Is It Time to Do Routine Adult Pulpotomies?
Introduction
Two patients walked into two dental offices with the same problem. They each had a molar with deep caries, a pulp exposure, pain and fear. One patient chose traditional endodontic treatment and, after making several 40-minute visits to his dentist, paid $1,200 and left “cured.” He later got a $1,000 crown to restore the tooth. The second patient had a one-visit pulpotomy and an alloy filling, which took 25 minutes. He paid $250 and left “cured.” Who got the better deal? For whom was the deal better, the dentist or the patient?
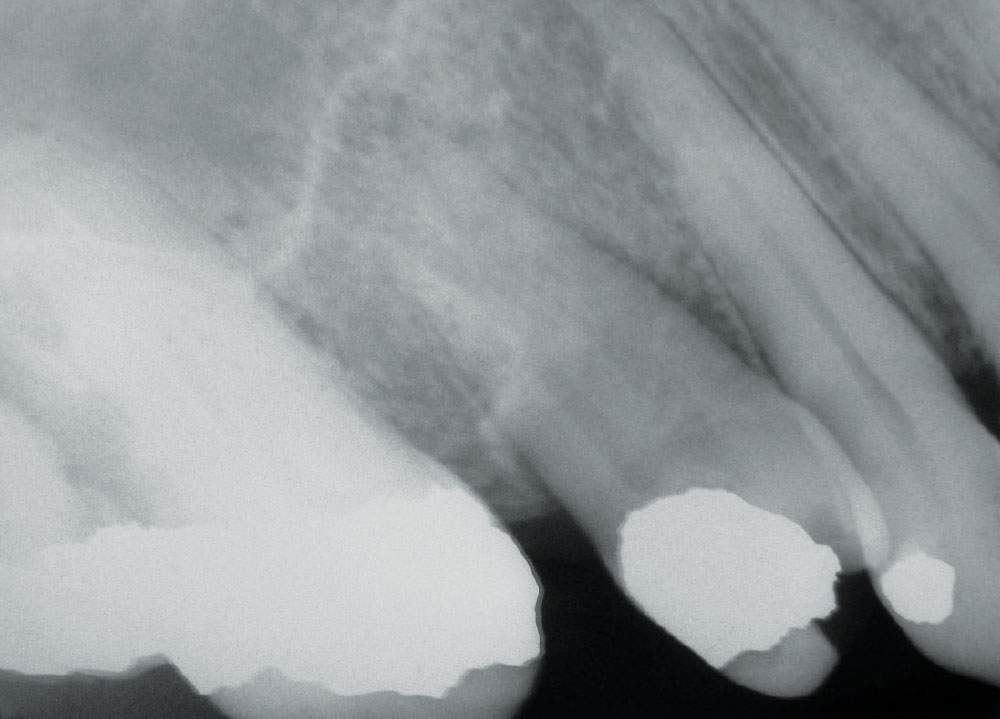
As our nation’s prosperity continues to decline during this recession, and business, insurance and government benefits rapidly erode, fewer patients can afford traditional root canal therapy, yet the need for endodontic treatment is continually greater. The more people who delay routine dentistry (exams, prophylaxis, restorations) because of finances, time and other “excuses,” the more exposed pulps will eventually come into our offices. We are seeing this now. Fewer and fewer patients can afford or want root canal treatment. Endo is becoming the treatment of the rich and well-connected (insured), primarily because of the high cost of therapy (Fig. 1).
So great is the cost of endo that extraction and implants have become a viable, though high-priced, alternative. Average U.S. prices for a molar endo range from $900 to $1,400. But for most patients, even those with a paltry $1,000 maximum on their dental insurance policies, extraction is generally the only practical and affordable treatment offered. They cannot afford the price of endo and often choose low-cost extractions as their only alternative. This unfortunate state of affairs will continue — if not grow — as our economy languishes and widespread un- and underemployment continues. And when “prosperity” does come back, in a year or three from now, it will never be (economically) the way it once was. Insurance and other employment benefits will be lower. Government-sponsored dental plans (e.g., Medicaid) will opt for the least expensive treatment. Endodontics, as we know it, will have to change.
The average patient needs a low-cost, quick and comfortable alternative to traditional endodontics, besides extraction. They do not have the money, patience or resources to afford traditional endo in the way we have done it in the recent past. Many do not have the money to get implants, fixed bridges and other expensive replacement dental treatments, yet they want to save their teeth.
