Full-Arch Implant Restorations: Improving Patients’ Lives Over the Short and Long Term

Note: The Hahn Tapered Implant System is now known as the Glidewell HT Implant System
Doctors who perform implant therapy in full-arch indications not only restore form and function, but also improve the quality of life for the edentulous patient. Whether requesting treatment for ill-fitting, poorly functioning dentures or a permanent solution for terminal dentition, these patients commonly suffer from discomfort, diminished chewing capability, and low self-esteem as a result of their condition. By providing a fixed implant prosthesis, we can positively impact these patients’ lives with a restoration that mimics the appearance and function of natural teeth while minimizing bone loss.1,2
Immediate provisionalization after implant placement is particularly beneficial to the fully edentulous patient and instantly addresses many of the problems associated with edentulism or untreatable dentition. Receiving fixed teeth on the day of surgery is appealing to patients because it allows for the immediate restoration of function, avoids challenges related to removable temporary dentures, reduces the number of surgical appointments, and establishes a template for the eventual full-arch restoration.
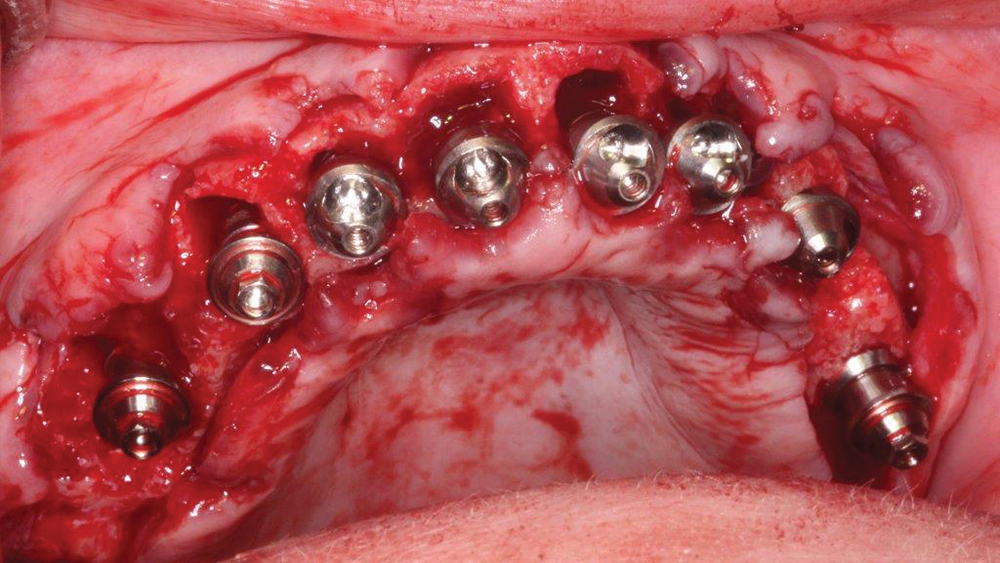
Because this approach is indicated only in the presence of high initial implant stability, many practitioners have refined their techniques and surgical armamentarium to increase the likelihood that immediate loading can be safely performed. This includes the use of implants with an aggressive thread design to maximize primary stability and the odds that an immediate provisional appliance can be delivered.
