Getting the Lines Right

INTRODUCTION
In a perfect dental esthetics world, the maxillary gingival line and incisal plane, the upper and lower lip, and the pupillary line should be approximately parallel to each other.1,2,3 In addition, the incisal plane and gingival line of the maxillary anterior teeth should flow seamlessly into the gingival line and occlusal plane of the posterior teeth (curve of Spee). Ideally, the incisal plane and gingival line of the mandibular anterior teeth should also be parallel and blend with the aforementioned planes and lines,4 but proper occlusion and an attractive smile can be achieved even if the maxillary incisal plane and gingival line are not parallel with those of the mandible. The maxillary incisal plane and gingival line should, ideally, be parallel to the lower lip and interpupillary line even if the mandibular incisal plane and gingival line do not parallel those of the maxillae.1,2,3 The pupillary line and lower lip-line can normally be used as a reference to a horizontal plane because they are normally approximately parallel to a true horizontal plane (i.e., the floor or a tabletop).2
A comprehensive examination and consultation is important in treatment planning and explaining to patients these complex alignment cases. If the patient views quality photos of his or her smile and teeth as well as photos of similar restored cases, the patient can understand his or her condition and the reasons for periodontal surgery, incisal plane realignment and possibly the recommended restoration of additional teeth as part of the treatment plan.
A comprehensive examination and consultation is important in treatment planning and explaining to patients these complex alignment cases.
CASE REPORT
A 40-year-old woman in good health presented for dental examination with a chief complaint of unattractive PFM crowns on her maxillary central incisors. The patient also stated that she did not like her “gummy” smile2,4 or the color of her natural teeth2 and was displeased with her smile in general (Fig. 1). She was an executive with a large company and felt her dental appearance might be a stumbling block for advancement in the company.4,5 The author had previously completed a restoration for the patient’s sister, who presented with a similar condition. Following a preexamination interview, a comprehensive examination was performed, including a medical and dental history review, full-mouth radiographs, maxillary and mandibular full-arch impressions for study models, face-bow, 15 high-quality photographs of the patient’s teeth and smile, and a thorough clinical examination of the teeth, soft tissue, occlusion, muscles of mastication and temporomandibular joints.
It was determined that the existing crowns on the maxillary central incisors were deficient, and the maxillary and mandibular gingival lines and incisal planes were significantly not parallel to the pupillary line and lower lip-line (Figs. 1–3). The upper lip was maximally arched with lips in repose (Fig. 4),6 and there was significant maxillary gingival display with the full smile (Figs. 1, 2).7 The patient’s natural teeth were discolored.2
Diagnosis and Treatment Planning
At the consultation appointment, the high-quality photographs of the patient’s smile and teeth were viewed as well as pre-op and post-op photos of similarly restored cases. It was determined that periodontal crown-lengthening surgery would be performed on the maxillary teeth, extending anteriorly from the mesial of the right and left first molars, followed by replacement of the full crowns on the central incisors. Porcelain veneers would be placed on the lateral incisors, cuspids, and first and second bicuspids, to be done after six weeks to three months of healing, following the periodontal crown-lengthening surgery (the author normally waits three months). The periodontal crown-lengthening surgery and anterior restorations would create an incisal plane and gingival line parallel to the pupillary line and lower lip, as well as improve the hue, chroma and value of the teeth. It should be noted that treatment cost was a factor in this case for the patient.
Ideally, the same procedures would be performed on the mandibular anterior teeth. It was determined, however, that an improved esthetic result with excellent occlusion and function could be achieved without changing the incisal plane and gingival line of the mandibular anterior teeth. Bleaching of the lower teeth (Philips Zoom In-Office Whitening [Philips North America; Andover, Mass.]); a maxillary hard acrylic, centric relation occlusion nightguard; and minimum composite bonding of the chipped incisal edges of the lower anterior teeth were included in the treatment plan.