Endodontics is not the only issue, however. Usually the tooth, after endo treatment, will require an expensive crown and recommended post, which further stresses limited economies.
Wouldn’t it be nice to offer our patients a cheap, quick and comfortable “magic bullet”; a medicine and filling placed in the infected or nonvital tooth which will render it asymptomatic, stable and serviceable for long periods of time? That is what a pulpotomy can be, and we can offer it without any special kits, training or expensive equipment.
We dentists are morally obligated to help the growing mass of financially strapped patients, and the only technique that will meet this need, short of mutilating extractions and free endo, is the adult tooth pulpotomy.
Pulpotomy
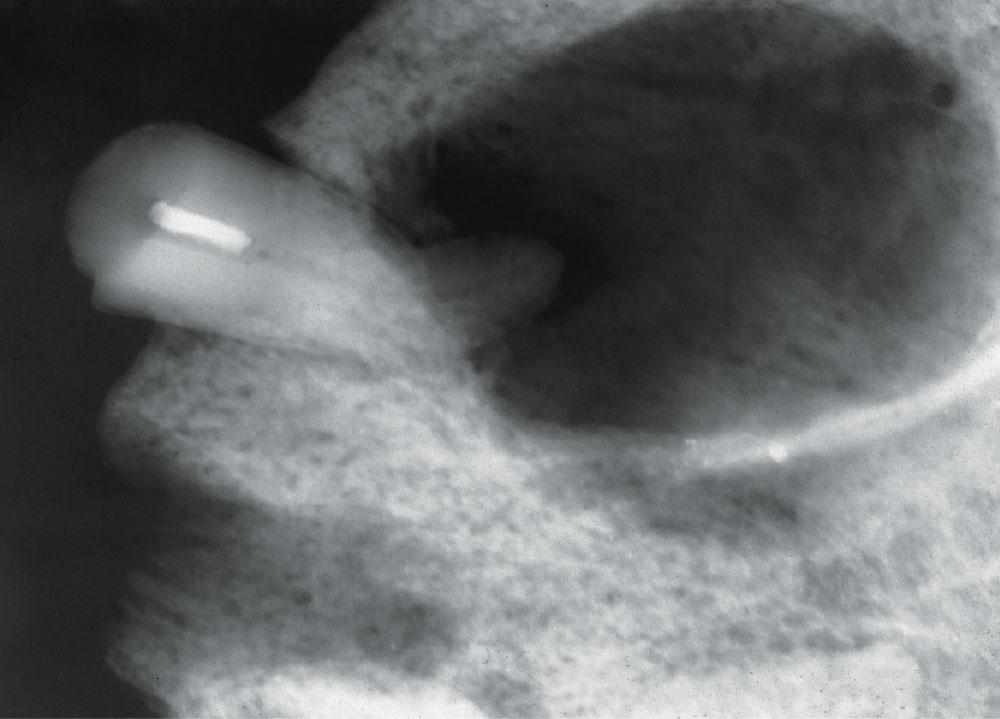
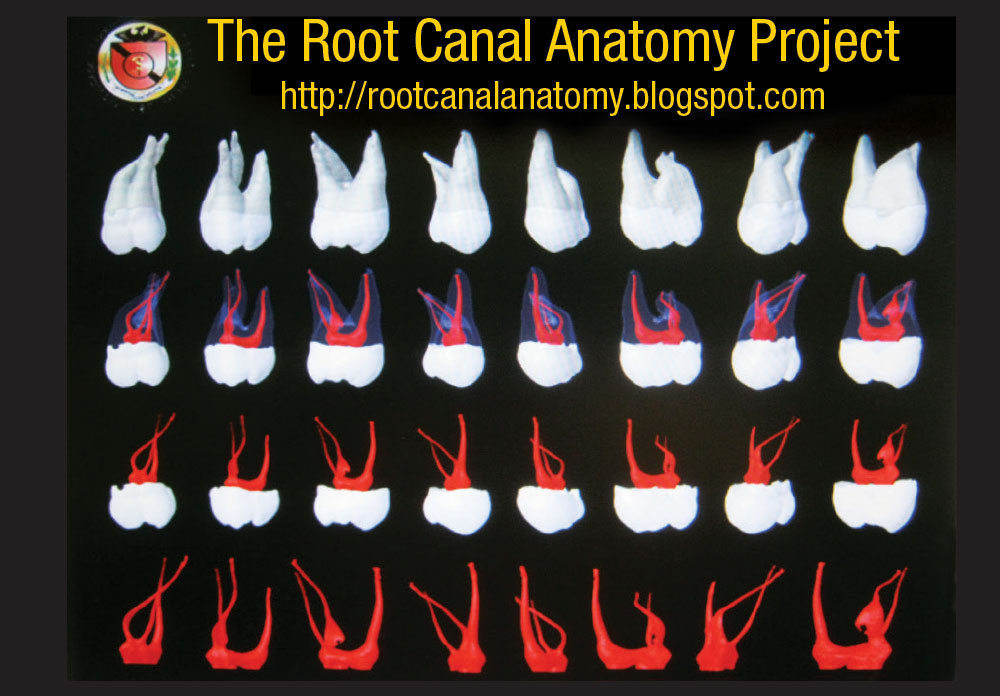
A pulpotomy is the removal of the dental pulp and the placement of medication that will halt infection and preserve the tooth.1-3 There are numerous types of pulpotomies, such as the pulpectomy (removal of the pulp), partial pulpectomy, shallow pulpotomy (and its “deep” analogue) and radicular pulpotomy. All of these remove the pulp tissue, more or less. The emptied pulp chamber is filled with a germicidal medication, which destroys infective organisms and mummifies (fixes) any remaining tissue that could later contribute to a septic condition around the tooth.1-6 Formocresol (FC) has been very popular with dentists for more than 100 years. The original Buckley’s formula for FC consists of 19% formaldehyde and 35% cresote, plus fillers.3-6 Glutaraldehyde, calcium hydroxide, zinc oxideeugenol (ZOE), mineral trioxide, ZOE with 6% paraformaldehyde (N2) and ferric subsulfate are some of the other medications in popular use. All of these cause cell death, mummify tissue and are theoretically mutagenic, though in the real world, no related cancer cases have ever been reported.1,7 They render the infected tooth aseptic, and thus allow the tooth to remain in the mouth comfortably for years (Fig. 2).
The typical pulpotomy procedure is to open the tooth’s pulp chamber, remove the decay and as much of the pulp tissue as practical, place the medication (e.g., FC) in the form of a cotton pellet or cement paste, and then close the tooth with a restoration (e.g., alloy, composite, crown).1-4 It is simple, quick and inexpensive. This is done in a single visit or several visits, depending on the initial infection and the response of the tooth. Since the advent of traditional endodontia, this technique has been usually reserved for deciduous teeth.3
