My First Implant

It’s not often that I praise patients for not following the advice of their dentist, but after placing my first implant that is exactly what I did. Ten years earlier, when this 32-year-old male patient had tooth #19 extracted, his dentist suggested they do a 3-unit bridge to replace the missing tooth. The patient didn’t like how much it was going to cost, but more importantly, he opposed the idea of prepping two adjacent teeth to replace one missing tooth, especially when he had no restorations on the lower arch. I told the patient he made a good decision not having the bridge done, since that is what allowed us to place the implant without harming either of his adjacent teeth. Fixed bridges seem to create as many periodontal problems as the restorative problems they were meant to resolve. Throw in the fact that the two abutment teeth could potentially need endodontic treatment now or later, and a compelling case is made for the single tooth implant.
This 32-year-old male patient presented with a missing lower left first molar. I had been instructed to look for a patient like this for my first implant: young, healthy and with lots of bone. I liked the idea of getting my feet wet in the posterior, where esthetics would most likely not be an issue.
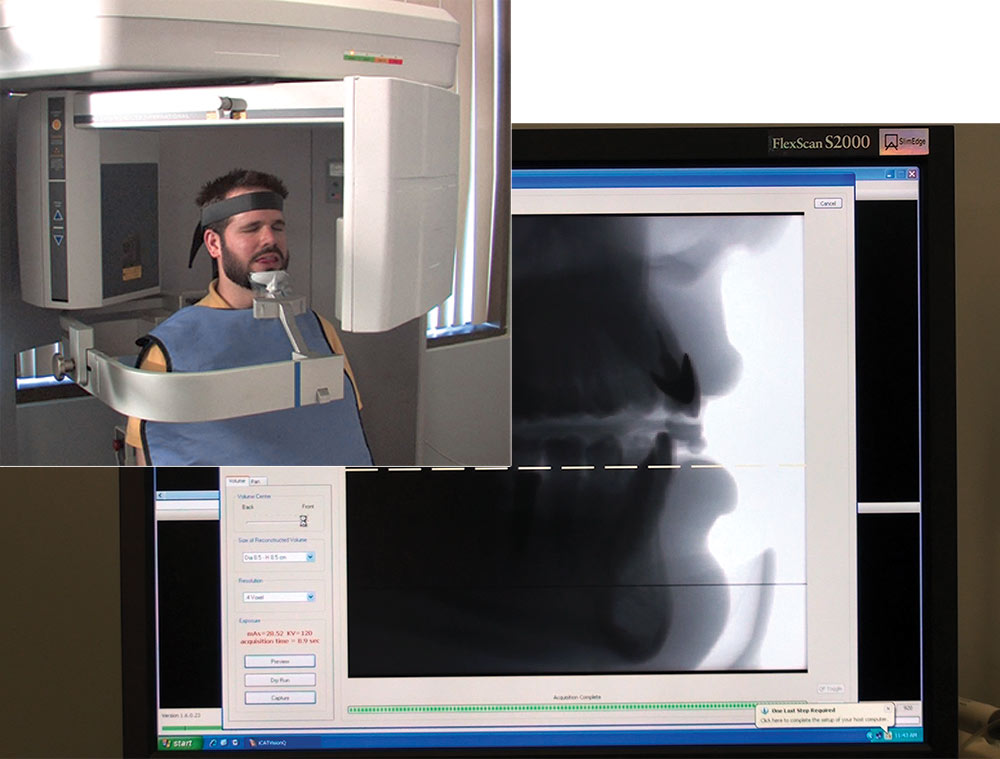
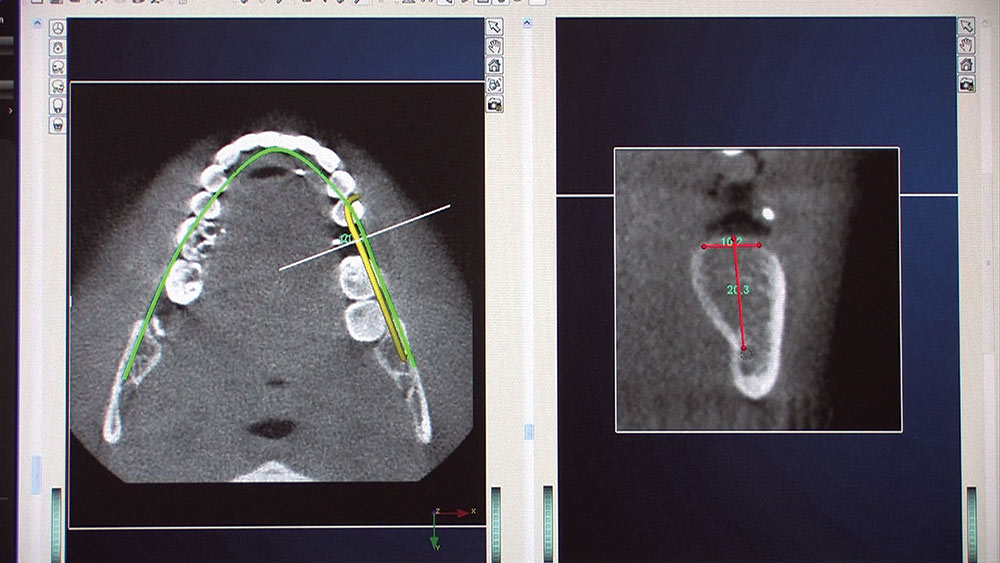