When incisal edge position is being changed, it is important to inform patients prior to treatment and in writing that, initially, their phonetics will change and may seem strange — especially the F, S, V, church and swish sounds. The F and V sounds are formed by the incisal edges of the maxillary incisor teeth touching the vermillion border of the lower lip. The S, church and swish sounds are formed by the passage of air between the incisal edges of the upper and lower incisor teeth.4,6 The patient will adjust nicely to the new incisal edge alignment and, in the author’s 35 years of experience, have no problem speaking after a day or two of practice. It is important, however, that the patient stand in front of a mirror and read aloud for 30 minutes or so, several times a day during the phase of provisional restorations to develop new speech patterns. This must be done while the patient is in the provisional restorations, just in case the individual is not able to adjust to the new alignment. If for whatever psychological or emotional reason the patient is not able to adjust to the altered incisal plane, the provisional restorations would be modified and tested to satisfy the patient’s phonetic requirements, sacrificing ideal esthetics. The provisional restorations, of course, are used as a matrix for the incisal plane of the final restorations. Again, this has never been a problem in the author’s experience.
It is important that the restorative dentist say to the patient initially, prior to tooth preparation: “You are going to love your new smile and will have no problem adjusting to the new teeth length. It may take a day or two, but, just like a child speaking clearly with missing or erupting front teeth, you will adapt quickly to the improved anterior alignment. If you will read aloud in front of a mirror for 30 minutes, twice a day, you will be speaking well and comfortably in a day or two.” Do not say, “Let’s try this new front teeth alignment and see how you like it.” Those words put doubt into the patient’s mind as to whether this is a predictable procedure, and this could invite unnecessary failure. This is a very predictable procedure, and the patient will do well with it. It will be different though, and patients need you, the restorative dentist, to give them the confidence that they will adapt to this different incisal plane alignment. Another example would be changing a golf grip, swing or stance. You need the assurance of your golf instructor that the different position is correct and will be better than the old positions.
A written consultation sheet of the agreed-upon treatment was prepared, and then reviewed and signed by the patient. The aforementioned incisal plane and gingival line changes, as well as anticipated adjustment issues, were written down, and the patient signed the form to indicate acceptance.
Clinical Protocol
First, a dental prophylaxis and oral hygiene instruction appointment was scheduled. After this was completed, an appointment for periodontal crown-lengthening surgery was scheduled. At that appointment, the patient was monitored and sedated. At the same appointment, prior to crown lengthening, the old crowns on the central incisors were removed, those teeth were reprepared, and provisional bis-acryl crowns (Luxatemp® [DMG America; Englewood, N.J.]) were fabricated. Endodontic therapy had been performed on the left central incisor many years ago, and the tooth was dark (Fig. 5). A “walking bleach” mixture of 30% hydrogen peroxide and sodium perborate tetrahydrate was placed inside the cleaned out pulp chamber and sealed with IRM® Intermediate Restorative Material (DENTSPLY Caulk; Milford, Del.).