The average patient needs a low-cost, quick and comfortable alternative to traditional endodontics, besides extraction. They do not have the money, patience or resources to afford traditional endo.
Adult pulpotomies are not as popular with dentists today as they were 100 years ago. Historically, traditional endodontia has been reported to be a more reliable treatment than pulpotomy techniques, based on the rate of saved teeth and the longevity of their preservation.8-26 However, new research is changing this view.5,6,12-16
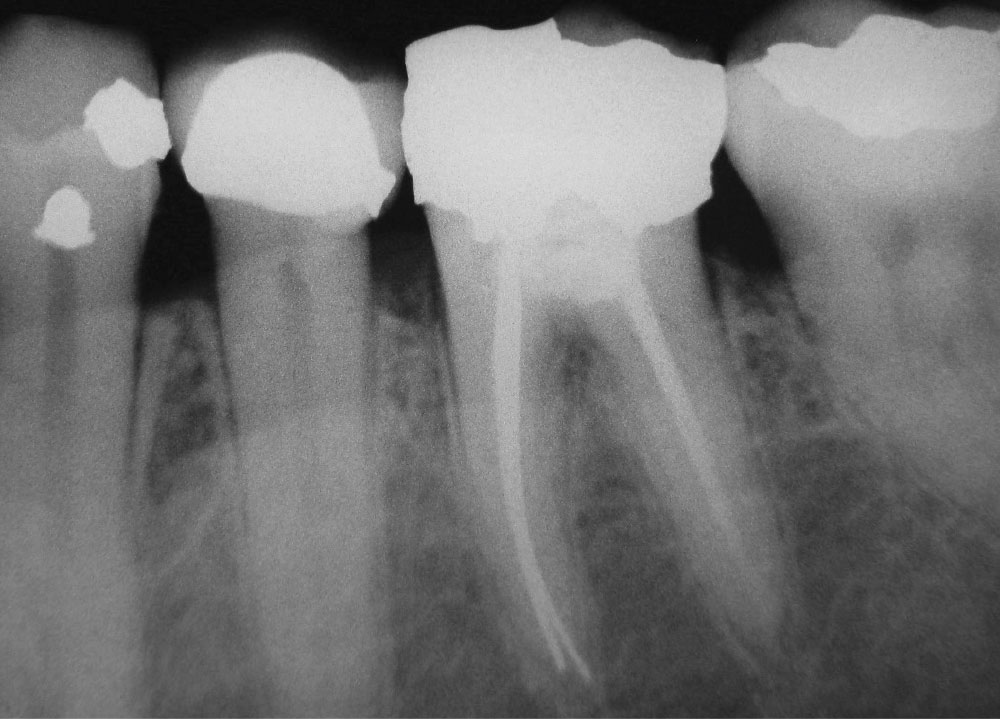
The pulpotomy, as a therapeutic dental treatment, has a long history. It has been used for thousands of years. Zias reports a pulpotomy-endodontic treatment found in the tooth of a Middle Eastern, Hellenic-Nabatian soldier of 200 B.C.27 (Fig. 3). In this ancient case, the large radiolucency around the treated tooth’s apex shows a less-than-perfect therapeutic result, though the treatment may have been started just prior to death. Dentists throughout history commonly used adult tooth pulpotomies until the 1930s, when traditional endo was developed and promoted as being a more reliable pulpal therapy.1-3,25,26 In 1964, endodontics became a recognized specialty.
Traditional Endodontics
The object of traditional endodontics is to remove pulpal tissue and seal the canals to the apex area of the root1,2,3,26 (Figs. 1, 4). This is done with an ever-increasing complex of technology: devices and techniques such as Ni-Ti files, reamers, sealers, tissue diluents, microscopes, apex electronics, ultrasonics, lasers and piezo-electric actuators.8 By my count, there are 35 rotating file systems and five reciprocating instrument systems on the market at this time devoted just to cleaning canals. The progression of increasing complexity has caused the cost of doing endo to escalate to economically prohibitive levels for many people. The 4,000 endodontic specialists (with 253 new graduates per year) are not numerous enough to perform the estimated 24,000,000 root canal treatments needed each year.8,18,19 This leaves most endodontics to be done by the general practitioner.
