profession will prescribe medication for that — Ritalin — to try and calm them down. But that’s just treating the symptom while the cause of the problem is a blocked airway, which is due to the tonsils and adenoids. Get those out and these kids do beautifully.
Q3: I remember when I took your course 15 years ago that you used to get into arguments with the medical community because you could not find an ENT to take out the tonsils and adenoids for those reasons. They thought you were crazy. Rather, they wanted to wait for six bouts of tonsillitis before they resorted to taking them out. In the last 15 years, has that changed much? Are ENTs now more willing to listen to a dentist?
BR: Well, it’s three times now, three infections a year requiring antibiotics before they will typically remove tonsils and adenoids. My way around it is I have an overnight sleep study I give to kids. If I can show that these children have sleep apnea, they have to take them out. And I have no problem at all when they have sleep apnea. In fact, an ENT wrote me a letter the other day and said, “This patient’s tonsils aren’t large.” I took a picture of the tonsil and put it on an 8×10 photo and sent it to him — it looked like an apple, it was so big. The guy said in the response, “Wow, I guess they are pretty big.” So, I still send a copy of the ceph that shows the airway constriction, but most of the ENTs don’t learn how to read a ceph. General dentists look at cephs, orthodontists look at cephs, but ENTs don’t. But I think it’s getting better. I do have some ENTs who will definitely take them out for me, and I have articles to give dentists who take my courses to help educate ENTs. I find that everything is education — there is not enough communication between the medical profession and the dental profession.
Q4: Well, if the ENT said the tonsils weren’t big enough to come out at this time and then you took a photograph and sent it back to him and he said, “Wow, those are big,” what was he basing his assessment that they weren’t very big on if he didn’t look at them visually?
BR: You have to keep in mind that the tonsils go up and down. Say, the child is allergic to dairy products. If they have a lot of dairy products, they’ll get really big. And then when they go off dairy products for three or four days, maybe they’ll shrink. They also get larger with colds, but we won’t take them out if they get large with a cold because it’s part of the immune system. But if they’re consistently blocking the airway and causing snoring and sleep apnea and all kinds of other health problems, then we definitely get those out. It also encourages mouth breathing.
Q5: So the bottom line is that a patient can have enlarged tonsils and make an appointment to go see an ENT, and maybe the first appointment is 10 days later, and when the patient shows up they’re back to their normal size and the ENT will say, “I don’t know what you’re talking about.”
BR: That can happen, that can definitely happen sometimes. So we bring them in several times — maybe once every two weeks — and we watch them. And we also see if they’re mouth breathing. If they’re mouth breathing because of large tonsils blocking the airway, that is a problem because malocclusions have been linked to mouth breathing. Because when the tongue sits low in the mouth, it doesn’t go up to the roof of the mouth when you swallow. Every time you swallow the pressure from the tongue doesn’t spread out the maxilla, so the upper maxilla constricts. When the maxilla is constricted you get crossbites, and you also get the mandible going distally. The cause of the Class II malocclusion has long been studied from every angle. It was established in the 1900s that the cause of the Class II malocclusion was mouth breathing, which caused constriction of the upper arch and forced the mandible to go posteriorly to help the patient occlude better. We really have to get to the cause of these problems, and we have to fix these airway problems early.
Q6: One of the eye-opening things I learned in your class 15 years ago is that, when a child swallows 2,000 times a day — when that tongue presses up against that anterior portion of the palate — it helps to expand the upper jaw. And until I learned that from you and I started reading some of Dr. Brendan Stack’s work on how the skull itself was constantly expanding and contracting, I had always thought of the mouth and the skull as being in a fixed, concrete state. I never realized just how fluid and how dynamic things were. But it’s amazing how just through swallowing and the tongue pressing on the anterior palate, it really shapes the maxilla to the ideal shape and size, doesn’t it?