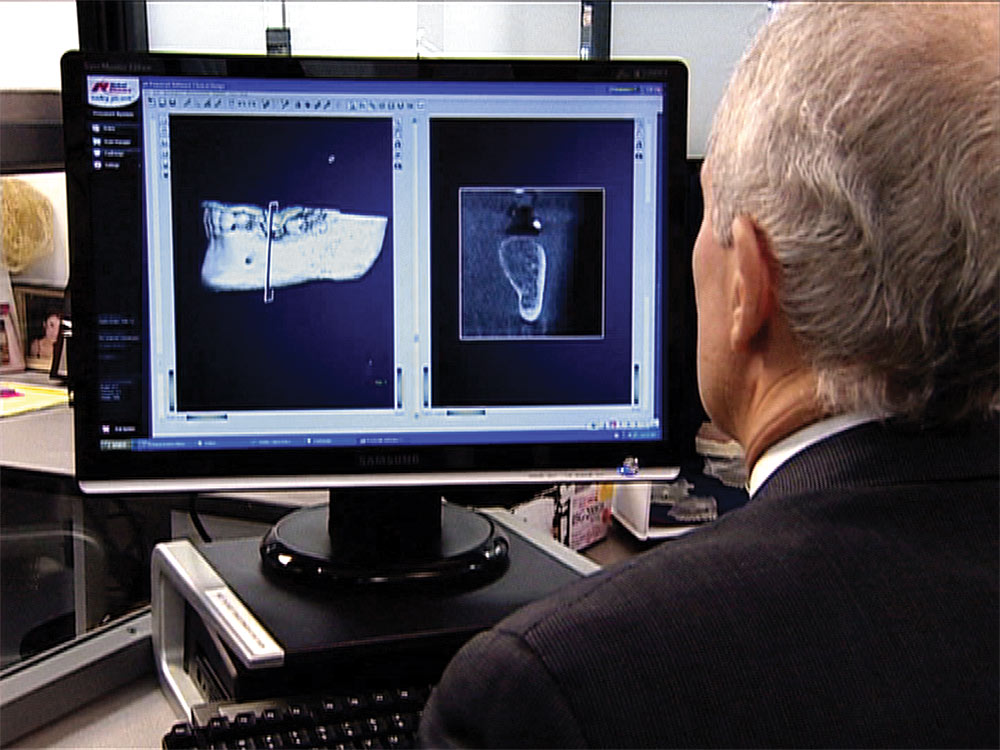
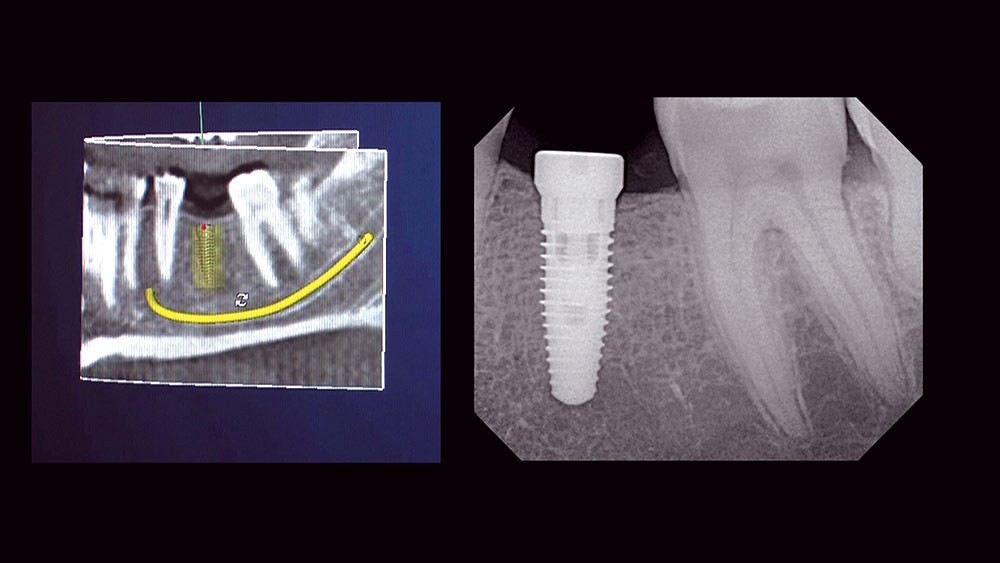
I’ve always known that patients would rather stay in my office than be referred to another office, but I was afraid to surgically place an implant. Up to this point I had been restoring implants for some time and had taken numerous implant courses. However, when our implant department convinced me that Digital Treatment Planning technology would eliminate the guesswork, I decided I was ready to give it a try.