Dentists throughout history commonly used adult tooth pulpotomies until the 1930s, when traditional endo was developed and promoted as being a more reliable pulpal therapy.
Traditional endo has many drawbacks. Not only does it take much time, effort, investment (equipment cost) and skill, but to the long-suffering patient, it is often uncomfortable, involving anesthesia, rubber dams, long periods with the mouth open, retreatments, post-op sensitivity, blow-ups, blocked canals, separated files, apicoectomies, hypochlorite leaks, ledges, excessive biofilms, lateral canals, anastomoses, deltas, overfills, underfills, cracks, perforations and microsurgery (Figs. 1, 4–6). Today’s endodontic sealers and canal obturators (e.g., gutta-percha), though often tolerated, form leaky seals, seldom fill all voids in the canals and are associated with chronic apical irritation from leaking pathogens9,10 (Figs. 4–6). This is why 96% of in situ-biopsied, endodontically treated teeth often have large accumulations of lymphocytes (in response to infection) found in the apical tissues years after treatment9-11 (Fig. 5).
Even though traditional endo has its problems and hazards, it provides a relatively excellent, consistent result in saving teeth (Figs. 1, 4). This result has been far better and more consistent than what was once found with many older adult pulpotomy techniques.1-3,25,26 New research and techniques are changing this view.3,4,12-16
Success
Traditional endodontic therapy is intended to preserve the diseased tooth. Whether the treatment is traditional endo, with its completely sealed canals, or a pulpotomy with mummified pulpal tissue, the measure of success is an asymptomatic, functional and disease-free, long-lived tooth (Figs. 1, 2, 4, 7–9). Traditional endodontia defines success as the treated tooth being asymptomatic, with no periapical (radiographic) pathology, and the sealers (e.g., gutta-percha) extending to the anatomic apex of each root.3,10,11,26
As time progresses, increasingly more stringent criteria are applied to the definition of “quality endo.” Some of these criteria are questionable. Must the canal be sealed exactly to the anatomic apex (Fig. 4)? Must the periapical tissue appear perfectly “normal” around the apex as seen on the radiograph (Fig. 7)? Must the tooth last 10 to 30 years post treatment? Is it a success if it survives only eight years?