BR: Absolutely, it’s key. The proper size to the maxillary arch is the key to patients being able to breathe through their nose. Because when you expand the maxilla, you enlarge the nasal cavity transversely. When you expand the maxilla, the palate drops. That makes the nasal cavity larger vertically. When you just expand the maxilla, you are providing the best service possible for any patient. If I could do one thing for every patient, that’s what I would do. And that’s usually my first step. Expanding the maxilla creates enough room for all the permanent teeth to fit. It makes more room for the tongue so the patient can speak properly. Having a proper size maxilla allows the mandible, sometimes on its own, to come forward and help correct the Class II malocclusion. It will certainly correct the Class II Division II malocclusion if you expand the maxilla and torque those anteriors out. And many times, the mandible comes forward on its own. A lot of these kids, the malocclusions can really be corrected long before their permanent teeth have even erupted. It’s so easy to work with kids with fixed removable functional appliances when they’re actively growing. The mothers will happily bring them in, the mothers will pay your fee, and everybody appreciates what you do. You see the kids get healthier and better looking, and it’s very rewarding for doctor and staff. In fact, I’ll tell you one thing: you’ll never get any of my hygienists to go back to perio. They are orthodontic hygienists who I have trained, and they would never go back to perio — they love what they do.
Q7: When I took your course, I mistakenly thought treating adults would be easier than treating kids. Boy, was I wrong! And it wasn’t until I started doing some cases that I realized it was much easier to hop in and do this type of dentistry on kids.
Today I saw a patient, an adult female, and I thought of you because she had her four bicuspids extracted. As I looked at this patient from the side, her face looked very flat. It looked like somebody had hit her in the mouth with a baseball bat — just a very flat face from the base of the nose down to the chin. And as I examined her intraorally, I noticed a diastema between the cuspids and second bicuspids. Is this something that you see routinely, this kind of relapse after four bicuspid extractions?
BR: What’s happening there is, the patient probably has temporomandibular joint dysfunction and the condyles are probably back too far. And what’s happening is, all night long the lower jaw is coming forward and the lower anteriors are pushing all those teeth forward and it’s causing that space to open up. It takes place over a number of years, it may take five or 10 years to do it, but that is what’s happening. We see that a lot. I’m not saying you can’t take out bicuspids because there are specific cases where it’s a good idea. But I think in the past far too many bicuspids were taken out. In fact, I took out too many bicuspids more than 30 years ago. And I tell my patients that I’m doing it a little bit better today because 25 years ago I didn’t like my bicuspid extraction results either. I was looking at facial profiles that looked very flat. When I started using functional appliances, I was developing beautiful faces. I think anybody doing cosmetic dentistry has to think about creating a good foundation before you do cosmetic dentistry. Cosmetic dentistry is the roof in the house, but it helps to have a good foundation of orthodontics to build it.
Q8: You make a great point. The cosmetic dentistry we do at the lab is highly invasive and typically needs to be redone every seven to 10 years. And a lot of times we’re taking some, or all, of the enamel off the teeth to achieve our results. If you truly want to achieve esthetic success in the most conservative way, you have to be comfortable with diagnosing and/or treating orthodontics. And frankly, the only reason — with the exception of tetracycline — that porcelain veneers even exist is because of dentistry’s failure to diagnosis orthodontics early enough in children.
BR: I agree, but I think the orthodontic profession has to take partial blame for this. They historically waited a long time to initiate treatment. But if you look at the orthodontic society’s website today, they are recommending children be screened by age seven. So a lot of orthodontists are now switching their practices to early treatment. I remember something you said at the end of my course. You said that patients should take a class action lawsuit out against the dental schools for their failure to train dentists to diagnose or treat an orthodontic case. You said we learn fixed and removable prosthodontics, we learn periodontics, we learn endodontics. All the other specialties are taught to us in dental schools except for ortho. The orthodontists basically taught us to refer patients out and discouraged us from doing it.
By the way, Mike, this doesn’t happen in just North America. I’ve taught in many places across the world — Hong Kong, Poland, Australia, England, Scotland — and everywhere I’ve been it’s the same story. I just think that dental schools have to change. It was interesting because I just spoke to an orthodontist in South America who actually took my course many years ago in Atlanta. And he told me all general dentists in South America do functional appliances. They don’t do braces, they don’t do fixed braces, but they do functional appliances. They develop arches, they fix airway problems, and they bring the lower jaws forward when they’re deficient. They just treat the kids orthopedically. Because remember, orthopedics is to fix the bone problems and orthodontics is to fix the tooth problems. So I think we need to get better at orthopedics.
