Photo Essay with Dr. Daniel Melker on the Perio-Restorative Connection
Note from the Editor
I chose to include another photo essay from periodontist Dr. Daniel Melker in this issue because I have a huge amount of respect for his clinical skills and his excellent clinical photographs. About eight years ago, I begged and pleaded with Dan to let me come spend a day or two at his office to watch how he works. I finally wore him down, and he allowed me to spend some time observing him in surgery, and then going through case slides, many of which were 15 to 20 years post-op.
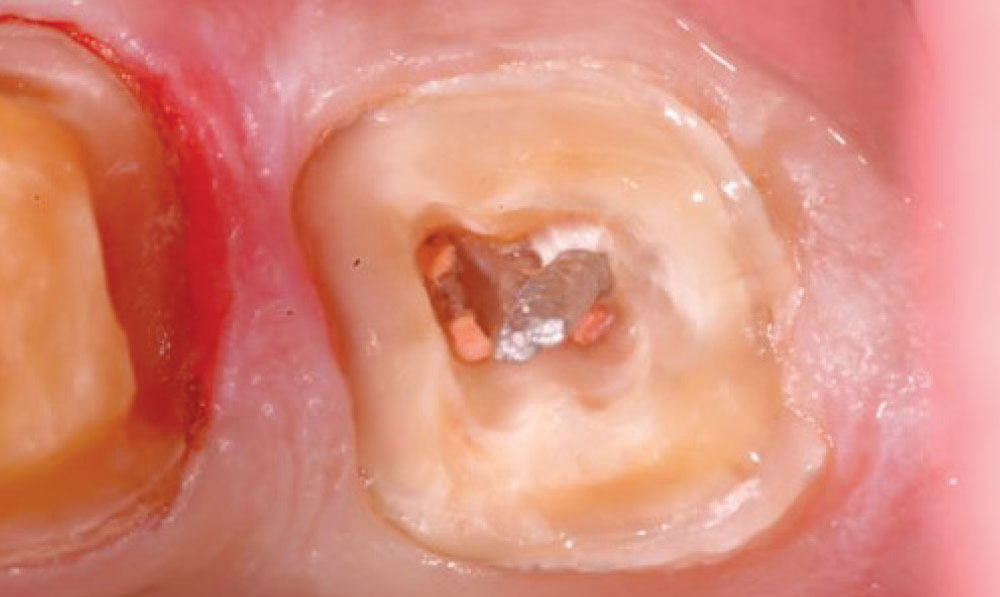
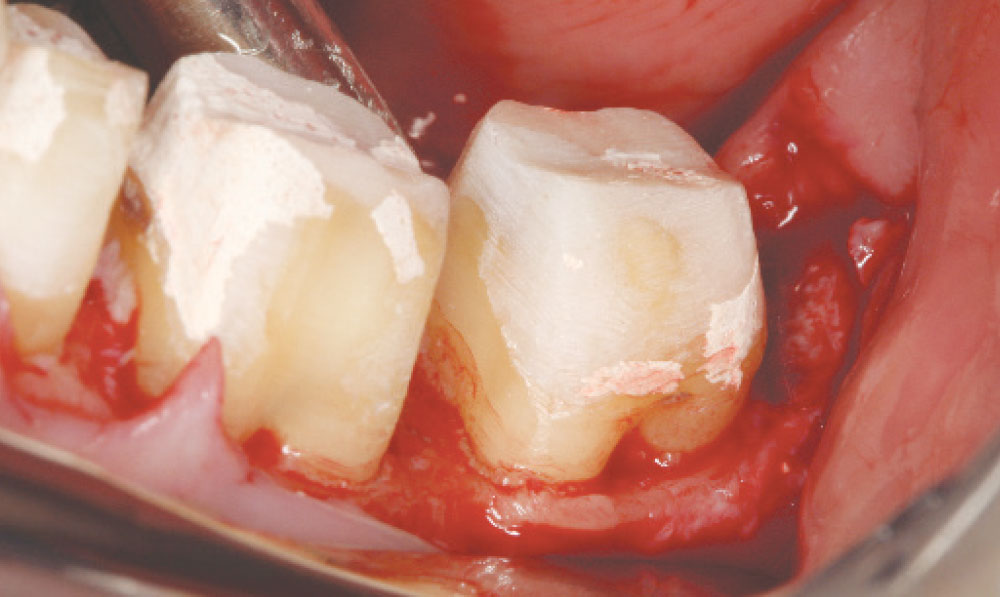
Dan is Dr. Bill Strupp’s periodontist — the one partially responsible for all the gorgeous tissue you’ve seen in Bill’s articles in Chairside® or at his lectures. Dan happened to be working on one of Bill’s patients the first day I spent at his office, and when he took off the temporaries, I saw those same Strupp preps I have seen so many times before. Not that there was ever any question, but it was clear Bill practices what he preaches, and the same goes for Dan.