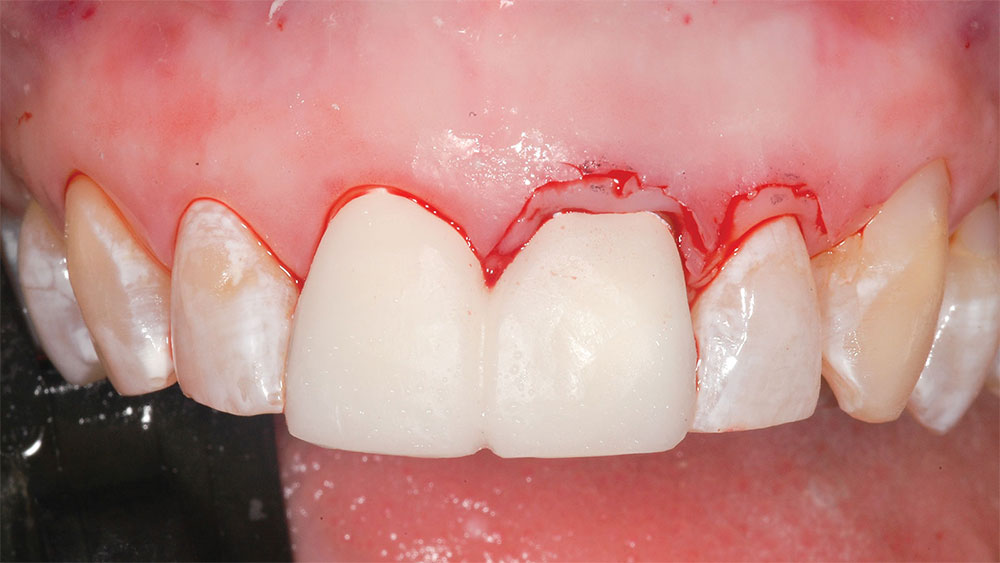
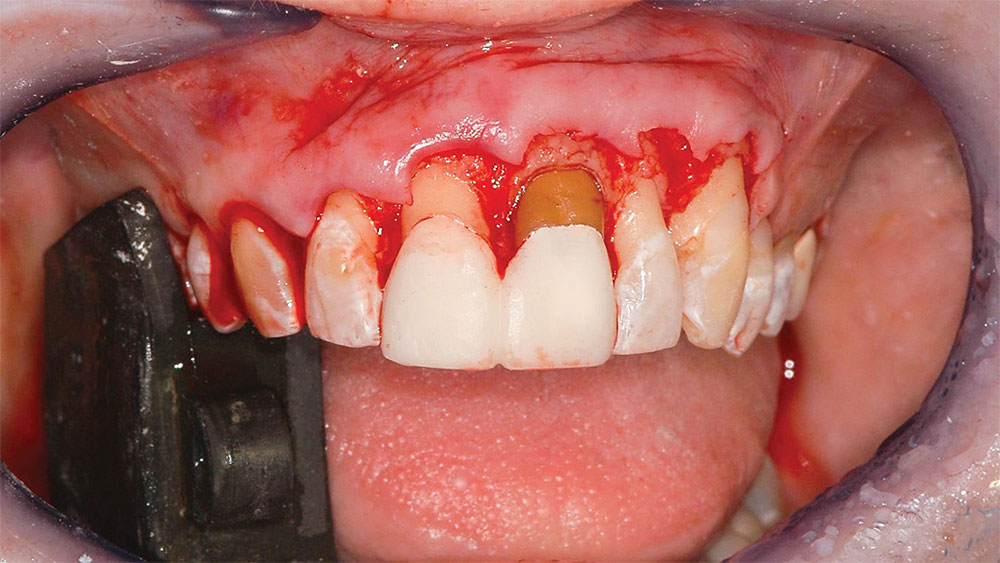
Periodontal crown-lengthening surgery was then performed. Lip retractors (Spandex® [Hager & Werken GmbH & Co. KG; Duisburg, Germany]) were placed, and the patient’s face was viewed as she sat in an upright position to determine the exact desired gingival line alignment. That line was marked with a sharp-tipped permanent marker (Fig. 6). Local anesthesia was administered (4% Citanest® Plain followed by lidocaine hydrochloride 2% and 1/100,000 epinephrine injection [DENTSPLY International; York, Pa.]), and a beveled incision was made with a size 15 Bard-Parker® blade (Aspen Surgical Products, Inc.; Caledonia, Mich.) at the newly marked gingival line position from the mesial of the right central incisor to the mesial of the left first bicuspid (Fig. 7). This incision is the improved gingival line position and, as previously described, should be approximately parallel to the lower lip and interpupillary line. Next, an incision was made in the gingival sulcus around each tooth from the mesial of the right central incisor to the mesial of the left first bicuspid. This incision extended interproximally to include the facial half of the papillae. The palatal half of the papillae remained in place (Dr. Pat Allen, Dallas, Texas, clinical observation). The gingival strip between the two incisions was removed with a periosteal elevator and rongeurs.