Q9: So once the South American GPs finish the orthopedic portion of the case, they send the patients to the orthodontist to do the fixed braces?
BR: That’s right.
Q10: That actually makes a lot of sense, doesn’t it?
BR: It does. I mean, the orthodontist could certainly do that and teach that. But again, only orthodontists who do that kind of treatment should be in the dental schools’ teaching. What I feel is, any orthodontist who starts getting into teaching GPs seriously gets so much slack from his colleagues that it just makes it very uncomfortable for him. But I’m lucky because in Las Vegas every year at my big meeting, I’m able to invite some world-class orthodontists who really want to share their knowledge and help the entire profession. I invited an orthodontist to speak once and he said, “Well, I’m not very popular if I come to your meeting.” And he designed this fantastic appliance, a wonderful appliance, which I use a lot in my practice. And I asked him: “Did you design that appliance to help just orthodontists and their patients? Or did you design that appliance to help everybody? All the patients in the world?” I said: “I want you to think about that. I’m going to call you back in three days, and I’m going to ask you if you’re going to speak at my convention.” I called him back three days later, and he said: “You know what, you got to me. You’re right — I designed this appliance for everyone, not just orthodontists. And every general dentist who’s competent should be able to use this appliance to help their patients.” I thanked him very much, and he came on the program, and he was a big success.
Q11: I feel like I got a pretty darn good education at UOP; I got to do six veneers back in 1988 while I was in my last year there. However, my big beef with dental school is that when I think back on my ortho education, it seems like it was about 14 minutes long. I remember we had some ridiculously difficult wire-bending task to complete. And basically, the take home message was: “See, ortho is tough. Don’t even think about doing it: Refer.” My point always was, if we received that little knowledge — we didn’t even know barely enough to diagnose, let alone treat — and if we got that poor of an education in endo or perio or anything else there would be a class action lawsuit by the American people because you’d have to go to another country to have a root canal since none of us were taught how to do endo. I know there’s a limited amount of time to teach dental students, but this is pretty important stuff. Not that any of it’s not important stuff, but I could easily make an argument that learning how to do functional orthodontics is just as important as learning how to do dentures!
BR: That’s right. Well, my course is eight days long. At the end of those eight days — obviously there are four manuals that go with it and some lab work — but at the end of those eight days, I’ve got dentists doing simple cases. They’re graduating and they’re coming out doing simple cases. You know, if you added eight days to any orthodontic curriculum, which you could easily do, you could reduce some of the information on other courses and get general dentists to have a basic understanding of what they’re doing to help patients. Seventy percent of kids have some type of malocclusion. That’s a huge number of children in your practice that could benefit. And you don’t have to do any external marketing — they’re right there and they trust you. All those patients in your practice trust you and like you and they will listen to you.
I don’t mind selling, but I’d rather just present the case and have them say yes. It’s just so much more professional. And I don’t have to sell ortho — it sells itself. I mean, all mothers want their children to have straight teeth; they want them to be healthy.
Q12: Most dentists don’t seem to enjoy working on kids. Most GPs want to have an all-adult practice that they can do crown and bridge on. They don’t like doing fillings on the kids because that doesn’t bring in a lot of money. It’s really pleasing when you get to work on kids without a needle, without a handpiece, and the same parents who couldn’t afford two crowns on themselves can suddenly afford the same $2,000 for their kids. Have you noticed that, that parents are much more willing to spend money on their kids than themselves?