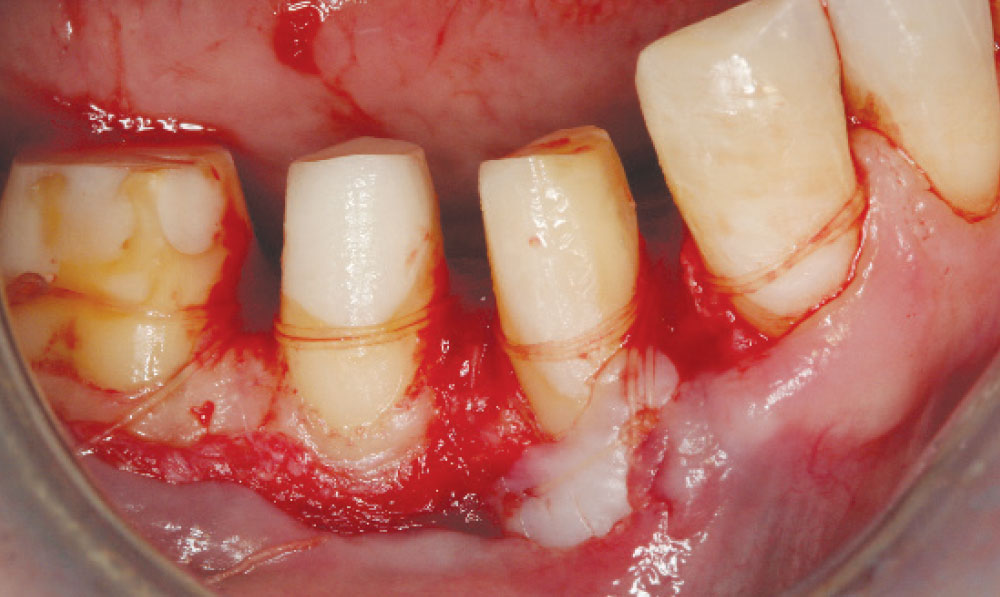
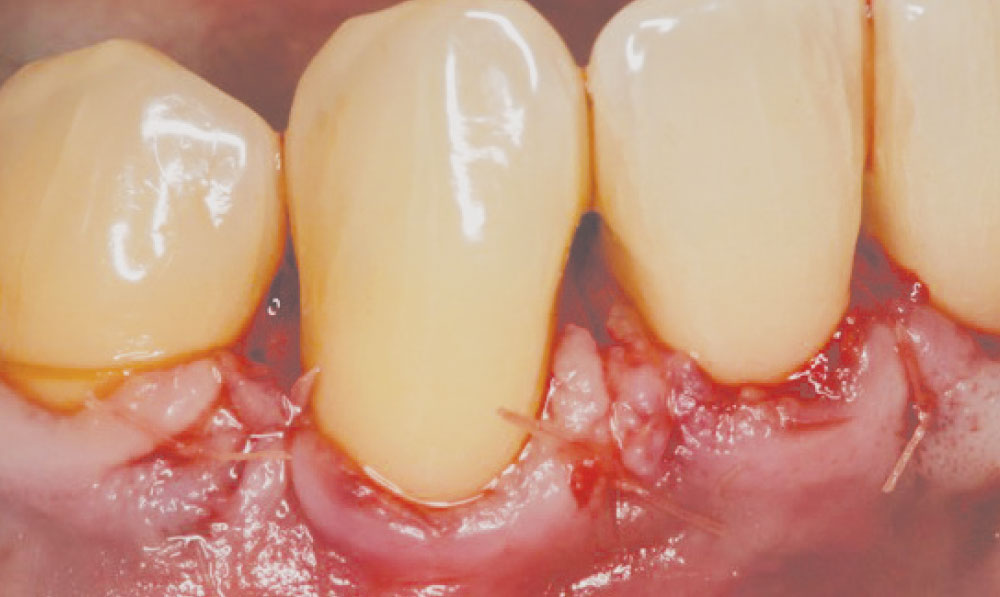
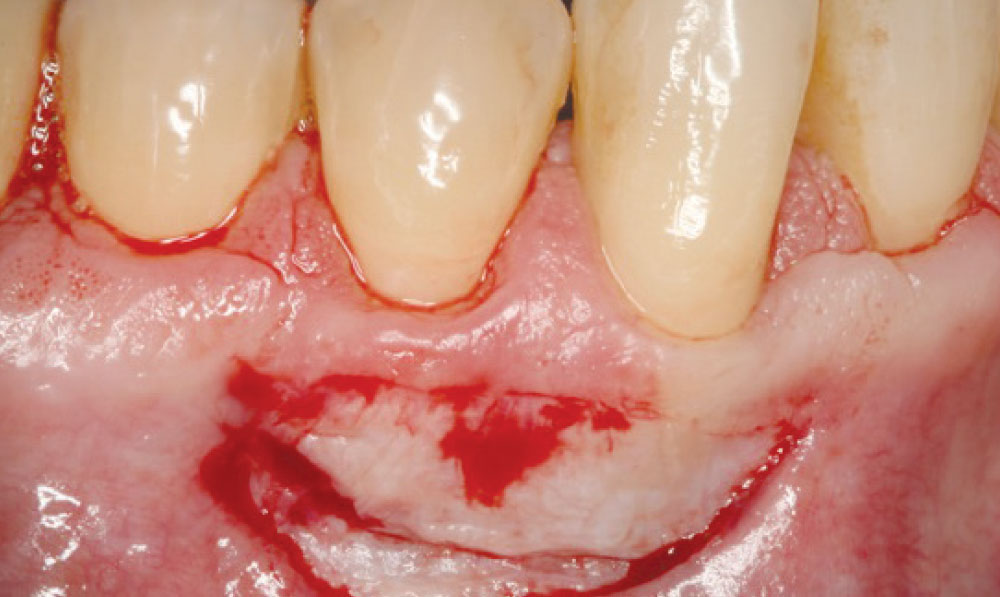
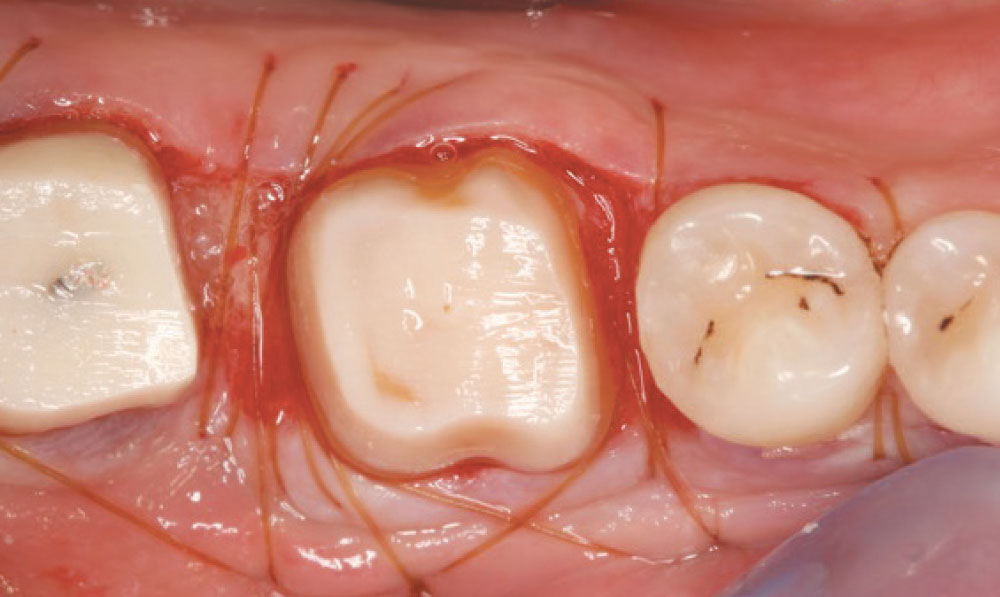
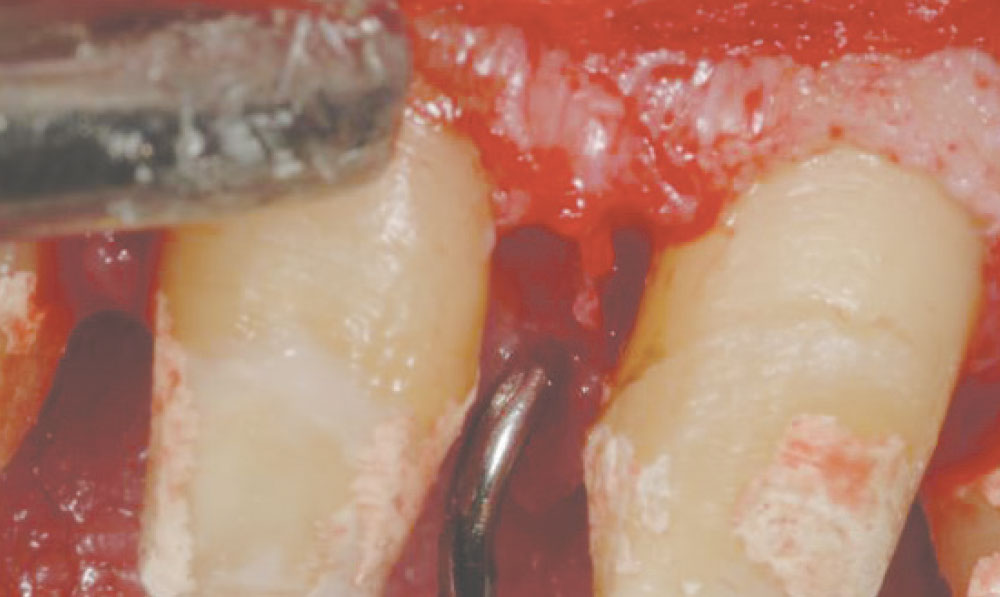
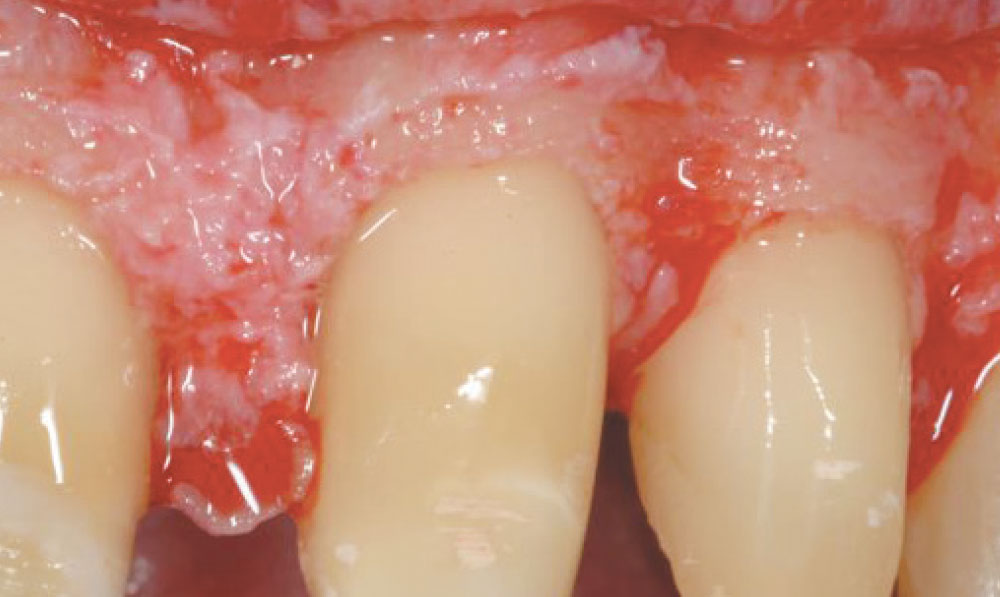
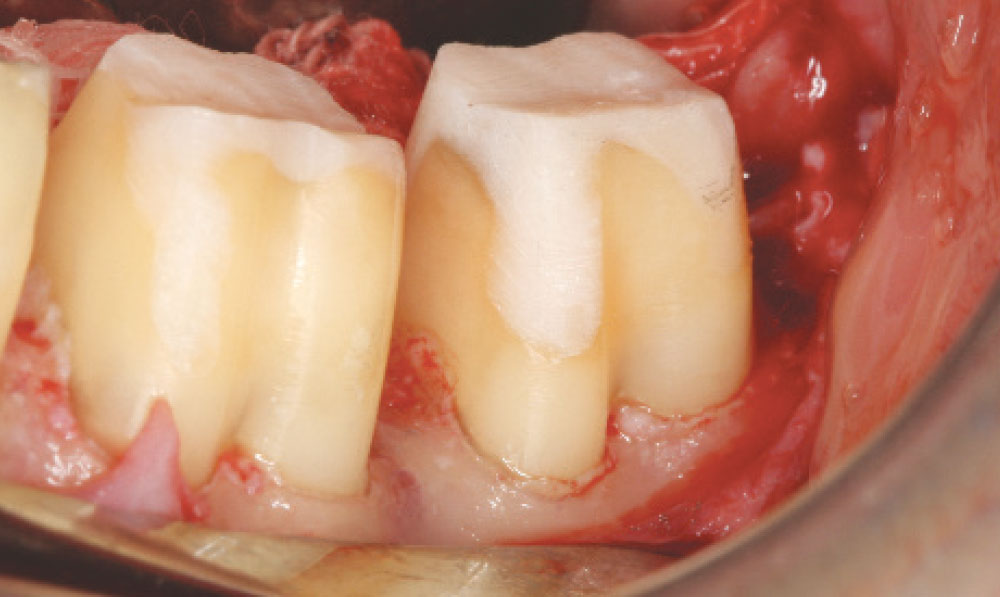
While I was there, I got to see a couple root reshaping cases (Dan prefers biologic shaping), which at the time boggled my mind. I didn’t know of anyone else doing this at the time, and I still don’t see anyone else showing these types of cases, other