96% of in situ-biopsied, endodontically treated teeth often have large accumulations of lymphocytes found in the apical tissues years after treatment.
Pulpotomy success has similar criteria, except the canals are not completely sealed to the apex, and in some cases, asymptomatic, nonprogressive periapical abnormalities (e.g., root scars) are noted and periodically observed (Figs. 2, 7–9). Both treatment methods define the lack of tooth-related pain, swelling, fistulas, mobility and intercanal pathology as needed for “success.”6,17 Success in both methods is often dependent on case selection, as well as the skill of the dentist, good fortune and the cooperation of the patient. A nonvital molar, with a large crack running through the crown, is less likely to be successfully treated than an intact, otherwise healthy, but recently exposed tooth, regardless of which treatment method is used.
The failure rate of traditional endo is varied: 5.3% are associated with significant pain17; 18% of treated teeth are eventually lost, with a relative rate of 2% being lost each year; 6% are reported lost in six years; and 50% are lost 30 years after treatment.2 Of traditional endodontic failures over the years, 60% fail due to prosthetic problems (e.g., tooth cracks, internal resorption), 32% fail due to periodontal concerns and 9% fail due to purely endodontic considerations.18 Generally speaking, between 74% and 86% of endodontically treated teeth are retained, even though they may have some radiographic signs of periapical abnormalities11,19 (Fig. 4).
Between 74% and 86% of endodontically treated teeth are retained, even though they may have some radiographic signs of periapical abnormalities.
The history of the pulpotomy presents a mixed collection of successes and failures. Pulpotomy for deciduous teeth are routine and dependable. The deciduous tooth, pretreated or not, responds well to pulpotomies and is required to last only a few years in the mouth before it is exfoliated (Fig. 10). Long-term pulpotomy success is not a consideration in deciduous teeth. Pulpotomies in permanent or adult teeth sometimes present failure because of fractured and leaking restorations. This is partially due to the expectation that a damaged/repaired tooth should last an ever-increasing lifetime. Another reason for past pulpotomy failures was an economic issue resulting in a weak restoration (e.g., amalgam) being placed in the treated tooth instead of a strong, but expensive crown. A large amalgam placed in a bombed-out tooth will often leak after a few years of wear. Recent reports have showed an increasing rate of success with adult pulpotomies, even for extended periods of time4,6,12,13,16 (Figs. 2, 7–9).
DeRosa has shown a 65% success rate of pulpotomies after eight years’ follow up.20 Aguilar did a meta-analysis of PubMed adult pulpotomy studies, finding a 73% to 99% success range over three years.13 Witherspoon described a 95% success rate for pulpotomies after 1.5 years.21 Barrieshi-Nusair reported a 90% success rate of pulpotomies after two years.22 Qudeimat presented a 92% success rate using CaOH pulpotomies after three years.4 Noorollahian demonstrated a 94% success rate after two years.23 Honegger reported in a study of 123 teeth an 83% success rate after seven years.24 These recent reports show adult tooth pulpotomies can have a success record approaching, if not surpassing, that of traditional endodontics.10,17,19
Pulpotomy Study
I did a study of 500 adult tooth pulpotomies over a six-year period. Patients were selected on two levels: 1) they had pulp exposures in restorable teeth, and 2) they were given the option of traditional endodontics, pulpotomy or extraction. Those who chose pulpotomy paid the same fee as an extraction and were offered a free extraction if the results of the pulpotomy were not to their liking. The patients were fully informed of the options and potential problems. Economics was the major factor in their decision.
The pulpotomy teeth were radiographed before treatment, and at six-month and two-year recall intervals. Only 302 patient pulpotomies returned for their two-year recall, making this, in reality, a study of 302 patients: the largest ever conducted to date. Semiannual checkups extended for most of the patients well into three years, after which time normal patient attrition reduced the numbers being followed on further visits. The longest patient pulpotomy followed was for 19 years. Success was measured by the asymptomatic condition of the tooth (no pain or mobility), and the absence of overt radiographic, intercanal or periapical pathology. Patients who experienced pulpotomy failure were encouraged to have the tooth retreated at no cost.