BR: Yes, from one room to the other. I remember one time I suggested a crown, it was $1,000 and the mother said, “I can’t afford that.” Her little girl was in the next room having a prophy and a cleaning and fluoride treatment, and I walked in and said: “Geez, she’s got a narrow jaw here. She’s got a crossbite in the back. You know, that’s going to be about $1,500. Plus the orthodontic records, that’s going to be around $2,000.” And the mother said, “Well, when do we take the records?” And, of course, I said, “Do you mind telling me why you just couldn’t afford the crown for $1,000?” She said: “Children are different. My child gets whatever she needs. We will find the money, and we’ll pay it on time.” I said: “Of course. We’ll set up a payment plan for you. You pay so much a month.” And she said: “Well, we’re going to get that done. There’s no question.”
Now we’re into a situation where the U.S. is in a recession. You and I talked about that a couple of days ago. You said elective dentistry in the lab is down a bit. Well, I can tell you my practice is not down. We’re averaging about six new patients a day in ortho, TMD and sleep apnea — we’re just really humming along. And each one of those patients could be a significant amount. If you do just functional appliances, it is about $2,000. But if you do the entire ortho case, it’s about $6,000 in my office. There’s a lot of demand for health. There’s a lot of demand for someone who can do a case without extracting permanent teeth. And there’s a lot of patient demand to use functional appliances in order to avoid orthognathic surgery, in cases where it’s appropriate.
Q13: Isn’t it funny how when it comes time to tell adults about their proposed treatment, we get into case presentation and how to educate your patient to get them to say yes. If you have a patient who needs $6,000 worth of crown and bridge, you have to really kind of put on a sales cap to convince them this is the right thing for them to do. And you’re saying that you tell the same patient their kid needs $6,000 worth of ortho and they’ve already got their checkbook out of their pocket!
BR: It’s great. I don’t mind selling, but I’d rather just present the case and have them say yes. It’s just so much more professional. And I don’t have to sell ortho — it sells itself. I mean, all mothers want their children to have straight teeth; they want them to be healthy. And I think if you talk about the airway and you talk about the breathing and you talk about the sleep apnea and you talk about the healthy temporomandibular joint, you talk about all the things that functional appliances deliver, and more room for your tongue to speak, all of the things you can do for their kids, mothers say, “You know what, I want to be in your practice.” And then, that builds my general practice because they want to switch from their dentist to me. That’s because their general dentist said, “Wait till 13,” and the orthodontist said, “Wait till 13,” and the mother said, “It doesn’t makes any sense.” And mothers are smarter nowadays. They talk. I mean, they go to soccer practice, they go to church, and they go to the grocery store, everywhere, talking to other women. And if one woman has been to my practice or to another practice that does functional appliances or early treatment, that’s where those mothers are going to head.
Dr. Michael DiTolla: There is absolutely a secret society of women that men don’t know about because men are typically at work. But it’s true: if you’re off for a day and you take your kid to soccer practice, you see this. And the No. 1 priority in these mothers’ lives is making sure their kids are healthy and that they look good.
BR: I had a referral today from that. The guy came in and I said, “Well, how did you find us?” And he said, “My next door neighbor comes to you and really likes you.” We had another consultation with someone else, and I said, “Are you coming here because you didn’t like what he said?” And he said, “No, no, you were just so highly recommended we had to meet you.” So, word of mouth spreads. And if you do a good job with these patients — I mean, it’s the same as any business or any practice — you’re going to get referrals. And we get referrals. I’m really happy with that. We do treat our patients well.
Q14: And just as a little bit of disclosure, when I first took your course, the eight-day course, I went back and — as most dentists are — I was afraid to do my first ortho case, like most dentists are terrified to place their first implant. So I didn’t do any ortho cases right away. Then, when it came time where I had some patients lined up, I had forgotten a lot from the course. And you were generous enough to let me come back and audit the course a second time. When I came back the second time having done some screenings and records, I knew what questions to ask and I was ready to go. So once I took the course a second time, I was able to go back and start treating these kids with a bigger degree of confidence. Are you still letting attendees audit the course like that after they take it the first time?