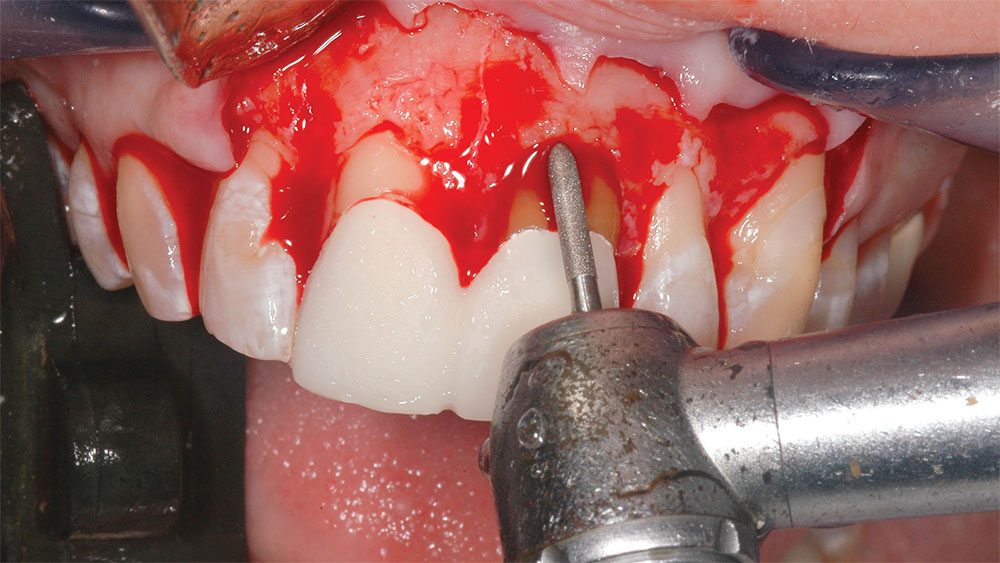
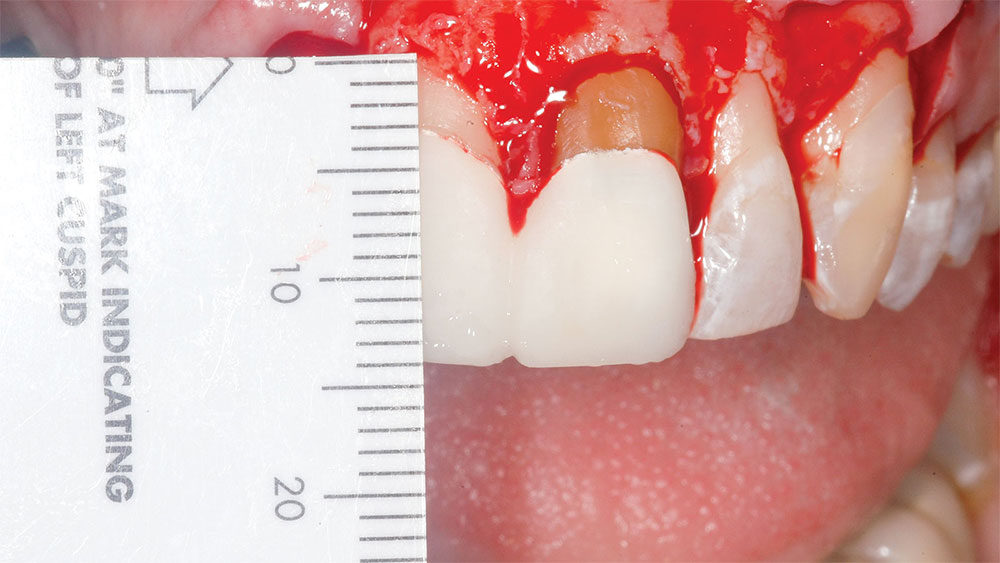
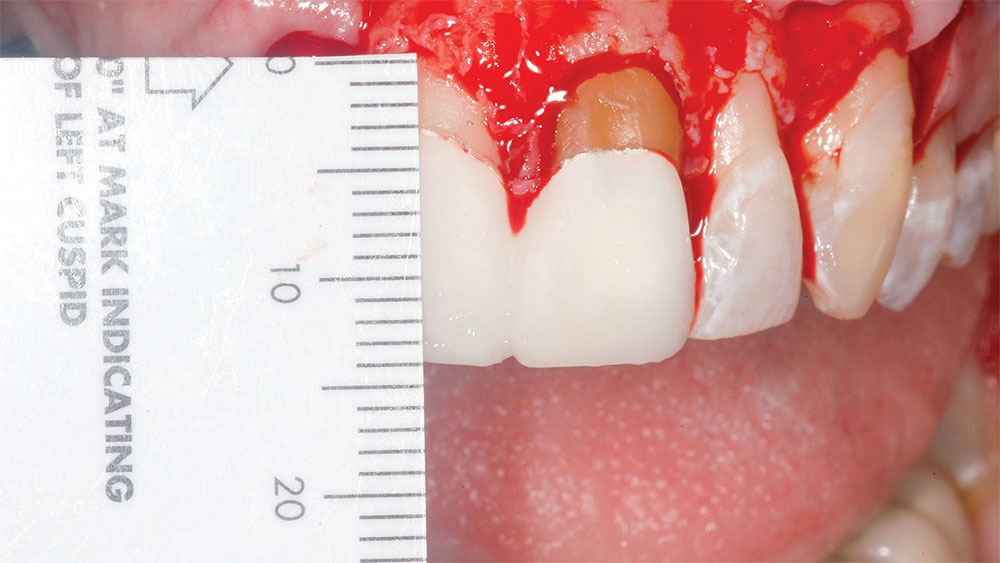
Measurements were made and recorded from the incisal edges of the teeth involved to the newly established gingival line (Fig. 8). The average central incisor is 10.5 mm in length from the gingival line to the incisal edge,4 so the supragingival central incisor tooth display following surgery should normally be less than 12 mm. The gingiva was then elevated with a periosteal elevator, and the alveolar crest was recontoured with a fine football diamond bur (No. 379) and No. 4 round diamond bur (No. 8801-023 [Brasseler USA; Savannah, Ga.]) on a high-speed handpiece with high water spray using a very light touch (Fig. 9). Various periodontal scalers and curettes were used to perfect the alveolar crest position and cleanly remove 0.5–1.5 mm of bone from the facial surfaces of the involved teeth. For the newly established gingival line to be stable, the newly established alveolar crest line should be 3 mm from the newly established gingival line (Figs. 10–12).8 For example, if the newly established gingival line measures 11 mm from the incisal edge of a tooth, the newly established alveolar crest should measure 14 mm from that incisal edge (compare Figure 13 [clinical crown length following periodontal crown-lengthening surgery and provisionalization] with Figure 8 [distance from incisal edge to newly established alveolar crest following osseous surgery]). If only gingivectomy is performed without osseous removal and recontouring to establish a 3 mm distance between the alveolar crest and gingival line, the gingiva will regrow coronally to establish its own appropriate biologic width.8,9
Interrupted 5-0 polypropylene sutures (PROLENE® [Ethicon, Inc.; Somerville, N.J.]) were placed through each papilla with a small, reverse cutting needle to secure the periodontal flap into the proper position. The new gingival line was parallel to the lower lip and interpupillary line (Fig. 12). The nonresorbable sutures were removed in seven days. If left in place longer, the tissue would overgrow the suture, making removal difficult and painful, sometimes even requiring local anesthesia. The ultrathin 5-0 PROLENE suture and small reverse cutting needle are recommended because only minimal damage is done to the papillae. The patient was instructed to rinse gently with a solution of chlorhexidine gluconate (PerioGard® [Colgate Oral Pharmaceuticals; New York, N.Y.]) for one minute each morning and night for three weeks. During that time she flossed gently but did not brush. After two weeks, the gingival line area could be gently wiped in a semicircular and incisal direction with a cotton ball that is held by tweezers and dipped in the chlorhexidine gluconate liquid.