The pulpotomy consisted of air rotor access to the pulp, removal of the coronal pulp tissue and decay, placement of a cotton pellet with Buckley’s FC formula, and then restoration with a ZOE base and amalgam filling. In a few cases where the patient could afford it, a cast crown was placed. Patients with “hot” teeth were given antibiotics and pain medications prior to treatment. Average operative time was 30 minutes.
Here are the clinical results:
- 8% had some degree of pain and needed pain medications
- 8% had teeth that failed and were eventually extracted
- 25% had problems requiring repeat of the pulpotomy
- 68% had no problems
Over the two-plus years of this study, patients experienced 68% initial success. Most of the patients did well with their first pulpotomy. Another 25% experienced flare-ups and required an additional pulpotomy retreatment and new restoration. This was primarily due to large amalgam restorations cracking and allowing contaminants to enter the pulp chamber. Thus, 92% of the pulpotomies eventually succeeded, while 8% of the pulpotomies failed and resulted in extraction or further treatments using traditional endodontics. This degree of success is comparable to traditional endodontics.2,11,18,19,25
Problems
In the past, major difficulties with adult pulpotomies involved them being unpredictable in outcome and a bias, especially in North America, favoring traditional endo as a competing technique.1-3,25,26 Some pulpotomies present problems; often, a few years after treatment, the teeth may produce a static, periapical radiolucency on radiographs that is asymptomatic and seldom progresses25 (Fig. 8). Some clinicians consider this a failure, while others do not because the patient is comfortable, asymptomatic and functioning for years3-6,12-16 (Figs. 4, 9). Occasionally, cases of adult pulpotomy result in the tooth’s canals ossifying or exhibiting resorption, though this is also seen in traditional endodontic treatment.23,25,26 These complications make traditional endo, when attempted at a later time, more difficult. Such problems may be due to inadequate amounts of pulpotomy medication being used or the coronal seal (restoration) leaking, allowing the loss of the medication and leakage of microbes into the tooth.
There are theoretical concerns over the mutagenic effects of FC and other pulpotomy medications. Eugenol, glutaraldehyde, zinc oxide and silver points are also theoretically mutagens, however, and are used extensively in traditional endo.5,6,7 None of these agents have been associated with overt neoplastic changes in the real world because so little of the material is used in pulp therapy.5,6,7 They are perfectly safe.
When compared to the difficulty and the cost of traditional endodontics, pulpotomies excel. It only takes a few minutes to reopen a failing pulpotomy tooth, insert more pulpotomy medication (e.g., FC) and replace or patch the restoration (Fig. 11). What is needed is more research on the most efficient and dependable adult tooth pulpotomy techniques and medications. Though this need has been apparent for more than 50 years, little work has been done and there seems to be a sinister, ethical dilemma in play.
Are Endodontists Biased?
The endodontic specialty community controls endodontic research, including pulpotomy science. Compared to North American research involving traditional endo, adult pulpotomies research is, in comparison, minuscule and has been so for decades. An internet PubMed search produced 144 adult pulpotomy papers in the literature, most describing molar treatments in young adults. Those involving mature teeth were most-commonly published in predominately non-U.S. countries.4-6,12-17,20-22 In contrast, traditional endodontics has well over 10,000 articles recommending traditional endodontics.1,2,3 This is not a simple coincidence. There is a reason for this imbalance, and I believe it lies with the endodontic specialty. Endodontics, as practiced today, is a complex, expensive operation with 4,000-plus specialists devoting their entire practices to the subject. In this specialty, as well as in general practice, traditional endo is a very profitable procedure producing high fees for minimal, though demanding, work and materials. It is a cash cow, and many dentists milk it.
An internet PubMed search produced 144 adult pulpotomy papers in the literature, most describing molar treatments in young adults. … In contrast, traditional endodontics has well over 10,000 articles recommending traditional endodontics.
What would happen if a dependable, simple, quick and low-cost pulpotomy technique for adult teeth was promoted? It would, overnight, nullify the need for traditional endodontics and the people who practice it. GPs would do financially well because they could focus on restoring more teeth saved by the technique. Endodontists, unfortunately, would suffer greatly because their skills and service to the patient would be eclipsed. No one would want an expensive, time-consuming traditional endodontic treatment when they could have an inexpensive, quick, dip-a-pellet-in-the-pulp-chamber pulpotomy.