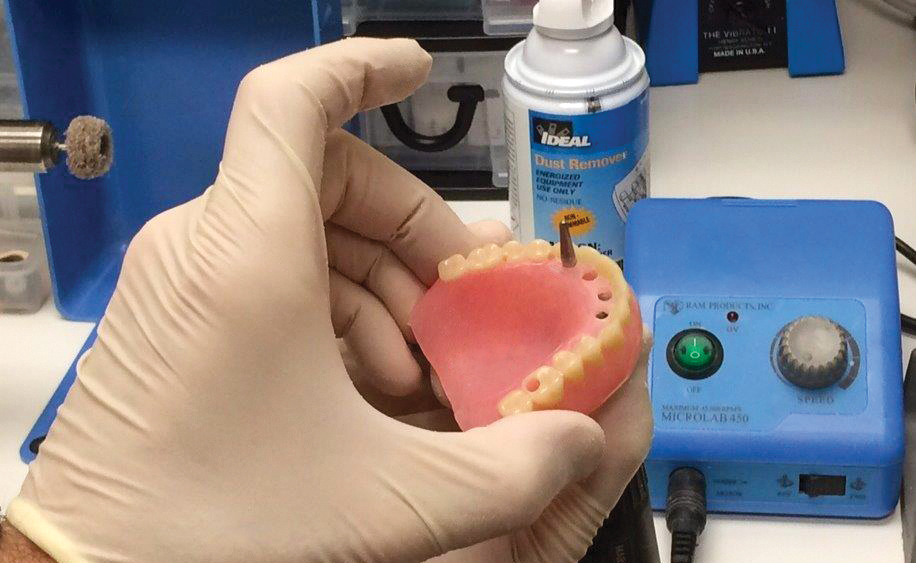
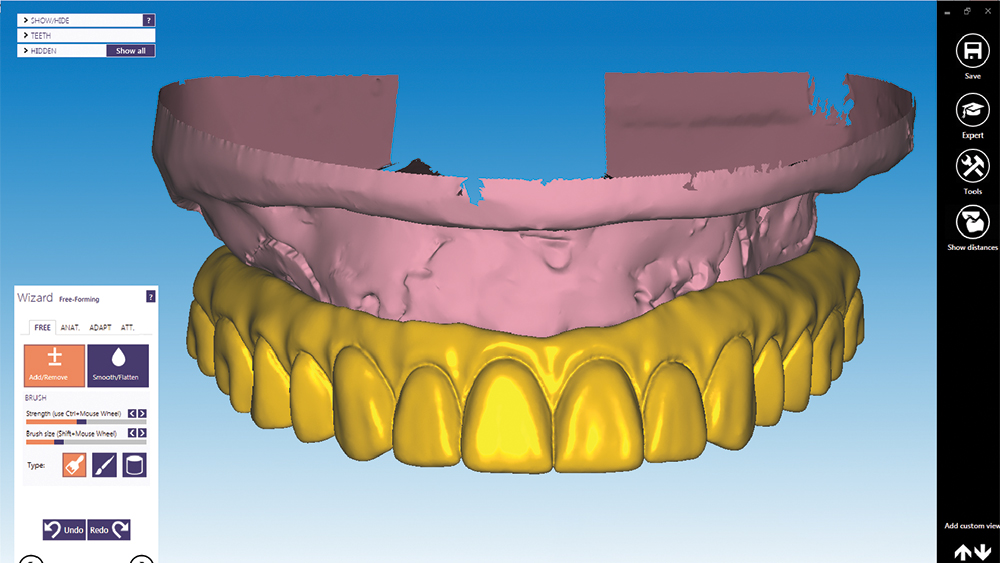
During the restorative phase of treatment, dentists are taking advantage of the CAD/CAM process to fine-tune prosthetic designs with a remarkable degree of precision, providing the patient with a confident smile. Clinicans can visualize the ideal prosthetic outcome through dental CAD software, confirm that design in physical form via the PMMA provisional implant prosthesis, and make any final adjustments before the final restoration is produced in durable, esthetic BruxZir® Solid Zirconia.