BR: Absolutely. If they want to take it again, they can take it for half price. If they bring someone with them, they come free. But what I’ve just done, Mike, is my internet course. I’ve already got 30 people lined up just to know how much I’ll charge. And I’m going to be very fair to the first 50. I’m going to give a deal to the first 50 and then it’ll go up, up, up. And that is going to be a really good way to learn because there’s going to be a 20-minute session and then there’s going to be a test at the end of every 20 minutes. And then you’re going to get hours of continuing education. Plus, you’re going to get notes. I think the internet is a really good way to learn. So maybe they won’t have to retake the course. Maybe they take it once and then if they take the internet course, it’s a nice review and they can do it in their home. They won’t have to travel. Nowadays, you have to deal with the hassle of airfare and air travel, the cost of gas and hotels and everything else.
Q15: Also, Space Maintainers® Laboratory had a big part in why I started to do ortho cases because I was really nervous. Even after the second time I was nervous to start some of these cases. And it was right at the time Space Maintainers came out with something called The Second Opinion, where you send all the patients’ orthodontic records to them and you get a 120-page “cook book” on how they suggest to treat each patient. I did that for the first 10 or 15 patients I treated. And then once I realized everything was just like you said it was going to be in the course, I tapered off The Second Opinion for the easier cases. Do you think that type of hand holding is a good idea for the GP who’s doing his first few cases?
BR: Absolutely. They are a great lab. They’ve got a lot of good education materials, brochures, and they have great people on the telephone to help you with cases when you call in. And they also have The Second Opinion. And, as you mentioned, when dentists come to my courses they’re allowed to bring cases, models and photographs — all the things we teach you how to do with the records in the course and the X-rays — and I now have assistant instructors at the courses. And the assistant instructors and I review cases at no charge. We’re there to make sure everything goes well. You know, I’ve never had anyone successfully sued who took my course and I’ve trained 10,000 dentists. Anybody who follows my system and takes the records the way they’re supposed to and who doesn’t do the difficult cases we teach them not to do.
Q16: Give me a typical timeline for one of these two-phase ortho cases. Let’s say an 8-year-old patient comes in with a Class II malocclusion.
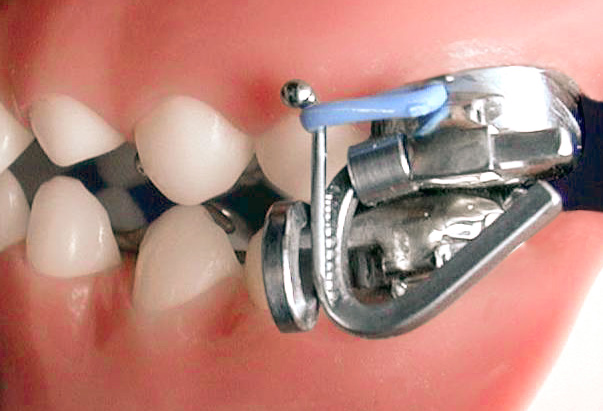
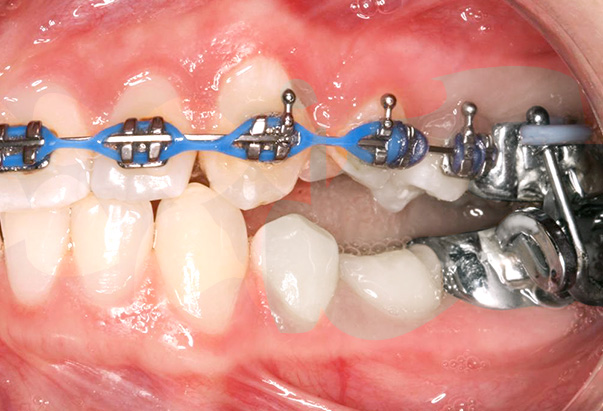
BR: What I would do is put in an appliance to widen the upper arch. That would take about four months. Then I would probably put in a Twin Block, which would move the lower jaw forward. That would take about seven months. And then I would probably modify the Twin Block into a Twin Block 2, and hold her there until she’s maybe 10 years old. She just wears the appliance for another six months. So treatment time so far would be 17 months. And I wouldn’t have to see her every month because the appliance works almost by itself, so I’d see her every two months. And the mother would pay me about $200 a month and I’d check her for about five minutes. We’ll spend more time cleaning up the room and getting it ready for the next patient than actually seeing the patient. I just make sure to check the appliance, make sure it’s not hurting, and adjust the appliance accordingly. Turn the screws or whatever you have to do. Then, I would just wait until all the rest of the permanent teeth erupted. And many times when I do that, you deal with 80% of the malocclusion. Then when the permanent teeth erupt, I might only be in fixed braces for nine months. So I would tell the patient: “Look. My usual fee is $6,000. Let’s do Phase 1 for $2,000. If you have to do Phase 2, the most I would probably charge you is $4,000.” And then if the patient comes back, you say: “Look, I’ve got a conscience. I really can’t charge you $4,000, I’ll only charge you $3,500 because it’s only going to take me six months.” The mother’s quite happy. But I say, “Because I’m losing so much money on this case, you have to refer me to at least two more patients.” And believe it or not, the mothers say, “OK, I will.” It’s just unbelievable…they do. So then, wouldn’t that be nice if you had a child where you could treat early and wear these appliances for 17 months, which are no trouble for the kids to wear.