Not only would endodontic specialists economically suffer, but the endo equipment manufacturers, distributers, dealers, book publishers, journal editors (paid advertising), dental school programs, educators and so on would suffer the economic losses caused by universal use of adult pulpotomies and gradual marginalization of traditional endo. There are exceptions to this scenario, but they are in the minority.
In the real world, few people will willingly destroy their professions and livelihoods if they can help it, and the best way of protecting their turf is to isolate, denigrate and force adult pulpotomies to the margins of dentistry. It is the endodontists in dental school programs who write the textbooks, journal articles, approve the curriculum and teach the next generations of dentists. It is the endodontists who are most closely listened to (concerning endodontic matters) at professional meetings and the bureaucracies of many dental organizations.7,28 These are the people who advise the journal editors (as to what is an acceptable endo paper for the journals) and state boards of dentistry (licenses), and serve as expert witnesses in malpractice trials as to what “proper” treatment (e.g., endodontic standard of care) should be. There is a lot of money riding on the status quo of traditional endo and, though there are some exceptions, most dentists involved in traditional endodontics are biased concerning one technique: their favorite technique, which they have invested, perfected, espoused and taught over their lifetime.
I believe this bias is why so few pulpotomy articles are published or research encouraged. This is the present state of our profession. If you doubt this is or could be happening, study the 50-plus years of machinations surrounding the Angelo Sargenti endodontic technique (N2), where a paraformaldehyde-containing sealer (pulpotomy) is placed in the pulp chamber and roots of adult teeth.3,28 The technique is quick, easy and relatively inexpensive, popular in Europe, and there is some excellent scientific research supporting it.28 Many in the endodontic community have been somewhat less than candid and fair with the investigation and research of this competing technique.3,28 If it can happen to the Sargenti technique, it will also happen to other adult pulpotomy techniques.
How can pulpotomies withstand the pressure of traditional endodontics? Pulpotomy as a technique has three outstanding qualities that cause it to outshine other competing techniques: it is quick, easy to do and low in cost. In this economy, money talks the loudest. If an insurer, government bureaucrat or out-of-pocket patient can have a tooth treated for significantly less money (pulpotomy) than traditional endo (more cost), guess which technique will be approved and which will be rejected?
What Can We Do?
More clinical research must be done, and it will probably be the general dentists who will do it. Different pulpotomy techniques should be documented and followed for years, as longevity of the treatment is the most important issue. The dental societies, journal editors and dental school alumni must encourage this effort. Dental journal editors, especially, must seek out broad-minded reviewers/referees for endo-pulpotomy articles, not just dump them for review to a biased specialist. Dental school alumni should pressure their school’s endodontic departments to do more pulpotomy research and publish unbiased results. Dental society leaders must also be encouraged to support pulpotomy research.
In our practices, we should do more pulpotomies in cases where our patients would otherwise have the tooth extracted due to economic considerations. This is becoming easier to do because fewer patients can afford the alternative of traditional endo. Inform the patient of the options, negatives and benefits of this treatment. Many will leap at the chance to save their teeth without expensive endodontics. If the pulpotomy fails, there is no net loss because the tooth would already have been extracted. Retreatment is easy and usually effective. Price adult pulpotomies at reasonable levels so more people will choose them. Keep track of your cases and publish results when you can. I find that formocresol pulpotomies deliver excellent results and present no ethical problems if the patient is fully informed of the advantages and disadvantages. It is important that their cases be followed. Try it. The time is right.
We should do more pulpotomies in cases where our patients would otherwise have the tooth extracted due to economic considerations.
Summary
As the new economic realities continue to mold our healthcare system, traditional endodontic treatment is becoming the treatment of choice for only the rich and well-insured. The average patient, with limited financial resources, needs a way of preserving their cariously exposed adult teeth, and adult pulpotomies are the answer. A pulpotomy can preserve the tooth, eliminate pain and infection, and be done quickly, inexpensively and with minimal effort. It can save teeth, and new research demonstrates that it can be as effective as traditional endodontics. This service should be offered to our patients. It is the ethical thing to do.
Author’s note: With the exception of cropping (trimming), all images have not been digitally or otherwise edited or embellished by the author.
Dr. Ellis Neiburger is a general practitioner in Waukegan, Illinois. Contact him at 847-244-0292 or eneiburger@comcast.net.
References
- ^Seltzer S. Endodontology: biologic considerations in endodontic procedures. 2nd ed. Philadelphia: Lea & Febiger; 1988. p. 249-382.