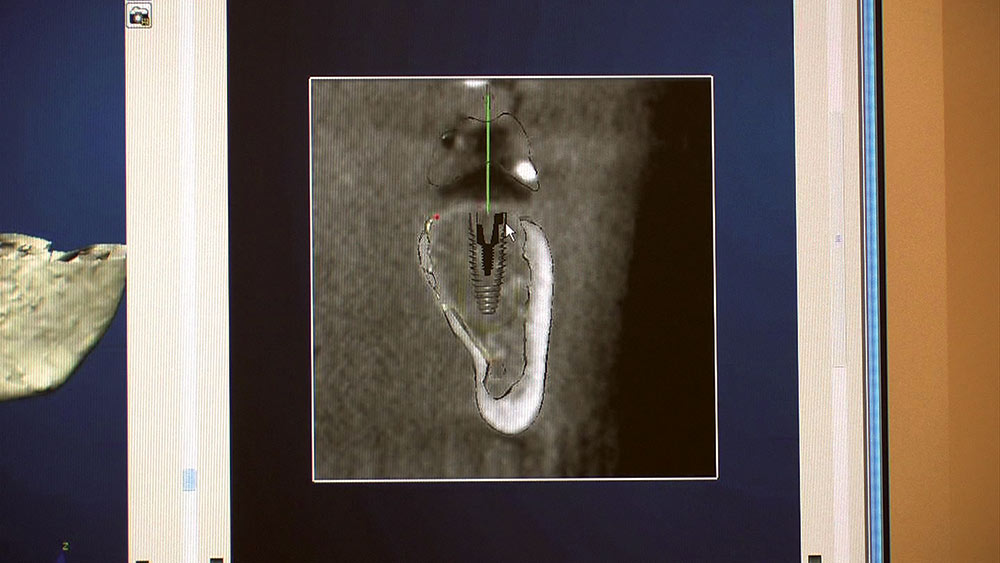
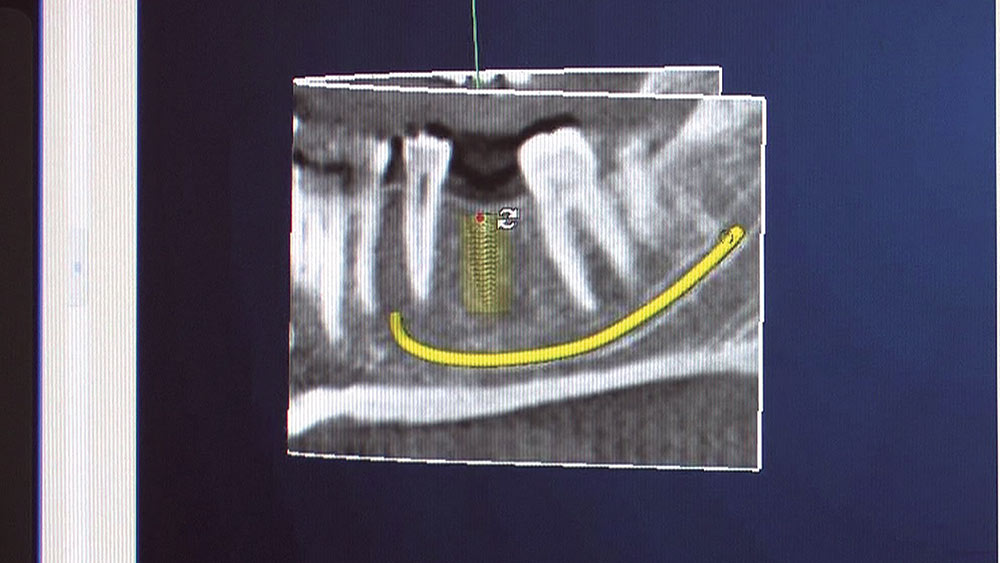
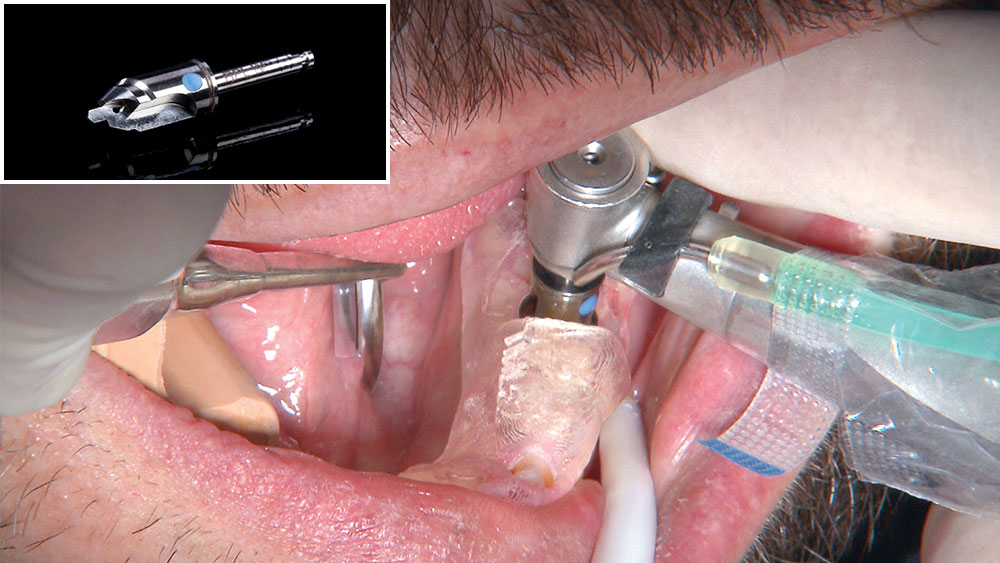
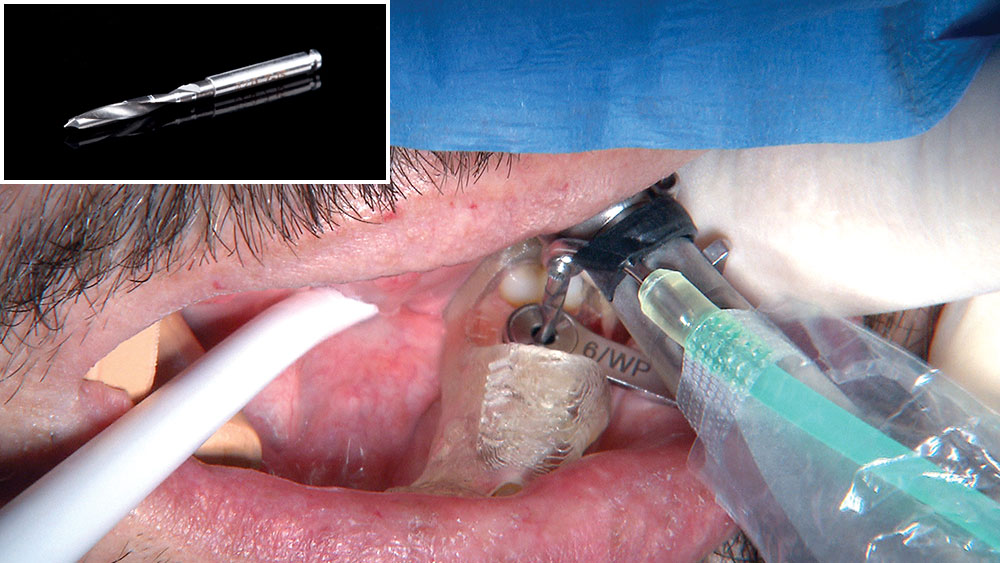
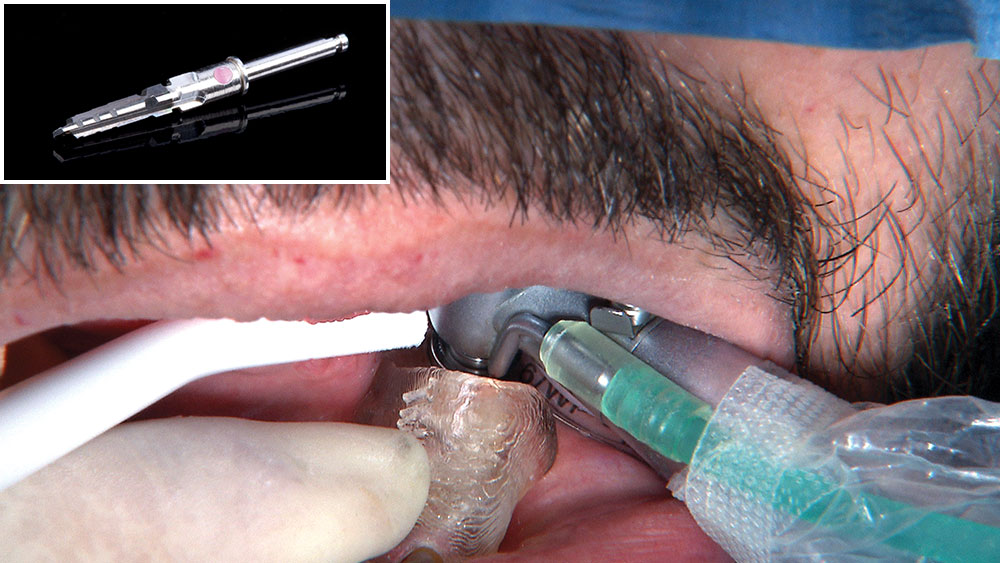
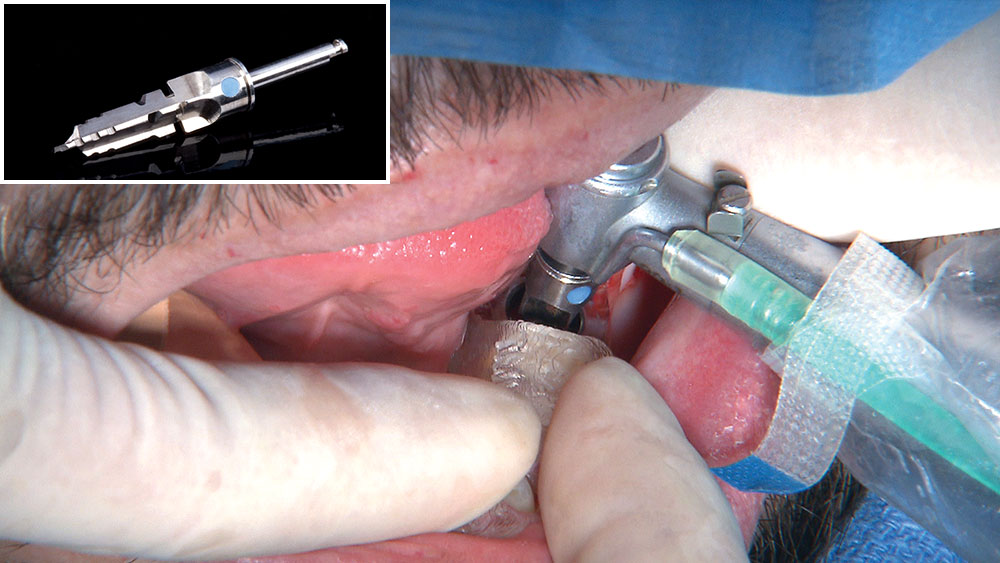
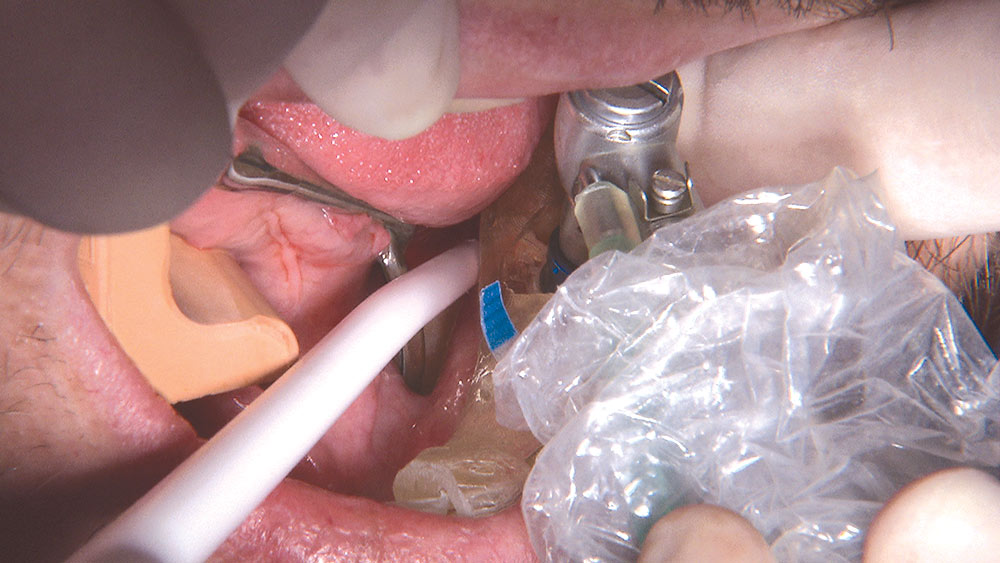
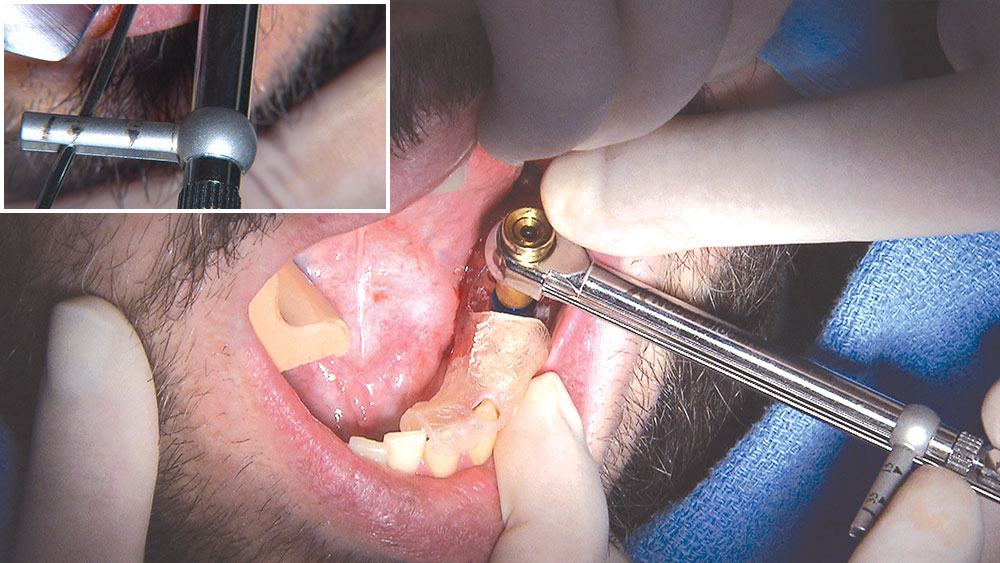
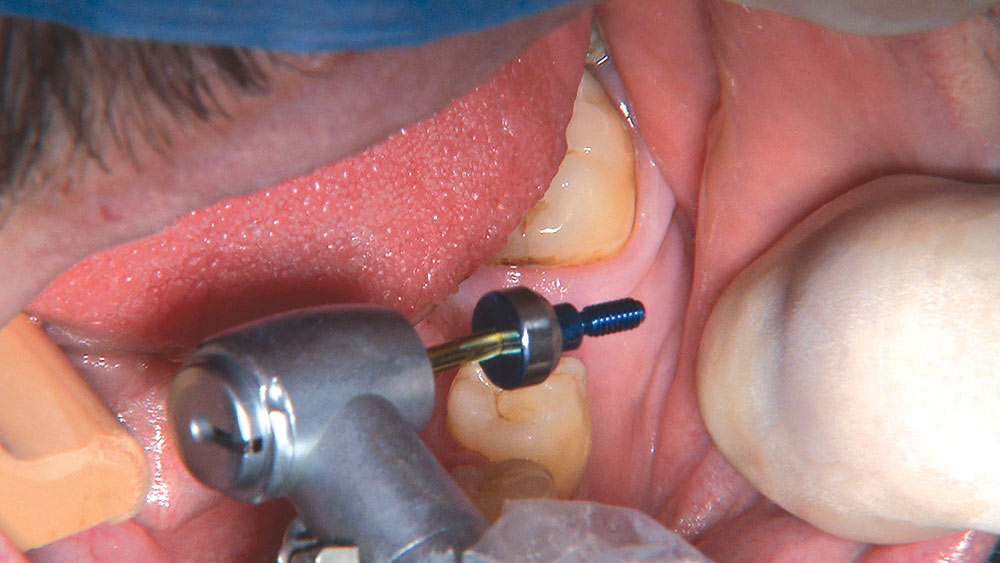
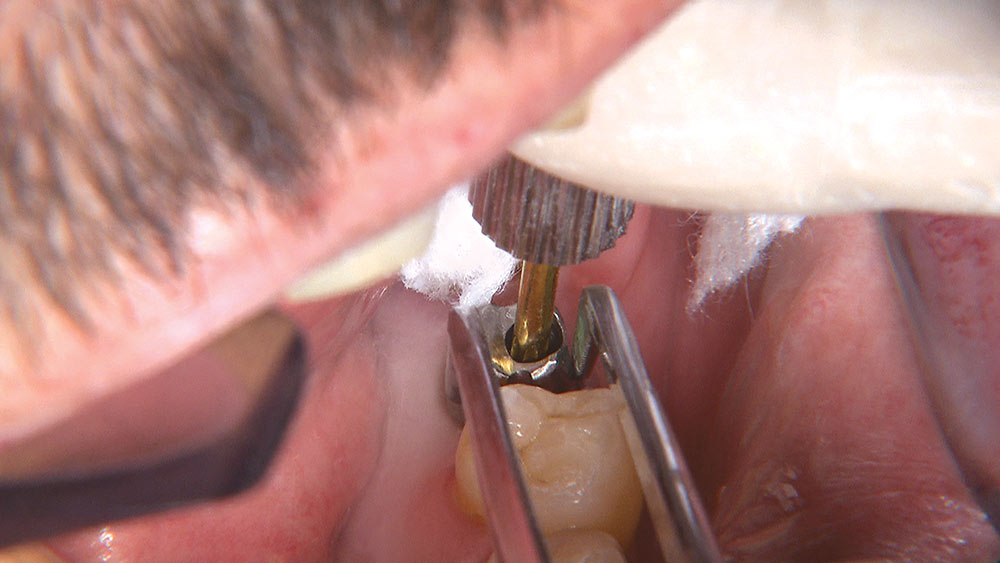