than Bill and Dan. Never before had I seen anyone routinely remove the CEJ (cementoenamel junction) to improve the long-term stability of the case. I also got to see some grafting and some hard tissue crown lengthening without a gingivectomy.
You may not want to attempt surgery quite like this yourself, but I think it’s important to know that it exists, because I guarantee you have many patients who would benefit from it. Make your periodontist take you out to lunch, bring this issue of Chairside with you, and show him what you would like him to try on a couple of cases. Resist the urge to take off an old, ugly PFM with a biologic width invasion and just slap on a new IPS e.max® (Ivoclar Vivadent; Amherst, N.Y.) crown because you know it will look better. Do the right thing and let your periodontist correct the condition, and then move forward — or do it yourself, if you feel comfortable. To push on with restorative dentistry while ignoring the tissue and supporting structures is an incomplete view of what we, as dentists, are here to do.
I hope that, like me, you will look at the cases that follow and get inspired. I think seeing them will encourage you not to just turn a blind eye the next time you come across one of these clinical situations in your own practice.
Case 1
Case 2
Case 3
Case 4
Case 5
Case 6
Case 7
Case 8
Case 9
Dr. Daniel Melker is in private practice in Clearwater, Florida, and lectures nationwide. Contact him at 727-725-0100.
References
- Satheesh K, MacNeill SR, Rapley JW, Cobb CM. The CEJ: a biofilm and calculus trap. Compend Contin Educ Dent. 2011 Mar;32(2):30,32-7.