A satisfactory result was achieved with the previously described tooth bleaching procedure for the left central incisor, and the bleaching mixture was removed from the tooth two days after placement. A very opaque, white-filled resin was used to fill the pulp chamber (Filtek™ Supreme [3M™ ESPE™; St. Paul, Minn.]).
The periodontal crown-lengthening surgery was allowed to heal for three months, establishing an ideal gingival line position. Impressions of the maxillary teeth and a face-bow record were taken for stone model mounting on a semi-adjustable articulator and a wax-up of the stone teeth to ideal alignment. The wax-up model would be used later to fabricate provisional restorations. An all-morning sedation appointment was made to prepare the maxillary anterior teeth for crowns and porcelain veneers.
Lip retractors were placed, and an ideal incisal plane position was determined with the patient sitting in an upright position (Fig. 14). The provisional crowns were removed from the central incisors. The incisal edges of the incisors and cuspids were prepared using a diamond bur (No. 909-050 [Brasseler USA]) with the patient again sitting in the upright position (Fig. 15). Minimal incisal adjustment was needed on the patient’s right incisors and cuspid due to the preexisting nonparallel incisal plane. Actually, only parallel alignment of the incisal edges of those teeth was performed. Following are objectives of the final restorative result:
- The central incisors should be the longest teeth, incisally, in the incisal plane.
- The central incisors should normally be 10–12 mm in length.
- The incisal plane, from cuspid to cuspid, should form a soft U or quarter-moon shape and be parallel to the lower lip, the interpupillary line and the gingival line.
- The incisal plane and the gingival line should blend smoothly into the occlusal plane and the posterior gingival line.
- The midline should be perpendicular to the interpupillary line. The interpupillary line represents a flat plane, parallel to the floor.
- The horizontal location of the midline in relation to the vertical center of the face was not a major consideration, because that is a skeletal teeth position issue.10
The central incisors were reprepared for full crowns, and the lateral incisors, cuspids, and first and second bicuspids were prepared for porcelain veneers. Retraction cord was placed circumferentially around the central incisors (full crowns) and in the facial sulcus only (Z-Twist, size 00 [Gingi-Pak; Camarillo, Calif.]) of the veneer-prepared teeth (Fig. 16). A polyether impression (Impregum™ Penta™ Soft [3M ESPE]) with custom trays was taken. A face-bow and a vinyl polysiloxane (VPS) (Blu-Mousse® Super-Fast [Parkell, Inc., Edgewood, N.Y.]) occlusal bite registration record (between the central incisors only) were taken for mounting the models of the prepared teeth on a semi-adjustable articulator for laboratory fabrication of restorations.
Bis-acryl provisional restorations (Luxatemp) were fabricated from a custom VPS matrix (Express™ STD Putty [3M ESPE]) made from the pre-op, waxed-up model. High-quality, full-face photographs were taken of the prepared teeth with lip retractors in place and the patient sitting in the upright position, face perpendicular to the camera lens (Fig. 16). These photographs were sent to the laboratory technician for face-bow mounting verification. Close-up photos were taken of the prepared teeth with shade tabs so the laboratory technician could view the hue, chroma and value of the teeth. This is especially important if a dark natural tooth shade must be blocked out in the restorations.
The provisional restorations were seated with provisional cement (Fynal® [DENTSPLY Caulk]) for the central incisor crowns and unfilled resin (Scotchbond™ [3M ESPE]) for the provisional veneers. With the patient sitting upright, face parallel to the camera lens, photographs were taken of the full face with lips retracted, full-face smile, incisal plane with lips in repose, and a close-up of the smile. These photos, along with study models of the provisional restorations, were sent to the laboratory as a guide for the ideal incisal plane and teeth alignment. The laboratory could fabricate a VPS incisal matrix from the stone models of the provisional restorations or mount the models of the provisionals on a semi-adjustable articulator with the face-bow and create a custom incisal guide table. The VPS incisal matrix or the incisal guide table could then be used to closely replicate the incisal plane of the provisional restorations in the final porcelain restorations. The patient adapted quickly to the remodeled incisal plane and was immediately speaking clearly and normally. She was checked in the office one week following teeth preparation and provisional restoration placement.
