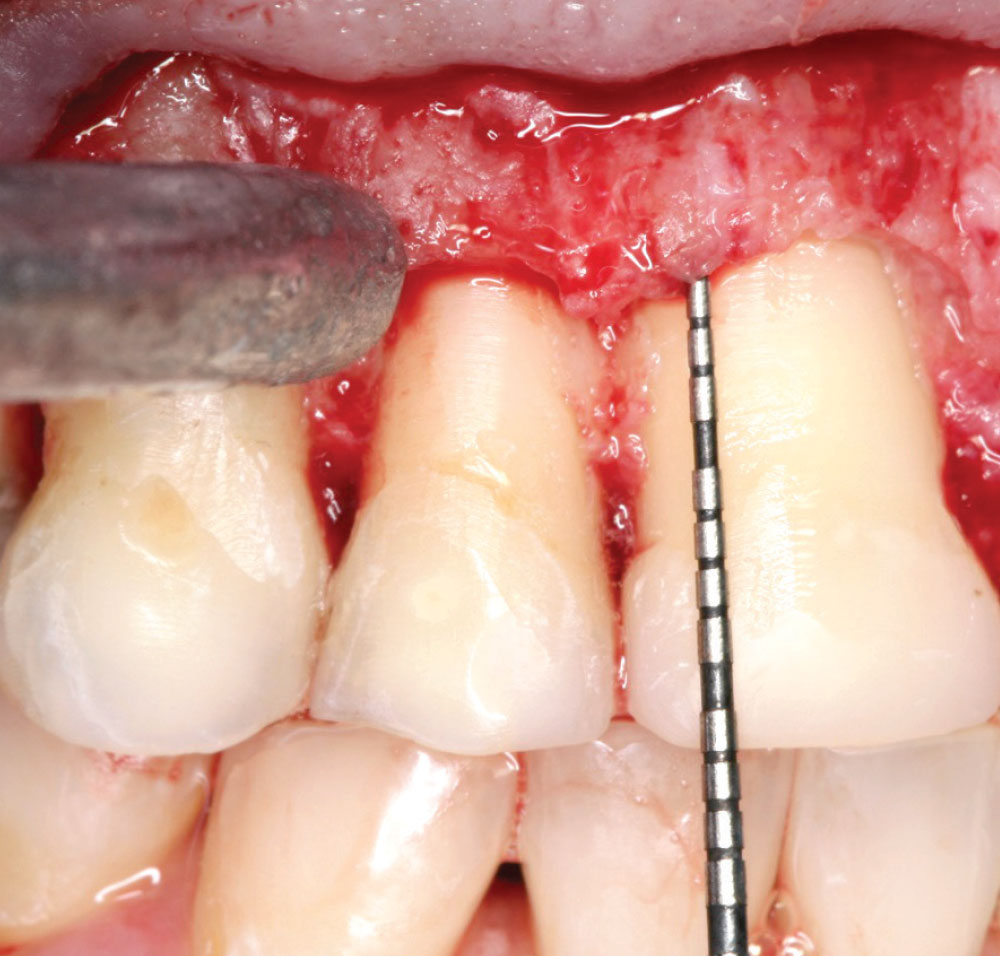
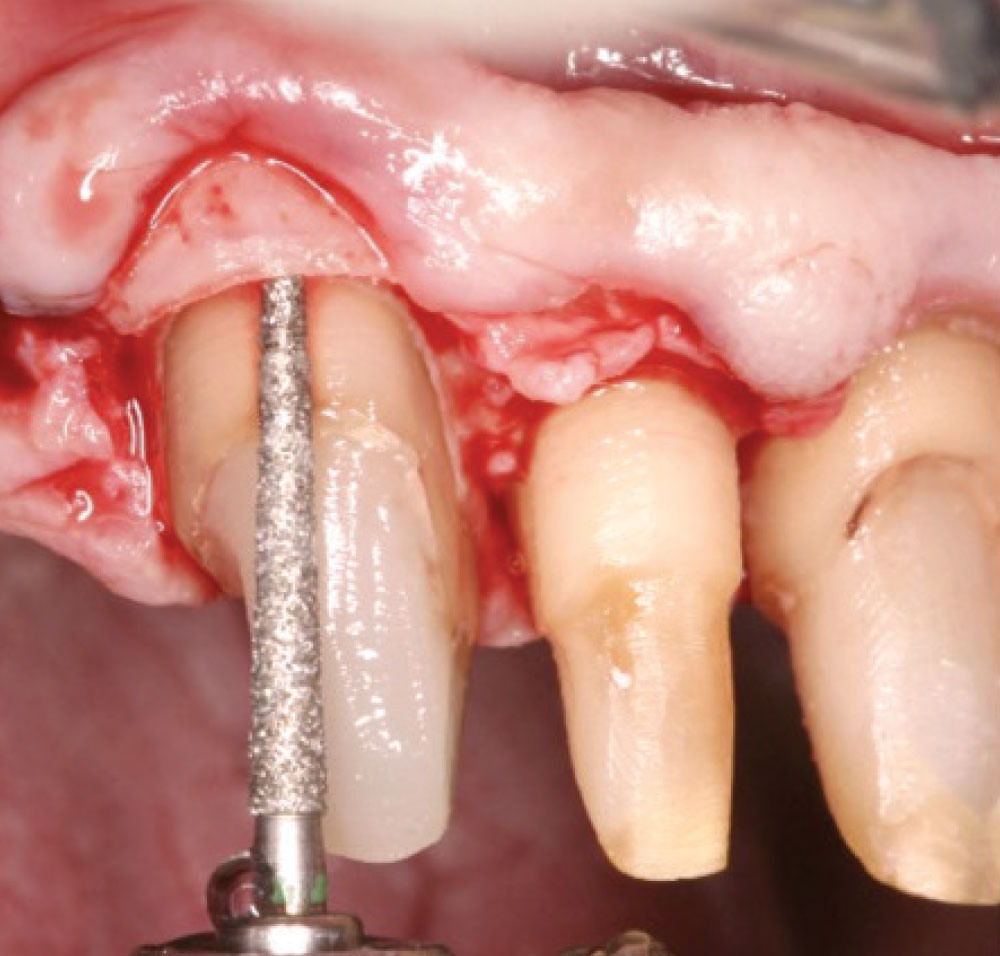
Periodontal Photo Essay: Is Closed-Flap Crown Lengthening a Biologically Sound Procedure?
Objective
The objective of this article is to discuss the biological aspects of bone and the changes that occur when it is infringed upon either through disease or during the correction of certain periodontal conditions. It will discuss the correction of osseous defects and why these procedures are necessary to create a long-term stable environment. When a comparison is made between certain periodontal problems stemming from either biologic width invasion or periodontal disease with closed-flap crown lengthening, similarities suggest that closed-flap crown lengthening is an unsound biologic procedure.
Case 1
Case 2
In this case, you will notice that the defect, which is caused by biologic width invasion, mimics the defect caused by closed-flap crown lengthening in the first case. Both are biologically unsound.
Case 3
Case 4
Case 5
Summary
Without the ability to remove the troughing created by the vertical removal of bone, closed-flap crown lengthening is biologically unsound. Horizontal access and visibility are needed to create a sound biologic surgical procedure.
Dr. Daniel Melker is in private practice in Clearwater, Florida, and lectures nationwide. Contact him at 727-725-0100.