- ^Torabinejad M, Walton RE. Endodontics: principles and practice. 4th ed. St. Louis: Saunders; 2009. p. 224-87.
- ^Ingle J, Bakland L. Endodontics. 4th ed. Philadelphia: Lea & Febiger; 1994. p. 26-30, 224-9.
- ^Qudeimat M, Barrieshi-Nusair KM, Owais Al. Calcium hydroxide vs mineral trioxide aggregates for partial pulpotomy of permanent molars with deep caries. Eur Arch Paediatr Dent. 2007 Jun;8(2):99-104.
- ^Cohen BI, Pagnillo MK, Musikant BL, Deutsch AS. Formaldehyde evaluation from endodontic materials. Oral Health. 1998 Dec;88(12):37-9.
- ^Asgary S, Ehsani S. Permanent molar pulpotomy with a new endodontic cement: A case series. J Conserv Dent. 2009 Jan;12(1):31-6.
- ^American Dental Association, Council on Dental Therapeutics. The use of root canal filling materials containing paraformaldehyde. 1986.
- ^Nasseh A. The evolution of endodontics. Inside Dentistry. 2011 Jun;7(6):88-9.
- ^Hugh CL, Walton RE, Facer SR. Evaluation of intracanal sealer distribution with 5 different obturation techniques. Quintessence Int. 2005 Oct;36(9):721-9.
- ^Lin LM, Rosenberg PA, Lin J. Do procedural errors cause endodontic treatment failure? J Am Dent Assoc. 2005 Feb;136(2):187-93.
- ^Hollanda AC, Estrela CR, Decurcio Dde A, Silva JA, Estrela C. Sealing ability of three commercial resin-based endodontic sealers. Gen Dent. 2009 July-Aug;57(4):368-73.
- ^Asgary S, Eghbal MJ. A clinical study of pulpotomy vs. root canal treatment of mature molars. J Dent Res. 2010 Oct;89(10):1080-5.
- ^Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod. 2011 May;37(5):581-7.
- ^Bjørndal L, et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs direct complete excavation, and direct pulp capping vs partial pulpotomy. Eur J Oral Science. 2010 Jun;118(3):290-7.
- ^Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009 Apr;35(1):4-8.
- ^Calişkan MK. Pulpotomy of carious vital teeth with periapical involvement. Int Endod J. 1995 May;28(3):172-6.
- ^Balto K. How common is tooth pain after root canal treatment? Evid Based Dent. 2010;11(4):114.
- ^Karabucak B, Setzer F. Criteria for the ideal treatment option for failed endodontics: surgical or nonsurgical? Compend Cont Educ Dent. 2007 Jun;28(6):304-10.
- ^Friedman S, Mor C. The success of endodontic therapy: healing and functionality. Oral Health. 2005 May:25-41.
- ^DeRosa TA. A retrospective evaluation of pulpotomy as an alternative to extraction. Gen Dent. 2006 Jan-Feb;54(1):37-40.
- ^Witherspoon DE, Small JC, Harris GZ. Mineral trioxide aggregate pulpotomies: a case series outcomes assessment. J Am Dent Assoc. 2006 May;137(5):610-8.
- ^Barrieshi-Nusair KM, Qudeimat MA. A prospective clinical study of mineral trioxide aggregate for partial pulpotomy in cariously exposed permanent teeth. J Endod. 2006 Aug;32(8):731-5.
- ^Noorollahian H. Comparison of mineral trioxide aggregate and formocresol as pulp medicaments for pulpotomies in primary molars. Br Dent J. 2008 Jun 14;204(11):E20.
- ^Honegger D, Holz J, Baume LJ. Long-term clinical supervision of direct pulp capping (performed by the students of the School of Dentistry, Geneva). SSO Schweiz Monatsschr Zahnheilkd. 1979 Oct;89(10):1020-41.
- ^Ward J. Vital pulp therapy in cariously exposed permanent teeth and its limitations. Aust Endod J. 2002 Apr;28(1):29-37.
- ^Weine FS. Endodontic therapy. 5th ed. St Louis: Mosby; 1996. p. 722-49.
- ^Zias J, Numeroff K. Ancient dentistry in the Eastern Mediterranean: a brief review. J Israel Exploration. 1986;36:65-7.
- ^Arzt A. Anti Sargenti research is flawed. J Am Endo Soc. 2011 Summer;124:4.
Copyright © 2011 by E. Neiburger.