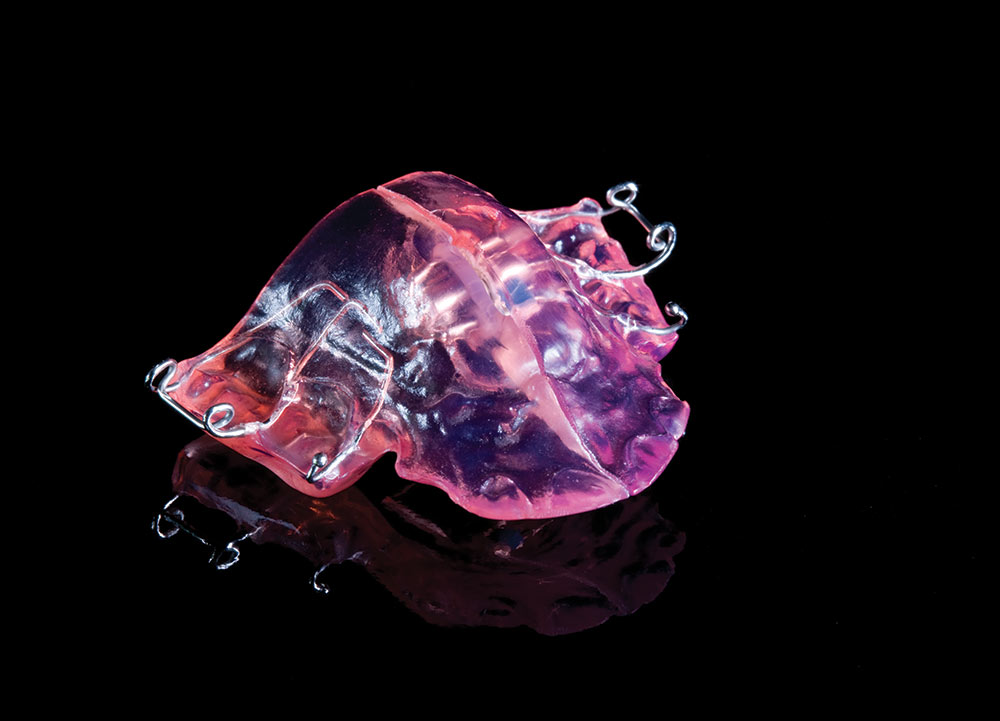
Q17: And isn’t it surprising how if you personalize the appliances for the kids, with a flower or a team logo, they are more apt to wear them?
BR: Oh, yes, absolutely. And I tell them, “Make sure you take this and show it to everybody else in your class and see if anybody else has one — because I think you’re the only person in the world who’s got it.” So then they’re showing the appliance off. And you are right: you personalize it, which Space Maintainers will do for you. They’ll send you a chart and let the kids pick the color they want, which is fun for the kids.