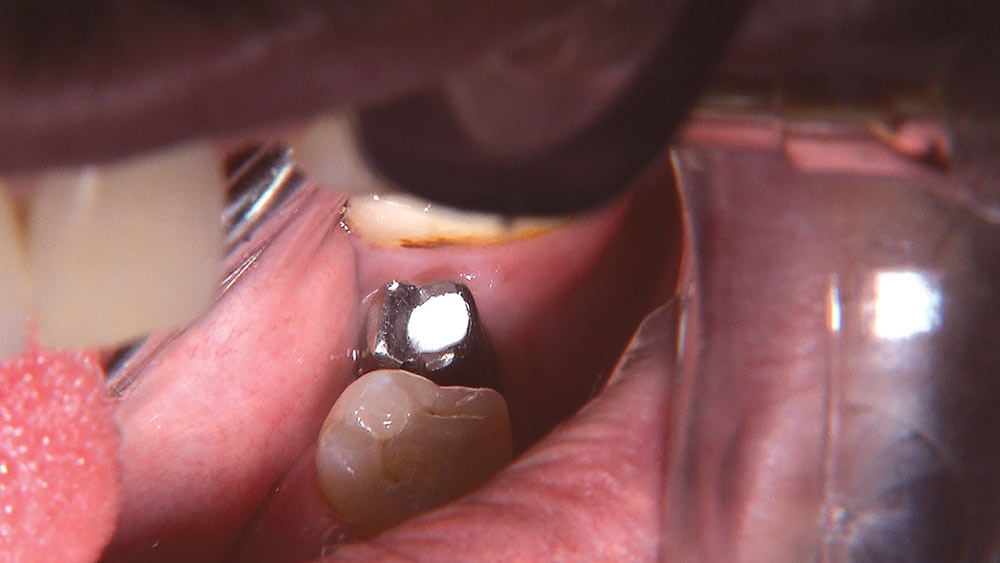
Here are some step-by-step pictures of my first implant. I can honestly say it was the most fun I have had in a long time, and it was easier than almost any crown prep I’ve recently done. I wish there was this much technology available to walk me through molar endo, wisdom tooth extractions or multiple-unit bridge preps. Take advantage of this technology and utilize the Digital Treatment Planning expertise of Glidewell’s implant department. If your first experience is anything like mine, you will immediately start looking for your second implant case. Or, if you are a part of a surgical-restorative team, you will find that this service provides an easy way to integrate and utilize this technology with your implant cases.
Because we planned on placing a NobelReplace™ implant, this case was done utilizing the NobelGuide™ Guided Surgery System. This photo essay will walk you through the process.
Four Months Later
For more information on Glidewell Laboratories Digital Treatment Planning services, call 800-497-3692.
NobelGuide and NobelReplace are trademarks of Nobel Biocare (Yorba Linda, Calif.). STA is a trademark of Milestone Scientific (Livingston, Calif.). Easyshade is a registered trademark of Vident (Brea, Calif.). Inclusive is a registered trademark of Glidewell Laboratories (Newport Beach, Calif.).