CASE REPORT
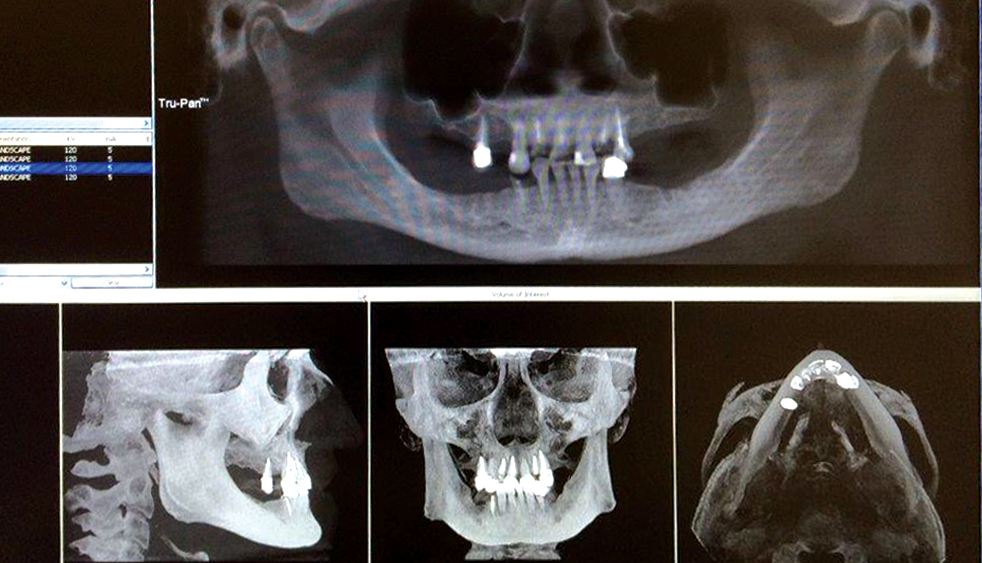
A patient sought treatment for advanced caries and periodontal disease in the maxillary arch, which had become painful and compromised her oral function. Although her remaining mandibular teeth also required replacement, she couldn’t afford to restore both arches at once and, like most patients, she placed a higher priority on her maxillary arch because of her esthetic needs. Following a discussion of treatment options, the patient requested a fixed restoration and was opposed to a removable appliance. At the surgical appointment, her maxillary teeth were extracted and Hahn™ Tapered Implants (Glidewell Direct; Irvine, Calif.) were placed. Sufficient primary stability was established for an immediate provisional appliance, which satisfied the patient’s request to leave the surgical appointment with a fixed restoration in place. After five months of healing and confirmation of the prosthetic design with a PMMA provisional, function, esthetics and quality of life were restored with a BruxZir Full-Arch Implant Prosthesis.
Sufficient primary stability was established for an immediate provisional appliance, which satisfied the patient’s request to leave the surgical appointment with a fixed restoration in place.
CONCLUSION
The combination of tried-and-true surgical protocols and modern implant prosthetics has simplified the restoration of function for patients with debilitating dental conditions, and has improved what we can accomplish esthetically. With the aid of proper implant selection and positioning, high primary stability can be established, allowing for the delivery of an immediate provisional that affords instant relief for the patient and gives the clinician a head start on determining the optimal prosthetic design for the patient. This provides the opportunity to transform the oral health — and quality of life — of the fully edentulous patient on the day of surgery, while setting the stage for a predictable, long-lasting restoration.
References
- ^Jacobs R, Schotte A, van Steenberghe D, Quirynen M, Naert I. Posterior jaw bone resorption in osseointegrated implant-supported overdentures. Clin Oral Implants Res. 1992 Jun;3(2):63-70.
- ^Preciado A, Del Río J, Lynch CD, Castillo-Oyagüe R. Impact of various screwed implant prostheses on oral health-related quality of life as measured with the QoLIP-10 and OHIP-14 scales: a cross-sectional study. J Dent. 2013 Dec;41(12):1196-207.
- ^Covani U, Cornelini R, Calvo-Guirado JL, Tonelli P, Barone A. Bone remodeling around implants placed in fresh extraction sockets. Int J Periodontics Restorative Dent. 2010 Dec;30(6):601-7.
- ^Tealdo T, Menini M, Bevilacqua M, Pera F, Pesce P, Signori A, Pera P. Immediate versus delayed loading of dental implants in edentulous patients’ maxillae: a 6-year prospective study. Int J Prosthodont. 2014 May-Jun;27(3):207-14.