My office is a very upbeat office, and I’ve got to do a lot of consultations all day. And I hear laughter all day. You just hear kids laughing and their parents laughing and everybody’s having a good time, which is different from some dental offices. And quite frankly, I’m not tired. We see 60 patients a day but it’s not tiring because I’m doing sleep apnea and some TMD cases. I’m also getting some very difficult patients referred to me by some general dentists who take my courses — they send me all the tough ones and they do the easy ones — so it takes me a little longer to do some of those cases. So we can really only do about 50 a day, but it’s just a pleasant way to practice. I’m so happy I got into ortho; I really feel I’m helping a lot of patients and it’s very rewarding.
When I look back, I think I was thinking of the money. I was thinking I can get a room going in ortho and I don’t have to be in there that much. We can generate some income there that’s nice and helps the bottom line and helps me feed my family. But eventually, when I sat back down to think about it, it’s more about the personal satisfaction. After a while, you have enough money and you really want to feel that you’re doing something good for your patients. And I feel I’m significantly improving the health of my patients. I believe that most dentists went into the profession to help people, I really do. And I’m not saying that when you put on 10 veneers that you aren’t improving their smile and their self-esteem, but I am improving their health as well. Especially when I treat snoring or sleep apnea. We really don’t have time to talk about that today, but maybe someday we can talk a little bit about snoring and sleep apnea because that’s another huge area of growth for any practice.
After a while, you have enough money and you really want to feel that you’re doing something good for your patients. And I feel I’m significantly improving the health of my patients. I believe that most dentists went into the profession to help people, I really do. And I’m not saying that when you put on 10 veneers that you aren’t improving their smile and their selfesteem, but I am improving their health as well.
Q18: Fifteen years ago, I don’t think you were talking much about snoring and sleep apnea. How did you get started with that?
BR: Well, I started noticing that an awful lot of my patients who were Class II malocclusions and had TMJ problems were also snoring and sleep apnea patients. I started reading about how bad sleep apnea is for your health. Forty percent of patients who have heart attacks have sleep apnea. Forty percent to 60% of diabetics have sleep apnea. Over 50% of patients who have a stroke have sleep apnea. GERD — gastroesophageal reflux disease — is also associated with sleep apnea. So all these medical problems are being caused by sleep apnea. I thought, if I don’t deal with the sleep apnea, how can I make my patients healthier, number one? I need to open up the airway because a lot of these patients are depressed, or they’re depressed because they’re not getting much sleep and they’re tired all the time, or they’re depressed because they’re in pain since their jaw is back too far. So the same patient who has sleep apnea is the TMD dysfunction patient. Because when your jaw is back, your condyles are back pressing on your nerves and blood vessels. And when your jaw is back, your tongue is back blocking your airway. When the tongue partially blocks the airway it’s snoring. But snoring is not dangerous to your health — just bad for your relationships. Probably 50% of my patients are coming in from their wives telling them: “Get in there. Otherwise, you are in a different bedroom and we’re going to get divorced…or something.” The other 50% are stopping breathing. They have been to the medical doctor who sent them to a sleep center for a polysomnogram — an overnight sleep study — and they’ve been diagnosed with sleep apnea. And the medical profession likes the CPAP machine, which is the thing that goes over the nose and looks like Darth Vader and blows air up your nose all night. A lot of patients can wear it, but a lot of patients can’t. So the patients who can’t wear it would come to me and say, “Look. I can’t wear this medical device but I’ve got the problem; can you help me?” And recently, the American Academy of Sleep Medicine came out with a statement that said: “For mild to moderate cases of sleep apnea, oral appliances are the treatment of choice.” So, when I read that in 2006 I realized, Mike, that we are now getting the backing of the medical profession to make oral appliances for the mild cases and slightly moderate cases. But for severe cases, we send them to the medical profession for the CPAP machine. It’s been a huge benefit to my practice, and now I really feel I’m treating all patients.