Porcelain-to-zirconium oxide (layered) crowns (Lava™ [3M ESPE]) were fabricated and placed on the maxillary central incisors. Porcelain veneers were placed on the lateral incisors, cuspids, and first and second bicuspids. The zirconium oxide copings were impregnated with silica in the laboratory with a Rocatec™ (3M ESPE) device, and then these were cemented clinically with a self-etching, self-adhesive resin cement (RelyX™ Unicem [3M ESPE]). The porcelain veneers were etched with 8% hydrofluoric acid in the laboratory and seated using a light-cured resin cement (RelyX Veneer Cement [3M ESPE]) (Fig. 17).
According to the treatment plan, the lower teeth were bleached, the chipped edges of the lower anterior teeth were bonded (Filtek Supreme), and a maxillary hard acrylic, flat plane centric relation occlusal nightguard was fabricated. After photos (Figs. 18–20) include “lips in repose.” As previously discussed, excellent occlusion, function and esthetics can be achieved even if the incisal plane of the mandibular teeth does not parallel the incisal plane of the maxillary teeth (Fig. 17).
IN SUMMARY
A beautiful smile is more than just white teeth. This article has discussed the importance of approximate parallelism of the interpupillary line, incisal plane of the maxillary teeth, and lower lip-line in dental esthetics. Methods of changing the maxillary gingival line and incisal plane, when they are not parallel with the lower lip and interpupillary line (which represent a flat plane or the floor), have been presented. As in all complex restorative cases, including the case presented in this article, a comprehensive examination and consultation is an essential step in treatment planning and presentation. Patients may further understand their condition through the use of images of similarly restored cases, allowing them to confidently partner with the dentist during all phases of their treatment plan.
As in all complex restorative cases, including the case presented in this article, a comprehensive examination and consultation is an essential step in treatment planning and presentation.
References
- ^Hulsey CM. An esthetic evaluation of lip-teeth relationships present in the smile. Am J Orthod. 1970 Feb;57(2):132-44.
- ^Davis NC. Smile design. Dent Clin North Am. 2007 Apr;51(2):299-318, vii.
- ^Passia N, Blatz M, Strub JR. Is the smile line a valid parameter for esthetic evaluation? A systematic literature review. Eur J Esthet Dent. 2011 Autumn;6(3):314-27.
- ^Bhuvaneswaran M. Principles of smile design. J Conserv Dent. 2010 Oct;13(4):225-32.
- ^Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996 Jun;11:18-28.
- ^Cutbirth ST. Importance of lip type classification: maxillary central incisor length determination versus lip phenotype. Dent Today. 2014;33:126-30.
- ^Eagly AH, Makhijani MG, Ashmore RD, et al. What is beautiful is good, but…: A meta-analytic review of research on the physical attractiveness stereotype. Psychol Bull. 1991;110:109-28.
- ^Teaching sounds in isolation to children with speech delays [internet]. [place unknown]: Speech and Language Kids; [cited 20 Oct 2014]. Available from: http://speechandlanguagekids.com/how-to-teach-a-new-sound.
- ^Yeh S, Andreana S. Crown lengthening: basic principles, indications, techniques and clinical case reports. N Y State Dent J. 2004 Nov;70(8):30-6.
- ^Camargo PM, Melnick PR, Camargo LM. Clinical crown lengthening in the esthetic zone. J Calif Dent Assoc. 2007 Jul;35(7):487-98.
Disclosure: Dr. Cutbirth is an occasional lecturer for 3M ESPE but has received no compensation for writing this article.