If I could just tell you one quick story: I had a patient today who came to me five months ago for snoring and sleep apnea. I examined her and I found her jaw went back — she had an overjet of 7 mm. Her tongue was back too far, blocking the airway, and she had sleep apnea. Then I examined her TMJs and found that she had temporomandibular joint dysfunction. She had headaches every day, she was on three medications a day, and she was very, very sick. She was very tired all the time because of sleep apnea, tired all the time because of the medication, and just really a very unhappy lady. So here’s a patient with an orthodontic problem. Here’s a patient with temporomandibular joint dysfunction and signs of sleep apnea. That’s why I’m doing all three, because they’re all related. I said to the patient: “I’m going to put you in a MARA appliance, which is going to bring your jaw forward. I am hoping that when I do I’m going to solve all three problems.”
Today she told me in front of another patient that since I put the appliance in, her headaches are gone. Her sleep apnea is gone, her snoring is gone, and she’s just a different person. She’s off medication. She did admit to me that she’s had two headaches in five months, but they were so minor she could take over-the-counter Tylenol. Just those two small headaches in five months, and she said she used to have them all the time constantly, migraines, everything. And she was on three pain medications daily, 24 hours a day. She said, “I’m 60 years old and I feel like I’m 40.”
I would encourage dentists to broaden their horizons because there’s a tremendous need for early diagnosis for kids. There’s a tremendous need to learn about TMD. Most dentists are scared stiff of TMD — they don’t want to get near it. But snoring and sleep apnea is a much shorter learning curve; you can learn that in a much shorter period of time.
Q19: That is amazing because I think it really gets to the heart of what you’re doing. And that’s why you’ve always gotten me excited about this. Because when we put veneers on a patient, every once in a while we’ll get a patient whose self-esteem was really hurt by their smile. So, when they see their new teeth for the first time they might cry because of the esthetic improvement. But we’re doing an esthetic improvement — and that’s fantastic — but what you’re doing on some of these patients is a massive quality of life improvement. And you’re taking somebody who lived in pain with these headaches on a daily basis and removing those — you must end up being a hero to a lot of these patients.
BR: (laughs) It’s terrific, but you’ve got to make the right diagnosis, you have to take full records, and you have to learn what you’re doing. There are courses everywhere for dentists to take. Dentists can take good courses. Not just mine — there are lots of good courses they can take. But I would encourage dentists to broaden their horizons because there’s a tremendous need for early diagnosis for kids. There’s a tremendous need to learn about TMD. Most dentists are scared stiff of TMD — they don’t want to get near it. But snoring and sleep apnea is a much shorter learning curve; you can learn that in a much shorter period of time.
Q20: So you’re teaching the ortho courses, and now you’re teaching snoring, sleep apnea and TMD courses as well?
BR: I am, and attendance on those courses is maybe 15 or 20 dentists. They’re not like the ortho courses that usually have 40 dentists because more people are interested in treating kids orthodontically with these appliances. And that’s probably a good way to start. That’s the basics. I would encourage dentists to take the ortho course first and then see if they like the science of sleep apnea or TMD. But I’ve transitioned a lot of dentists into those courses and most of the dentists going to those courses have taken my previous courses, and their practice is rolling along. What I’ve told them works, they are happy with the results, they feel good about what they’re doing for patients, and they just want to get better.
MD: For dentists who are interested, what is your website so they can look into getting more information?
BR: It is rondeauseminars.com.
MD: I just wanted to say that since the first time I took your course you’ve struck me as a really open-minded dentist, somebody who is willing to speak the truth whether it’s popular or not. And while the things you said 15 years ago made me shake my head a little bit then, I look to you now and I think you should feel somewhat vindicated — they appear to be true and the research backs it up. And certainly my own clinical experience backs it up as well. You taught me how to be a better dentist and make my patients happier and make them healthier at the same time, AND make more money. And there is nothing wrong with that. I want to thank you for your time today. You shared some really important ideas with our dentists, and I look forward to doing this again with you in the future.
BR: Thanks a lot, Mike. It’s really a pleasure to talk to you again.
To contact Dr. Rondeau, email brondeau@rondeauseminars.com or call 877-372-7625.
The functional appliances presented in this article are courtesy of Space Maintainers® Laboratory (Chatsworth, Calif.; 800-423-3270).